Electrical injury
BMJ 2017; 357 doi: https://doi.org/10.1136/bmj.j1418 (Published 12 April 2017) Cite this as: BMJ 2017;357:j1418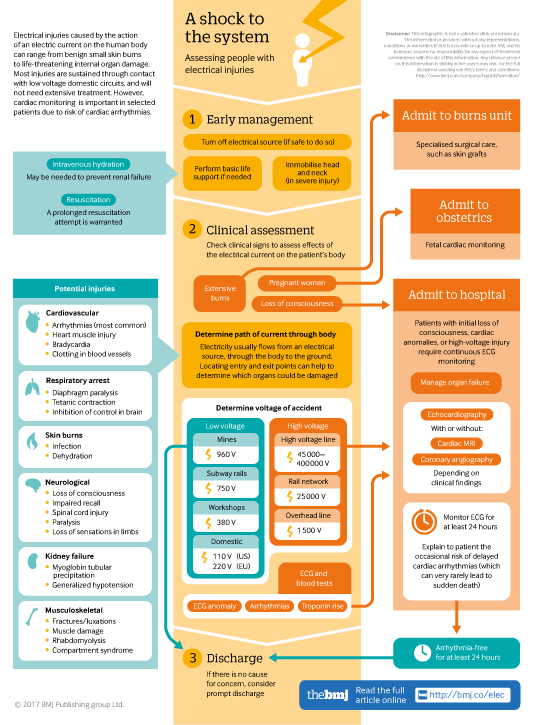
Infographic available
Click here for a visual overview of assessment for people with electrical injuries, including when to admit, and when people at low risk of complications can safely be discharged.
- Victor Waldmann, research fellow in cardiology1 2 3,
- Kumar Narayanan, consultant cardiologist, senior research associate3 4,
- Nicolas Combes, consultant cardiologist5,
- Eloi Marijon, cardiologist, associate professor of medicine1 2 3
- 1Cardiology Department, European Georges Pompidou Hospital, 20-40 rue Leblanc, 75908 Paris Cedex 15, France
- 2Paris Descartes University, Paris, France
- 3Paris Cardiovascular Research Center, Paris, France
- 4Cardiology Department, Maxcure Hospitals, Hyderabad, India
- 5Cardiology Department, Clinique Pasteur, Toulouse, France
- Correspondence to: E Marijon eloi_marijon{at}yahoo.fr
What you need to know
Electrical injuries are relatively uncommon but can be life threatening, causing extensive burns or internal organ damage
Wet skin can make otherwise be a minor injury more serious
Arrhythmias are the most common cardiac complication and may sometimes present late
Non-specific electrocardiographic (ECG) changes may be the only indicator of cardiac damage
Patients who have a normal ECG on admission after a low voltage injury with no loss of consciousness or initial cardiac arrest may be discharged home
Electrical injuries can range from small skin burns to life threatening internal organ damage. The most extreme form of electric shock, such as caused by a lightning strike, often results in instant death by electrocution. There is a lack of evidence regarding the management of patients after electrical accidents, which can cause concern for clinicians when these patients present.
This article discusses the main types of electrical injuries, their underlying pathophysiology, and practical issues relating to monitoring and treating seriously injured patients as well as those who are apparently well.
How common are electric shocks?
Many electrical accidents go unreported, so the true incidence is difficult to estimate. In the United States, the American Burn Association (www.ameriburn.org) estimates 4400 people are injured in electrical accidents and 400 others die from electrocutions each year, which are mostly work related (miners, electricians, and construction workers). Lightning strikes are responsible for up to 100 deaths a year.1 2 3
Of those admitted to US specialist burn units annually, 3-6% have had an electric shock.4 Many of the victims are young adults or adolescents, whose injuries often result from outdoor adventurous activities (such as climbing an electric pole, exploration of dangerous place as railway stations) and children involved in household accidents, mostly due to oral contact with electrical cords or cord sockets, contact with wall sockets directly (“finger in the socket”), or via a conducting foreign object (metal keys, pins, or cutlery).
How is the body affected after an electric shock?
Physiology
Electrical injuries affect the body in various ways. There are direct effects of current on body cells: for example, electric current can affect cell membranes, abruptly altering their electrical properties (cellular depolarisation) and causing direct cell injury by forming pores in cell membranes (electroporation) (fig 1⇓).
Fig 1 Diagram summarising main mechanisms of electrical current effects on cells and human body
Electric current also causes thermal injury due to conversion of electricity into heat as current passes through body tissues. Cellular and thermal injuries can be exacerbated by trauma sustained at the same time, such as a fall.
How to gauge likely severity
The severity of an electric shock depends on its intensity (current (I), measured in amperes) and the severity of burns is generally determined by the amount of energy delivered by the current (W, measured in joules) (box 1).
Box 1: What is an electric shock?
Electricity is a flow of electrons, measured in amperes (I), across a potential gradient from high to low concentration, expressed in voltage (V)
Ohm’s law (I = V/R) expresses the relation among voltage (V), current (I), and the impedance to electrical flow or resistance (R in ohms)
Joule’s law (W (Joules) = R × I2 × T) gives the heat energy produced as a result of current flow
The flow of current occurs from the entry point in contact with the electrical source to the exit point, which, in most instances, is in contact with the ground. Burns on the skin surface are often seen at the entry and exit points (fig 2⇓). Current generally takes the path of least resistance through tissues such as nerves and blood vessels. Voltage is the marker that is most often used for categorising electrical shocks as it is often the only variable known with certainty after exposure to electricity (boxes 2 and 3). The skin’s resistance to electricity can be reduced substantially by moisture, and so, when the skin is wet, what may otherwise be a minor injury with superficial tissue damage may be converted into a life threatening shock with extensive internal damage.5
Fig 2 (A) Finger skin burns at entry and exit points of electrical current (courtesy of Dr Kras, Centre Hospitalier de Martigues, France). (B) Severe foot burn after an electrical accident
Box 2: Main factors that determine the nature and severity of electrical trauma
Voltage (see box 3)
Resistance to current flow through the body
Type of current source (direct or alternating current)
Duration of contact with the current source
Path taken by the current through the body
Box 3: Main sources of electrical current, with associated voltage
High voltage
High voltage lines (45 000 to 400 000 V)
Rail network lines (25 000 V)
Overhead lines (1500 V)
Low voltage
Mines (960 V)
Subway electric rails (750 V)
Workshops (380 V)
Domestic supplies (US 110 V, Europe 220 V)
Effects on specific organ systems
Figure 3⇓ summarises the main types of organ-specific injuries after an electric shock. Cardiac effects are the most serious and among the most common electrical injuries. The heart is more commonly affected than other internal organs because electric current usually follows the path of lowest resistance in the body along blood vessels and nerves, directing the current towards the heart. Its central anatomical location in the chest also places it in harm’s way from currents passing both horizontally (hand to hand) and vertically (head to foot or hand to foot). Cardiac tissue vulnerability to potentially lethal arrhythmias when exposed to an external electric field sets it apart from other organs.19
Fig 3 Main types of organ-specific injuries after an electric shock
Fig 4 A 12-lead electrocardiogram and continuous Holter monitoring showing a huge transient QT interval prolongation (A) immediately after a high voltage electrical shock, associated with sinus tachycardia and premature ventricular extra beats (B) some hours later. The QT interval is the time between the start of the QRS complex and the end of the T wave. A lengthened QT interval indicates prolongation of electrical repolarisation, which can lead to ventricular arrhythmias. Corrected QT intervals (QTc) standards vary, but values greater than 460-480 ms are generally considered abnormal
How do I manage my patient after an electric shock?
The infographic suggests an approach to the assessment and management of electric shock based on currently available literature.20 21
The first step is to turn off the current source to prevent a further accident. Then, the management is mainly symptomatic. In witnessed accidents, a prompt and sometimes prolonged resuscitation attempt is warranted.22 Immediate resuscitation of patients in cardiac arrest from electrocution can result in long term survival, and complete recovery has been reported even after prolonged life support.20 23 Manage patients according to standard life support principles. Even when low blood pressure is not present, intravenous hydration is usually desirable to prevent kidney shut down. Adjust other aspects of management according the nature and severity of the injuries.
Discharge
Although only small studies have addressed this, all suggest that, in cases of low voltage injuries without any loss of consciousness or initial cardiac arrest, occurrence of serious arrhythmia is unlikely when electrocardiography at hospital admission is normal.7 24 25 Similar results have been reported with high voltage injuries, but more evidence is needed to support the safe discharge of these patients home.26 There are no established standards for the duration of monitoring after an electric shock, but 24 hours after admission or after resolution of arrhythmias is the most commonly adopted approach.
There is little data on the potential risks to an unborn baby after electrical shock to the mother during pregnancy, but it is recommended that both mother and fetus are monitored in hospital.27
In children no major differences in injury type or prognosis have been reported compared with adults, and so current guidelines on cardiac monitoring are the same.28
What to say to patients
If there is no substantial injury or electrocardiographic abnormality, reassure the patient that there is a low likelihood of any serious effect on his or her health
In the case of asymptomatic patients with non-specific electrocardiographic changes, explain that there is a need for a period of observation because of the occasional risk of delayed cardiac arrhythmias (which can rarely lead to sudden death). This involves electrocardiographic monitoring for at least 24 hours
In all patients, provide advice on prevention of future accidents
Education into practice
Are you comfortable with the management of an apparently healthy patient after electric shock?
Having read this article, what would you say to a patient with non-specific electrocardiographic changes after an electric shock who wants to be discharged home?
How patients were involved in the creation of this article
We obtained feedback on the article from three patients admitted to our hospital having had an electric shock. They provided input on whether the article was clear and gave information on the main risks and the right approach to adopt in situations involving electrical injury. Their suggestions to improve the article, such as to provide examples of electrical current sources with associated voltages, were then incorporated
Footnotes
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent obtained.




