- Medical Director of the Pain Management Center of Paducah, 2831 Lone Oak Road, Paducah, KY, 42003, and Clinical Professor, Anesthesiology and Perioperative Medicine, University of Louisville, Louisville, KY, USA
- Rehabilitation Medicine, New York University School of Medicine, New York, NY, USA
- Fourth Year Resident in Department of Physical Medicine and Rehabilitation at the University of Kentucky, Lexington, KY, USA
- Medical Director of Mid Atlantic Spine and Pain Physicians, Newark, DE, Pain Medicine Fellowship Program, Temple University Hospital, Philadelphia, PA, Department of PM and R, Temple University Medical School, Philadelphia, PA, USA
- Medical Director, Spine Pain Diagnostics Associates, Niagara, WI, USA
- Medical Director, Millennium Pain Center, Bloomington, IL, and Clinical Assistant Professor of Surgery, College of Medicine, University of Illinois, Urbana-Champaign, IL, USA
- Department of Anesthesia, LSU Health Science Center, New Orleans, LA, USA
- Interventional Pain Program, Professor and Director Pain Fellowship, Department of Orthopedics and Rehabilitation Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA
- Ohio Pain Clinic, Centerville, OH, USA
- Department of Anesthesia, Critical Care, and Pain Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA., USA
- 0President of Manhattan Spine and Pain Medicine, Department of Anesthesiology, NYU Langone-Hospital for Joint Diseases, NYU School of Medicine, New York, NY, USA
- 1Medical Director of Pain Medicine and Associate Professor of Anesthesiology and Orthopedics, Department of Anesthesiology, NYU Langone-Hospital for Joint Diseases, NYU School of Medicine, New York, NY, USA
- 2Department of Anesthesia, Critical Care, and Pain Medicine at Beth Israel Deaconess Medical Center, Boston, MA, and Assistant Professor of Anesthesiology at Harvard Medical School, Harvard Medical School, Boston, MA, USA
- 3Vice Chief of Interventional Care, Chief of Minimally Invasive Spine Surgery, Service Line Chief of Interventional Radiology, Director of Endovascular Neurosurgery and Neuroendovascular Program, Massachusetts General Hospital; and Associate Professor, Department of Radiology, Harvard Medical School, Boston, MA, USA
Correspondence Address:
Laxmaiah Manchikanti
3Vice Chief of Interventional Care, Chief of Minimally Invasive Spine Surgery, Service Line Chief of Interventional Radiology, Director of Endovascular Neurosurgery and Neuroendovascular Program, Massachusetts General Hospital; and Associate Professor, Department of Radiology, Harvard Medical School, Boston, MA, USA
DOI:10.4103/2152-7806.156598
Copyright: © 2015 Manchikanti L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Manchikanti L, Nampiaparampil DE, Manchikanti KN, Falco FJ, Singh V, Benyamin RM, Kaye AD, Sehgal N, Soin A, Simopoulos TT, Bakshi S, Gharibo CG, Gilligan CJ, Hirsch JA. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: A systematic review of randomized controlled trials. Surg Neurol Int 07-May-2015;6:
How to cite this URL: Manchikanti L, Nampiaparampil DE, Manchikanti KN, Falco FJ, Singh V, Benyamin RM, Kaye AD, Sehgal N, Soin A, Simopoulos TT, Bakshi S, Gharibo CG, Gilligan CJ, Hirsch JA. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: A systematic review of randomized controlled trials. Surg Neurol Int 07-May-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/comparison-efficacy-saline-local-anesthetics/
Abstract
Background:The efficacy of epidural and facet joint injections has been assessed utilizing multiple solutions including saline, local anesthetic, steroids, and others. The responses to these various solutions have been variable and have not been systematically assessed with long-term follow-ups.
Methods:Randomized trials utilizing a true active control design were included. The primary outcome measure was pain relief and the secondary outcome measure was functional improvement. The quality of each individual article was assessed by Cochrane review criteria, as well as the criteria developed by the American Society of Interventional Pain Physicians (ASIPP) for assessing interventional techniques. An evidence analysis was conducted based on the qualitative level of evidence (Level I to IV).
Results:A total of 31 trials met the inclusion criteria. There was Level I evidence that local anesthetic with steroids was effective in managing chronic spinal pain based on multiple high-quality randomized controlled trials. The evidence also showed that local anesthetic with steroids and local anesthetic alone were equally effective except in disc herniation, where the superiority of local anesthetic with steroids was demonstrated over local anesthetic alone.
Conclusion:This systematic review showed equal efficacy for local anesthetic with steroids and local anesthetic alone in multiple spinal conditions except for disc herniation where the superiority of local anesthetic with steroids was seen over local anesthetic alone.
Keywords: Chronic pain, epidural injections, facet joint injections, local anesthetic, spinal pain, steroids, saline
INTRODUCTION
The increasing prevalence of spinal pain and disability, and the explosion of health care costs are major issues for the US and the world.[
Martin et al.[
In another manuscript, Manchikanti et al.[
Epidural injections are used in managing spinal pain secondary to disc herniation, spinal stenosis, postsurgery syndrome, discogenic pain not from facet or sacroiliac joints, and multiple other conditions.[
The response to epidural injections is variable for various pathologies including disc herniation and/or radiculitis, discogenic pain without disc herniation, spinal stenosis, and postsurgery syndrome. Manchikanti et al.,[
Steroids and local anesthetics have multiple mechanisms of action when injected into the epidural space; antiinflammatory effects are predominantly seen with steroids and other effects are seen with local anesthetics.[
This systematic review assesses randomized controlled trials of epidural and facet joint injections utilizing saline, local anesthetic, and/or steroids. The objective of this review is to characterize the role of saline and local anesthetic in these procedures and to compare their effects to those of steroids in the long-term.
METHODS
The methodology for this systematic review was derived from evidence-based systematic reviews and meta-analyses of randomized trials.[
Only randomized trials utilizing a true active control design with injection of either sodium chloride solution or local anesthetic or steroid into the epidural space, on the nerve root, in the joint, or facet joint nerves were included. True placebo injections, that is, injections of inactive solutions into inactive structures, were not included.
In active control trials, two different procedures or drugs are compared. For this assessment, only the trials comparing sodium chloride solution, local anesthetic, or steroids were utilized. The rationale for assessing only the aforementioned agents is that they are the most clinically relevant medications. Further, trials where a drug was injected outside the epidural space, nerve root, or joint were excluded. This evidence will address the misconception concerning local anesthetic as a placebo or even sodium chloride solution as a pure placebo.
The interventions evaluated were caudal and interlaminar epidural injections in the cervical, thoracic, and lumbar regions; transforaminal epidural injections in the cervical, thoracic, and lumbar regions; and facet joint injections and nerve blocks in the cervical, thoracic, and lumbar regions.
The primary outcome measure was pain relief; the secondary outcome measure was functional improvement. A literature search was performed from various resources including PubMed, the Cochrane Library, the US National Guideline Clearinghouse (NGC), previous systematic reviews, and cross references.
The search period covered from 1966 through March 2014.
The search strategy emphasized chronic neck, thoracic, low back, and upper extremity pain; lower extremity pain; and chest wall pain treated with epidural or facet joint interventions. Search terms were:
(Chronic low back pain or chronic back pain or chronic neck pain or disc herniation or discogenic pain or facet joint pain or herniated lumbar discs or nerve root compression or lumbosciatic pain or postlaminectomy or lumbar surgery syndrome or radicular pain or radiculitis or sciatica or spinal fibrosis or spinal stenosis or zygapophyseal) and (epidural injection or epidural steroid or epidural perineural injection or interlaminar epidural or intraarticular corticosteroid or nerve root blocks or intraarticular injection or periradicular infiltration or saline injection or transforaminal injection or corticosteroid or methylprednisolone or facet joint or medial branch block); Sort by: Publication Date; Filters: Clinical Trial, Controlled Clinical Trial, Evaluation Studies, Multicenter Study, Randomized Controlled Trial, Validation Studies, Comparative Study.
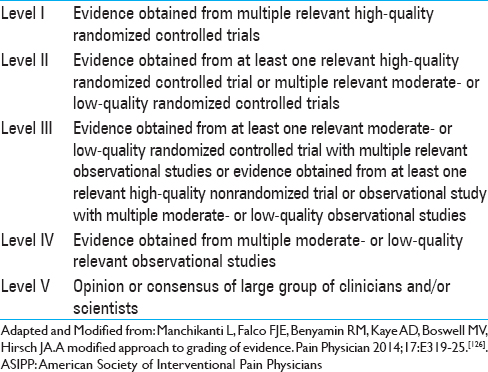
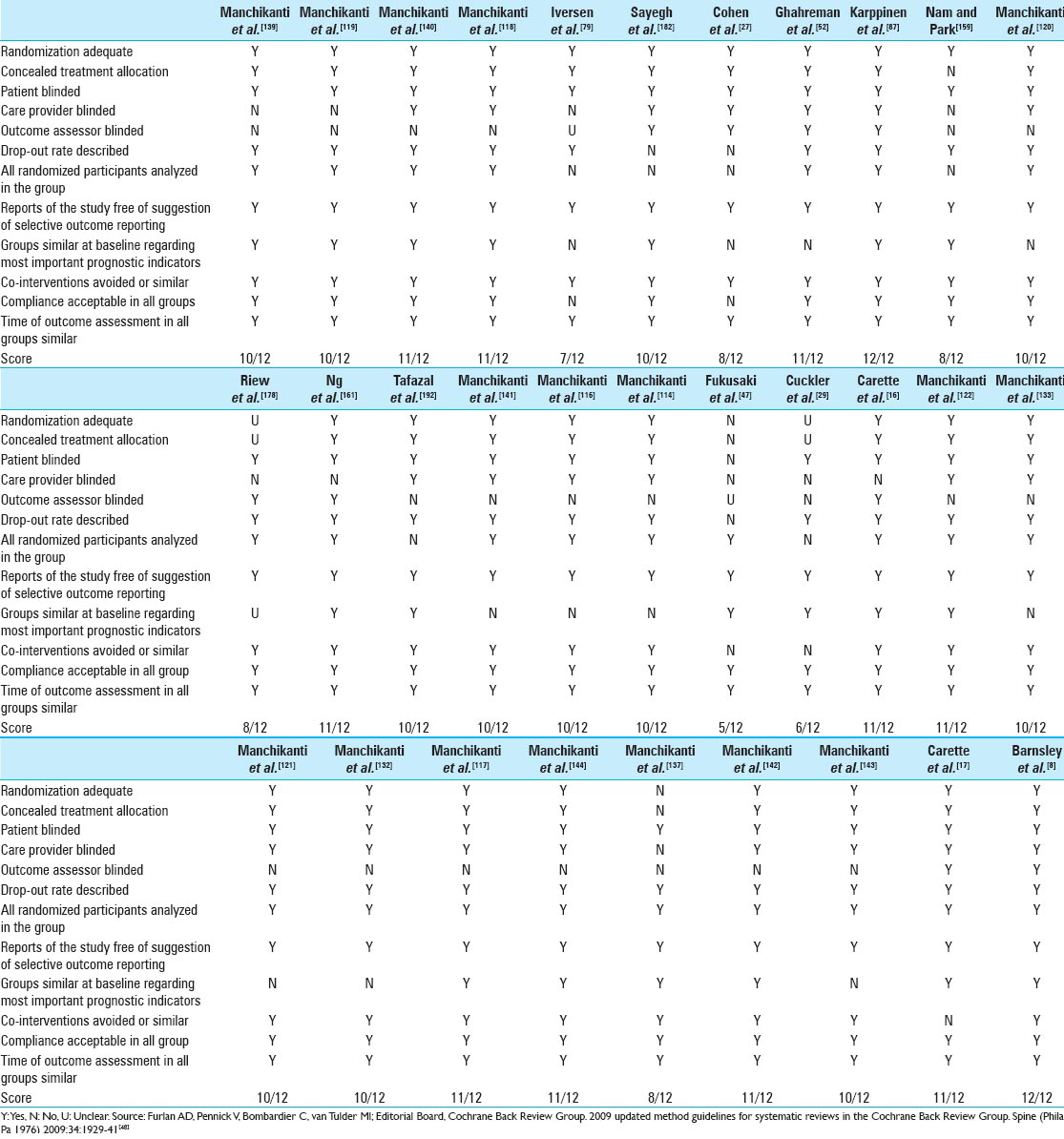
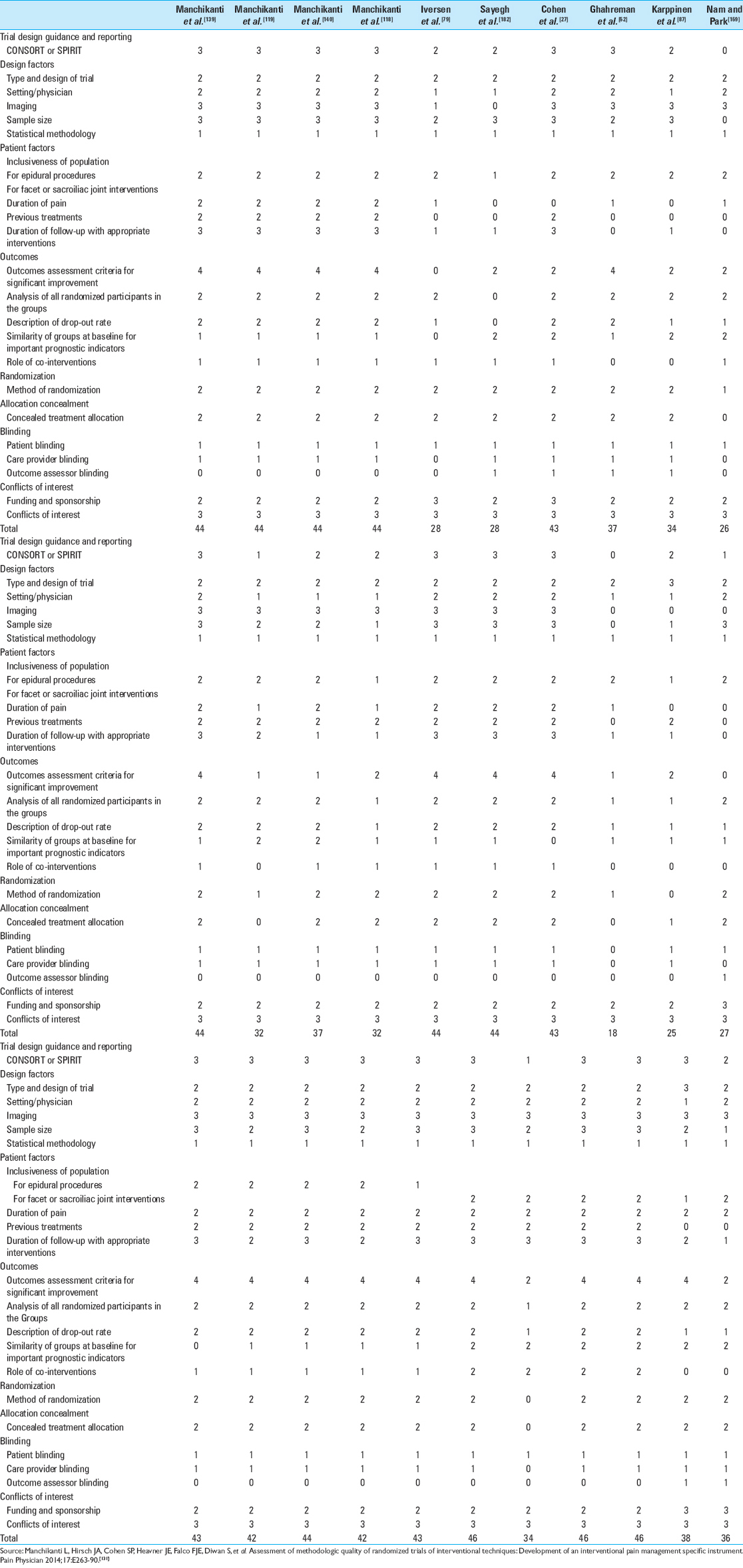
The quality of each individual article was assessed for bias using Cochrane review criteria [
The literature search, selection of trials, and methodological quality assessment were performed by at least two authors for each task. The allocation of trials for methodological quality assessment was distributed among the authors. Any discrepancies were resolved by consensus and the primary (LM) and senior (JH) authors.
Trials scoring 8–12 on Cochrane review criteria or 32–48 on ASIPP criteria were considered high quality, trials scoring 4–7 on Cochrane review criteria or 20–31 on ASIPP criteria were considered moderate quality, and studies scoring less than 4 on Cochrane review criteria or less than 20 on ASIPP criteria were considered low quality.
A meta-analysis was conducted if there were more than two trials that were condition-specific and homogeneous.
Analysis of the evidence was based on the condition, region, and modality (e.g. lumbar disc herniation, cervical spinal stenosis, or thoracic facet joint arthritis) so as to reduce any clinical heterogeneity.
The summary measure for pain was a 50% or more reduction of pain in at least 50% of the patients, or at least a 3-point decrease in pain scores; for disability scores the summary measure was a 50% or more reduction in disability in at least 40% of the patients or at least a 30-point decrease in disability scores measured on a scale of 0–100.
The analysis of evidence was conducted based on the qualitative level of evidence criteria synthesized by ASIPP[
RESULTS
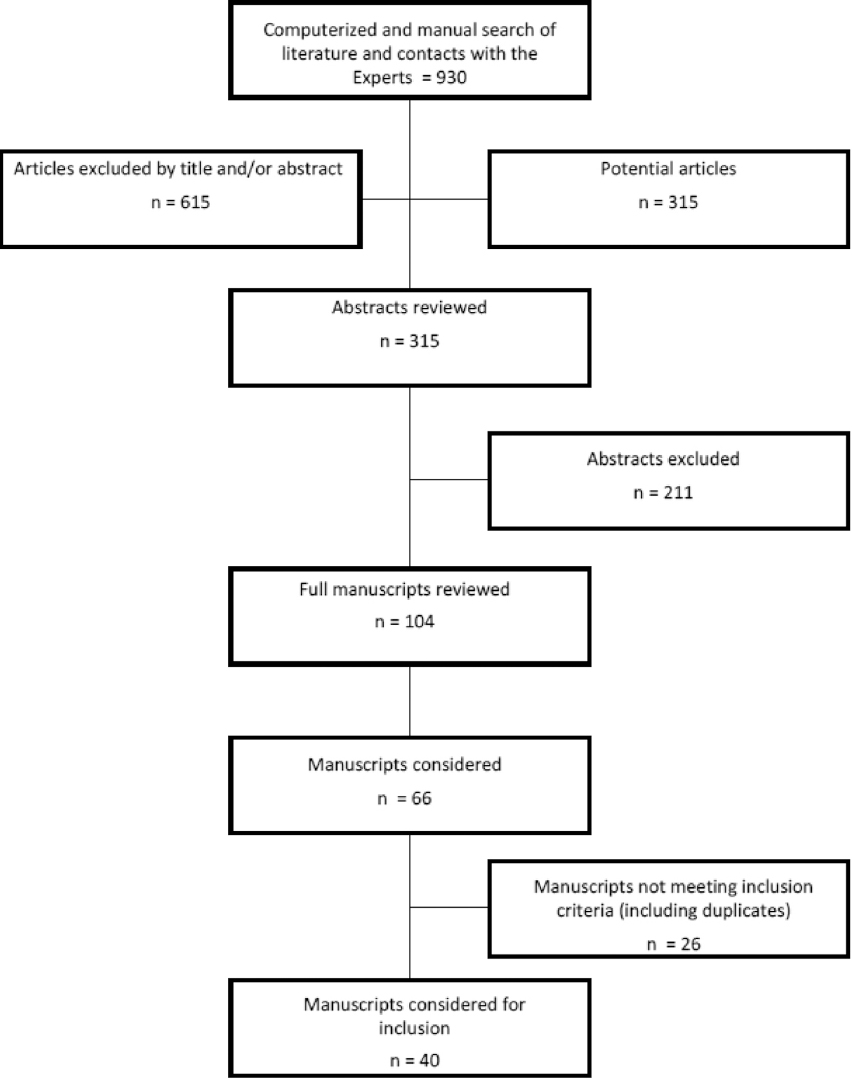
The literature search and study selection is shown in
Meta-analysis
There was no homogeneity among the 31 trials meeting the inclusion criteria for methodological quality assessment when the region, technique, solutions injected, and use of fluoroscopy were considered. Of the 31 trials, 13 trials by Manchikanti et al. assessing the role of epidural injections were similar in many aspects;[
Study characteristics
Study characteristics and outcomes are described in
Caudal epidural injections
Among those trials meeting the inclusion criteria, there were six examining the efficacy of caudal epidural injections with multiple solutions.[
Four of these studies were conducted by Manchikanti et al.[
All four trials showed similar results for the efficacy of caudal epidural injections with local anesthetic alone or local anesthetic with steroids in 50–80% of the patients. In these trials, success was defined as at least 3 weeks of significant improvement (50% improvement) in pain and function after the first two injections. All patients were grouped into successful (responsive) or nonresponsive categories accordingly. We then calculated the number of patients with disc herniation, discogenic pain, spinal stenosis, or postsurgery syndrome who were nonresponsive to local anesthetic alone or local anesthetic with steroid. We observed no significant differences in the patients who did not respond to either injection for any of the spinal conditions. This suggests that none of the spinal conditions influenced the response to either type of injection.
The study by Sayegh et al.[
Iversen et al.,[
In conclusion, there was Level I evidence supported by multiple, relevant high-quality randomized controlled trials[
There was also Level I evidence, based on multiple, relevant high-quality randomized controlled trials,[
Lumbar transforaminal epidural injections
There were eight randomized controlled trials assessing the efficacy of multiple solutions used in lumbar transforaminal administration.[
Cohen et al.,[
Ghahreman et al.,[
In a large trial, Karppinen et al.[
Nam and Park[
Manchikanti et al.,[
Riew et al.,[
Ng et al.[
Tafazal et al.[
There was Level I evidence, based on multiple, relevant high-quality randomized controlled trials,[
There was Level II evidence, based on one high-quality trial, that local anesthetics with steroids are superior to local anesthetic alone in avoiding surgery (33% vs 71%),[
Lumbar interlaminar epidural injections
There were six randomized controlled trials assessing the efficacy of multiple solutions used in lumbar interlaminar epidurals.[
Three of these studies were conducted by Manchikanti et al.[
In these manuscripts, the study subcategories were identified as responsive and nonresponsive groups. The responsive groups consisted of patients who received at least 3 weeks of significant improvement (50% improvement) in pain and function with the first two procedures. The number of patients in the nonresponsive category who received interlaminar epidural injections of local anesthetic only included 10 who had disc herniation, five who had discogenic pain, and nine patients who had central stenosis. In the corresponding nonresponsive local anesthetic with steroids category, the number of patients were: One who had disc herniation, six who had discogenic pain, and seven who had central stenosis. Thus, there was a high proportion of patients in the disc herniation group who were nonresponsive to lumbar interlaminar injections of local anesthetic, while there were no differences noted in the central stenosis or the discogenic pain groups compared with the corresponding responsive patients. In addition, in disc herniation, lumbar interlaminar epidural injections have somewhat superior results for pain relief at 6 months, and functional status at 12 months as observed in the local anesthetic with steroid group.[
Among the other trials, Fukusaki et al.[
Carette et al.,[
Based on multiple high-quality randomized trials[
Cervical interlaminar epidural injections
Among the trials meeting inclusion criteria, there were four high-quality trials[
All studies were conducted by Manchikanti et al.[
Based on multiple, high-quality relevant randomized trials,[
Thoracic interlaminar epidural injections
There was only one trial assessing thoracic interlaminar epidural injections. It was conducted by Manchikanti et al.,[
Manchikanti et al.,[
There was Level II evidence based on one high-quality randomized trial[
Facet joint interventions
Lumbar, cervical, and thoracic facet joint nerve blocks and cervical and lumbar intraarticular injections have been studied with saline, local anesthetic, and steroids. There were six randomized controlled trials assessing the efficacy of facet joint interventions with multiple solutions.[
Facet joint nerve blocks
Among the trials assessing facet joint nerve blocks, three of them included a 2-year follow-up, active control design, and appropriate outcome parameters.[
Based on the results of this assessment, these four trials, considered to be high-quality based on Cochrane review criteria and IPM-QRB criteria,[
Facet joint injections
There was one randomized controlled trial by Carette et al.[
Thus, there was Level I evidence for the lack of effectiveness for intraarticular injections based on two high-quality randomized controlled trials.[
Efficacy of epidural injections in specific spinal conditions
Disc herniation
Disc herniation has been treated with caudal, lumbar interlaminar, lumbar transforaminal, thoracic interlaminar, and cervical interlaminar epidural injections. There was no identifiable evidence from randomized controlled trials for either cervical transforaminal epidural injections or thoracic transforaminal epidural injections in treating disc herniation.
There were 15 trials assessing the role of epidural injections in disc herniation,[
Of the three caudal epidural injection trials, one trial[
All seven randomized controlled trials[
Of the three lumbar interlaminar epidural trials,[
There was Level I evidence, based on multiple, relevant high-quality randomized trials,[
In addition to the above, the level of evidence for each vertebral region was variable. There was Level I evidence for caudal, lumbar interlaminar, and lumbar transforaminal injections in managing lumbar disc herniation, with multiple high quality randomized controlled trials. There was also superiority for steroids in managing disc herniation in the lumbosacral region compared with local anesthetic alone in assessments up to one year with caudal and interlaminar epidural injections.
However, there was Level II evidence for managing cervical disc herniation and thoracic disc herniation based on at least one high-quality randomized controlled trial in each category.
Spinal stenosis
Caudal, lumbar interlaminar, lumbar transforaminal, thoracic interlaminar, and cervical interlaminar epidural injections have been utilized in treating pain from central spinal stenosis. There are no randomized controlled trials assessing the role of cervical or thoracic transforaminal epidural injections in managing pain of central spinal stenosis. There were seven trials assessing the role of epidural injections in central spinal stenosis,[
The caudal epidural injection trial was high quality.[
There was Level I evidence, based on relevant high-quality trials,[
There was Level II evidence in managing lumbar central spinal stenosis based on caudal and lumbar interlaminar trials, whereas there was also Level I evidence in managing cervical central spinal stenosis based on one randomized controlled trial, whereas there was no evidence available in managing thoracic spinal stenosis.
Discogenic pain
Discogenic pain has been treated with caudal, lumbar interlaminar, thoracic interlaminar, and cervical interlaminar epidural injections. There are no studies assessing the role of transforaminal epidural injections for discogenic pain.
There were three trials assessing the role of epidural injections in discogenic pain without disc herniation, radiculitis, or facet joint pain;[
There was Level I evidence, based on multiple high-quality relevant randomized controlled trials,[
There was Level II evidence based on two randomized controlled trials in managing discogenic pain with caudal and lumbar interlaminar epidural injections, with Level II evidence in managing cervical and thoracic discogenic pain, with one high-quality randomized controlled trial in each category.
Postsurgery syndrome
Postsurgery syndrome has been treated with caudal, lumbar transforaminal, thoracic interlaminar, and cervical interlaminar epidural injections. There were no studies assessing the role of lumbar interlaminar or transforaminal epidural injections.
There was only one randomized caudal epidural injection trial[
There was Level II evidence, based on the two high-quality, relevant randomized controlled trials,[
There was Level II evidence in managing lumbar postsurgery syndrome with caudal epidural injections and cervical postsurgery syndrome with cervical interlaminar epidural injections, with no evidence available for thoracic postsurgery syndrome.
DISCUSSION
In this assessment of the efficacy of various solutions injected into the spinal epidural space and over the facet joint nerves, there was Level I evidence that local anesthetics with steroids and local anesthetics or steroids administered in combination or separately were equally effective based on multiple, relevant, high-quality randomized controlled trials of spinal pain from various origins. However, for intraarticular injection, the evidence of lack of effectiveness was Level I for injections of sodium chloride solution, local anesthetic, or local anesthetic with steroids. There was also Level II evidence for the superiority of local anesthetic with steroids compared with steroids alone in managing disc herniation and Level IV evidence in spinal stenosis.
In recent years, there has been much debate in reference to interventional techniques in general, and epidural injections of steroids in particular, with catastrophic complications related to transforaminal epidural steroid injections, specifically in the cervical and thoracic spine.[
The findings of this systematic review, showing the equal effectiveness of local anesthetics alone and local anesthetics with steroid administered into the epidural space, facet joints, or over facet joint nerves, is in contrast to a long-held philosophy and belief in the medical community concerning the effectiveness of steroids in treating spinal pain based on the theory of spinal pain having an inflammatory component. The results of this study are valid as only high-quality, randomized controlled trials were utilized. Further, the grading of the evidence was based on a best-evidence synthesis utilizing a strict approach for methodological quality assessment. The long-term follow-up of one year or longer was utilized in arriving at the conclusions rather than short-term follow-up of 1, 3, 6, or even 12 weeks, etc., In fact, the results are similar to the Bicket et al.[
The findings of this systematic review may be explained by various mechanisms of steroids and local anesthetics, including the suppression of ectopic discharges from inflamed nerves, enhancing blood flow to ischemic nerve roots, the lysing of iatrogenic and inflammatory adhesions, a washout of proinflammatory cytokines, and reversal of peripheral and central sensitization.[
Noteworthy as well is that investigators may be missing the role of the nocebo effect. The implications of these results may be significant in not only designing clinical trials, but also in managing patients. Further, it is essential to understand the differences between chronic and subacute pain. Many of the studies included subacute or acute patients, leading to erroneous conclusions. In this evaluation, we also included some trials that included subacute patients; however, they were followed long-term.[
Based on this evaluation as well as the Bicket et al.[
However, these results should be interpreted in the context of their multiple limitations. Based on the results, an abundant amount of steroids is not advised. As explained, there was no meta-analysis performed. The majority of the high-quality, randomized trials included in this analysis were from one group of investigators. Consequently, further trials are essential. At present, this evidence suggests physicians carefully select patients and take the opportunity to discuss with them shared decision-making concerning the equal efficacy of local anesthetic with or without steroids in multiple conditions. Steroids with local anesthetic appear to have some superiority, even though it is derived from a low level of evidence, over local anesthetics alone in managing disc herniation.
CONCLUSION
This systematic review shows a lack of effectiveness for saline and equal effectiveness for local anesthetic alone and local anesthetic with steroids in multiple, high-quality randomized controlled trials for epidural injections for managing spinal pain in various regions for various pathologies and facet joint nerve blocks in managing facet joint pain. The results also showed the superiority of epidural steroid injections with local anesthetic over local anesthetics alone for disc herniation.
ACKNOWLEDGMENTS
The authors wish to thank Vidyasagar Pampati, MSc, for statistical assistance; Tom Prigge, MA, and Laurie Swick, BS, for manuscript review; and Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in preparation of this manuscript.
References
1. Abbott ZI, Nair KV, Allen RR, Akuthota VR. Utilization characteristics of spinal interventions. Spine J. 2012. 12: 35-43
2. Akkaya T, Sayin M. Transforaminal epidural steroid injection and its complications. Agri. 2005. 17: 27-39
3. Alimasi W, Sawaji Y, Endo K, Yorifuji M, Suzuki H, Kosaka T. Regulation of nerve growth factor by anti-inflammatory drugs, a steroid, and a selective cyclooxygenase 2 inhibitor in human intervertebral disc cells stimulated with interleukin-1. Spine (Phila Pa 1976). 2013. 38: 1466-72
4. Al-Shoha A, Rao DS, Schilling J, Peterson E, Mandel S. Effect of epidural steroid injection on bone mineral density and markers of bone turnover in postmenopausal women. Spine (Phila Pa 1976). 2012. 37: E1567-71
5. Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: The WEST study. Rheumatology (Oxford). 2005. 44: 1399-406
6. Arner S, Lindblom U, Meyerson BA, Molander C. Prolonged relief of neuralgia after regional anesthetic block. A call for further experimental and systematic clinical studies. Pain. 1990. 43: 287-97
7. Atluri S, Glaser SE, Shah RV, Sudarsha G. Needle position analysis in cases of paralysis from transforaminal epidurals: Consider alternative approaches to traditional techniques. Pain Physician. 2013. 16: 321-34
8. Barnsley L, Lord SM, Wallis BJ, Bogduk N. Lack of effect of intraarticular corticosteroids for chronic pain in the cervical zygapophyseal joints. N Engl J Med. 1994. 330: 1047-50
9. Benyamin RM, Manchikanti L, Parr AT, Diwan SA, Singh V, Falco FJE. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012. 15: E363-404
10. Bhatia MT, Parikh LCJ. Epidural saline therapy in lumbo-sciatic syndrome. J Indian Med Assoc. 1966. 47: 537-42
11. Bhushan A, Leigh JP. National trends in occupational injuries before and after 1992 and predictors of workers’ compensation costs. Public Health Rep. 2011. 126: 625-34
12. Bicket M, Gupta A, Brown CH, Cohen SP. Epidural injections for spinal pain: A systematic review and meta-analysis evaluating the “control” injections in randomized controlled trials. Anesthesiology. 2013. 119: 907-31
13. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000. 81: 1045-50
14. Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine (Phila Pa 1976). 1999. 24: 1813-9
15. Last accessed on 2015 Jan 27. Available from: http://canadiantaskforce.ca/wp-content/uploads/2014/03/Procedure-Manual-2014-v2-0FINAL.pdf/?414ed1 .
16. Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997. 336: 1634-40
17. Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991. 325: 1002-7
18. Cassidy JD, Carroll LJ, Côté P. The Saskatchewan Health and Back Pain Survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998. 23: 1860-7
19. Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand. 2006. 50: 265-82
20. Cathelin MF. Mode d’action de la cocaine injecte daus l’escape epidural par le procede du canal sacre. Comptes Rendues des Seances de la Societe de Biologie et de ses Filliales (Paris). 1901. 43: 487-
21. Cecchi F, Debolini P, Lova RM, Macchi C, Bandinelli S, Bartali B. Epidemiology of back pain in a representative cohort of Italian persons 65 years of age and older: The InCHIANTI study. Spine (Phila Pa 1976). 2006. 31: 1149-55
22. . CGS Administrators, LLC. LCD for Pain Management (L31845). p.
23. Chiller TM, Roy M, Nguyen D, Guh A, Malani AN, Latham R. Clinical findings for fungal infections caused by methylprednisolone injections. N Engl J Med. 2013. 4: 1610-9
24. Last accessed on 2015 Jan 27. Available from: http://www.americanpainsociety.org/uploads/pdfs/LBPEvidRev.pdf .
25. Civelek E, Cansever T, Kabatas S, Kircelli A, Yilmaz C, Musluman M. Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain. Turk Neurosurg. 2012. 22: 200-6
26. Cohen SP, Bicket MC. In Reply. Anesthesiology. 2014. 120: 1284-5
27. Cohen SP, White RL, Kurihara C, Larkin TM, Chang A, Griffith SR. Epidural steroids, etanercept, or saline in subacute sciatica: A multicenter, randomized trial. Ann Intern Med. 2012. 156: 551-9
28. Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998. 23: 1689-98
29. Cuckler JM, Bernini PA, Wiesel SW, Booth RE, Rothman RH, Pickens GT. The use of epidural steroid in the treatment of radicular pain. J Bone Joint Surg. 1985. 67: 63-6
30. Cui W, Li Y, Li S, Wang R, Li J. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil based anaesthesia. Eur J Anaesthesiol. 2010. 27: 41-6
31. Culling RD, Rice JH. Corticosteroid injections for chronic low back pain. N Engl J Med. 1992. 326: 834-
32. Cyriax JH. Epidural anesthesia and bedrest in sciatica. Br Med J. 1961. 1: 20-4
33. Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005. 30: 1441-5
34. Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006. 443: 139-46
35. Dilke TF, Burry HC, Grahame R. Extradural corticosteroid injection in the management of lumbar nerve root compression. Br Med J. 1973. 2: 635-7
36. Diwan SA, Manchikanti L, Benyamin RM, Bryce DA, Geffert S, Hameed H. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician. 2012. 15: E405-34
37. Dooley JF, McBroom RJ, Taguchi T, Macnab I. Nerve root infiltration in the diagnosis of radicular pain. Spine (Phila Pa 1976). 1988. 13: 79-83
38. Engel AJ, Kennedy DJ, Macvicar J, Bogduk N. Not all injections are the same. Anesthesiology. 2014. 120: 1282-3
39. Eriksen J, Ekholm O, Sjøgren P, Rasmussen NK. Development of and recovery from long-term pain. A 6-year follow-up study of a cross-section of the adult Danish population. Pain. 2004. 108: 154-62
40. Evans W. Intrasacral epidural injection in the treatment of sciatica. Lancet. 1930. 2: 1225-9
41. Even JL, Crosby CG, Song Y, McGirt MJ, Devin CJ. Effects of epidural steroid injections on blood glucose levels in patients with diabetes mellitus. Spine (Phila Pa 1976). 2012. 37: E46-50
42. Everett CR, Baskin MN, Speech D, Novoseletsky D, Patel R. Flushing as a side effect following lumbar transforaminal epidural steroid injection. Pain Physician. 2004. 7: 427-9
43. Falco FJ, Manchikanti L, Datta S, Sehgal N, Geffert S, Onyewu O. An update of the effectiveness of therapeutic lumbar facet joint interventions. Pain Physician. 2012. 15: E909-53
44. Falco FJ, Manchikanti L, Datta S, Wargo BW, Geffert S, Bryce DA. Systematic review of therapeutic effectiveness of cervical facet joint interventions: An update. Pain Physician. 2012. 15: E839-68
45. Fernández-de-Las-Peñas C, Alonso-Blanco C, Hernández-Barrera V, Palacios-Ceña D, Jiménez-García R, Carrasco-Garrido P. Has the prevalence of neck pain and low back pain changed over the last 5 years? A population-based national study in Spain. Spine J. 2013. 13: 1069-76
46. Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS. The rising prevalence of chronic low back pain. Arch Intern Med. 2009. 169: 251-8
47. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998. 14: 148-51
48. Furlan AD, Pennick V, Bombardier C, van Tulder M. Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009. 34: 1929-41
49. Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012. 13: 715-24
50. Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: A randomized double-blind placebo controlled trial. Pain Physician. 2013. 16: 185-96
51. Ghahreman A, Bogduk N. Predictors of a favorable response to transforaminal injection of steroids in patients with lumbar radicular pain due to disc herniation. Pain Med. 2011. 12: 871-9
52. Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010. 11: 1149-68
53. Ghanei I, Rosengren BE, Hasserius R, Nilsson JÅ, Mellström D, Ohlsson C. The prevalence and severity of low back pain and associated symptoms in 3,009 old men. Eur Spine J. 2014. 23: 814-20
54. Gillies JH, Ward JH, Griesdale DE. Corticosteroid injections for sciatica. N Engl J Med. 1997. 337: 1242-
55. Glaser SE, Falco FJ. Paraplegia following a thoracolumbar transforaminal epidural steroid injection. Pain Physician. 2005. 8: 309-14
56. Glaser SE, Shah RV. Root cause analysis of paraplegia following transforaminal epidural steroid injections: The “unsafe” triangle. Pain Physician. 2010. 13: 237-44
57. Gostine M. Corticosteroid injections for chronic low back pain. N Engl J Med. 1992. 326: 834-5
58. Grigoras A, Lee P, Sattar F, Shorten G. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain. 2012. 28: 567-72
59. Gunal I, Karatosun V. Avascular necrosis of the femoral heads after single corticosteroid injection. CMAJ. 2006. 175: 31-
60. Gupta AK, Mital VK, Azmi RU. Observations of the management of lumbosciatic syndromes (sciatica) by epidural saline. J Indian Med Assoc. 1970. 54: 194-6
61. Gupta S, Ward S, Munglani R, Sharma M, Lversen T. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011. 343: d5278-
62. Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B. Grading strength of recommendations and quality of evidence in clinical guidelines. Report from an American College of Chest Physicians task force. Chest. 2006. 129: 174-81
63. Hansen H, Manchikanti L, Simopoulous TT, Christo PJ, Gupta S, Smith HS. A systematic evaluation of the therapeutic effectiveness of sacroiliac joint interventions. Pain Physician. 2012. 15: E247-78
64. Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM. Current methods of the US Preventive Services Task Force. Am J Prevent Med. 2001. 20: 21-35
65. Häuser W, Bartram C, Bartram-Wunn E, Tölle T. Adverse events attributable to nocebo in randomized controlled drug trials in fibromyalgia syndrome and painful diabetic peripheral neuropathy: Systematic review. Clin J Pain. 2012. 28: 437-51
66. Hayashi N, Weinstein JN, Meller ST, Lee HM, Spratt KF, Gebhart GF. The effect of epidural injection of betamethasone or bupivacaine in a rat model of lumbar radiculopathy. Spine (Phila Pa 1976). 1998. 23: 877-85
67. He L, Uçeyler N, Krämer HH, Colaço MN, Lu B, Birklein F. Methylprednisolone prevents nerve injury-induced hyperalgesia in neprilysin knockout mice. Pain. 2014. 155: 574-80
68. Hollmann MW, Durieux M. Local anesthetics and the inflammatory response. Anesthesiology. 2000. 93: 858-75
69. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: Report of three cases. Spine J. 2002. 2: 70-5
70. Howick J, Bishop FL, Heneghan C, Wolstenholme J, Stevens S, Hobbs FD. Placebo use in the United Kingdom: Results from a national survey of primary care practitioners. PLOS One. 2013. 8: e58247-
71. Howick J, Friedemann C, Tsakok M, Watson R, Tsakok T, Thomas J. Are treatments more effective than placebos? A systematic review and meta-analysis. PLoS One. 2013. 8: e62599-
72. Hoy DG, Bain C, Williams G, March L, Brooks P, Blyth F. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012. 64: 2028-37
73. Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010. 24: 783-92
74. Hróbjartsson A, Gøtzsche PC. Placebo interventions for all clinical conditions. Cochrane Database Syst Rev. 2010. 1: CD003974-
75. Huntoon MA, Martin DP. Paralysis after transforaminal epidural injection and previous spinal surgery. Reg Anesth Pain Med. 2004. 29: 494-5
76. Huston CW, Slipman CW, Garvin C. Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehabil. 2005. 86: 277-83
77. Igarashi T, Kikuchi S, Shubayev V, Myers RR. Exogenous tumor necrosis factor-alpha mimics nucleus pulposusinduced neuropathology. Spine. 2000. 25: 2975-80
78. .editors. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011. p.
79. Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011. 343: d5278-
80. Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R. Surgery versus conservative management of sciatica due to a lumbar herniated disc: A systematic review. Eur Spine J. 2011. 20: 513-22
81. Kainer MA, Reagan DR, Nguyen DB, Wiese AD, Wise ME, Ward J. Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012. 367: 2194-203
82. Kang SS, Hwang BM, Son H, Cheong IY, Lee SJ, Chung TY. Changes in bone mineral density in postmenopausal women treated with epidural steroid injections for lower back pain. Pain Physician. 2012. 15: 229-36
83. Kang SS, Hwang BM, Son HJ, Cheong IY, Lee SJ, Lee SH. The dosages of corticosteroid in transforaminal epidural steroid injections for lumbar radicular pain due to a herniated disc. Pain Physician. 2011. 14: 361-70
84. Kaptchuk TJ, Friedlander E, Kelley JM, Sanchez MN, Kokkotou E, Singer JP. Placebos without deception: A randomized controlled trial in irritable bowel syndrome. PLoS ONE. 2010. 5: e15591-
85. Kaptchuk TJ, Stason WB, Davis RB, Legedza AR, Schnyer RN, Kerr CE. Sham device v inert pill: Randomised controlled trial of two placebo treatments. BMJ. 2006. 332: 391-7
86. Karaman H, Kavak GO, Tüfek A, Yldrm ZB. The complications of transforaminal lumbar epidural steroid injections. Spine (Phila Pa 1976). 2011. 36: E819-24
87. Karppinen J, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, Nieminen P. Periradicular infiltration for sciatica: A randomized controlled trial. Spine (Phila Pa 1976). 2001. 26: 1059-67
88. Karppinen J, Ohinmaa A, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T. Cost effectiveness of periradicular infiltration for sciatica: Subgroup analysis of a randomized controlled trial. Spine (Phila Pa 1976). 2001. 26: 2587-95
89. Kawamata M, Takahashi T, Kozuka Y, Nawa Y, Nishikawa K, Narimatsu E. Experimental incision induced pain in human skin: Effects of systemic lidocaine on flare formation and hyperalgesia. Pain. 2002. 100: 77-89
90. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: Two case reports. Pain Med. 2009. 10: 1389-94
91. Khan S, Pioro EP. Cervical epidural injection complicated by syrinx formation: A case report. Spine (Phila Pa 1976). 2010. 35: E614-6
92. Kim S, Hwang B. Relationship between bone mineral density and the frequent administration of epidural steroid injections in postmenopausal women with low back pain. Pain Res Manag. 2014. 19: 30-4
93. Kim WH, Sim WS, Shin BS, Lee CJ, Jin HS, Lee JY. Effects of two different doses of epidural steroid on blood glucose levels and pain control in patients with diabetes mellitus. Pain Physician. 2013. 16: 557-68
94. Klenerman L, Greenwood R, Davenport HT, White DC, Peskett S. Lumbar epidural injections in the treatment of sciatica. Br J Rheumatol. 1984. 23: 35-8
95. Koppert W, Ostermaier N, Sittl R, Weidner C, Schmelz M. Low dose lidocaine reduces secondary hyperalgesia by a central mode of action. Pain. 2000. 85: 217-24
96. Koppert W, Zeck S, Sittl R. Low dose lidocaine suppresses experimentally induced hyperalgesia in humans. Anesthesiology. 1998. 89: 1345-53
97. Kovacs FM, Urrútia G, Alarcón JD. Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: A systematic review of randomized controlled trials. Spine (Phila Pa 1976). 2011. 36: E1335-51
98. Kraemer J, Ludwig J, Bickert U, Owczarek V, Traupe M. Lumbar epidural perineural injection: A new technique. Eur Spine J. 1997. 6: 357-61
99. Lavoie PA, Khazen T, Filion PR. Mechanisms of the inhibition of fast axonal transport by local anesthetics. Neuropharmacology. 1989. 28: 175-81
100. Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions: Do age and gender matter? A population-based study of 34,902 Danish twins 20-71 years of age. BMC Musculoskelet Disord. 2009. 10: 39-
101. Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011. 89: 728-72
102. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009. 151: W65-94
103. Lyby PS, Forsberg JT, Asli O, Flaten MA. Induced fear reduces the effectiveness of a placebo intervention on pain. Pain. 2012. 153: 1114-21
104. Lyders EM, Morris PP. A case of spinal cord infarction following lumbar transforaminal epidural steroid injection: MR imaging and angiographic findings. AJNR Am J Neuroradiol. 2009. 30: 1691-3
105. MacMahon PJ, Crosbie I, Kavanagh EC. Reducing the risk of spinal cord infarction during transforaminal steroid injections. AJNR Am J Neuroradiol. 2010. 31: E32-
106. Malhotra G, Abbasi A, Rhee M. Complications of transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976). 2009. 34: 731-9
107. Manchikanti KN, Atluri S, Singh V, Geffert S, Sehgal N, Falco FJ. An update of evaluation of therapeutic thoracic facet joint interventions. Pain Physician. 2012. 15: E463-81
108. Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2 – Guidance. Pain Physician. 2012. 15: S67-116
109. Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM. An update of comprehensive evidence. based guidelines for interventional techniques of chronic spinal pain: Part II: Guidance and recommendations. Pain Physician. 2013. 16: S49-283
110. Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA. Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res. 2014. p.
111. Manchikanti L, Benyamin RM, Falco FJE, Caraway DL, Datta S, Hirsch JA. Guidelines warfare over interventional techniques: Is there a lack of discourse or straw man?. Pain Physician. 2012. 15: E1-26
112. Manchikanti L, Benyamin RM, Swicegood JR, Falco FJE, Datta S, Pampati V. Assessment of practice patterns of perioperative management of antiplatelet and anticoagulant therapy in interventional pain management. Pain Physician. 2012. 15: E955-68
113. Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012. 15: E199-245
114. Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. A randomized, double-blind controlled trial of lumbar interlaminar epidural injections in central spinal stenosis: 2-year follow-up. Pain Physician. 2015. 18: 79-92
115. Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. Lumbar interlaminar epidural injections in central spinal stenosis: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012. 15: 51-63
116. Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in chronic axial or discogenic low back pain: Results of a 2-year follow-up. Pain Physician. 2013. 16: E491-504
117. Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. Assessment of thoracic interlaminar epidural injections in managing chronic thoracic pain: A randomized, double-blind, controlled trial with a 2-year follow-up. Pain Physician. 2014. 17: E327-38
118. Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012. 5: 371-84
119. Manchikanti L, Cash KA, McManus CD, Pampati V. Fluoroscopic caudal epidural injections in managing chronic axial low back pain without disc herniation, radiculitis or facet joint pain. J Pain Res. 2012. 5: 381-90
120. Manchikanti L, Cash KA, Pampati V, Falco FJ. Transforaminal epidural injections in chronic lumbar disc herniation: A randomized, double-blind, active-control trial. Pain Physician. 2014. 17: E489-501
121. Manchikanti L, Cash KA, Pampati V, Malla Y. Two-year follow-up results of fluoroscopic cervical epidural injections in chronic axial or discogenic neck pain: A randomized, double-blind, controlled trial. Int J Med Sci. 2014. 11: 309-20
122. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. A randomized, double-blind, active control trial of fluoroscopic cervical interlaminar epidural injections in chronic pain of cervical disc herniation: Results of a 2-year follow-up. Pain Physician. 2013. 16: 465-78
123. Manchikanti L, Falco FJ, Diwan S, Hirsch JA, Smith HS. Cervical radicular pain: The role of interlaminar and transforaminal epidural injections. Curr Pain Headache Rep. 2014. 18: 389-
124. Manchikanti L, Falco FJE, Benyamin RM, Caraway DL, Helm S, Wargo BW. Assessment of infection control practices for interventional techniques: A best evidence synthesis of safe injection practices and use of single-dose medication vials. Pain Physician. 2012. 15: E573-614
125. Manchikanti L, Falco FJ, Benyamin RM, Caraway DL, Kaye AD, Helm S. Assessment of bleeding risk of interventional techniques: A best evidence synthesis of practice patterns and perioperative management of anticoagulant and antithrombotic therapy. Pain Physician. 2013. 16: SE261-318
126. Manchikanti L, Falco FJE, Benyamin RM, Kaye AD, Boswell MV, Hirsch JA. A modified approach to grading of evidence. Pain Physician. 2014. 17: E319-25
127. Manchikanti L, Falco FJ, Hirsch JA, Bicket M, Gupta A, Brown CH, Cohen SP. Epidural injections for spinal pain: A systematic review and meta-analysis evaluating the “control” injections in randomized controlled trials. Anesthesiology. 2013. 119: 907-31
128. Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM. Utilization of interventional techniques in managing chronic pain in the Medicare population: Analysis of growth patterns from 2000 to 2011. Pain Physician. 2012. 15: E969-82
129. Manchikanti L, Helm S, Fellows B, Janata JW, Pampati V, Grider JS. Opioid epidemic in the United States. Pain Physician. 2012. 15: ES9-38
130. Manchikanti L, Helm S, Singh V, Hirsch JA. Accountable interventional pain management: A collaboration among practitioners, patients, payers, and government. Pain Physician. 2013. 16: E635-70
131. Manchikanti L, Hirsch JA, Cohen SP, Heavner JE, Falco FJ, Diwan S. Assessment of methodologic quality of randomized trials of interventional techniques: Development of an interventional pain management specific instrument. Pain Physician. 2014. 17: E263-90
132. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical post-surgery syndrome: Preliminary results of a randomized, double-blind active control trial. Pain Physician. 2012. 15: 13-26
133. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic epidural injections in cervical spinal stenosis: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012. 15: E59-70
134. Manchikanti L, Malla Y, Wargo BW, Cash KA, McManus CD, Damron KS. A prospective evaluation of bleeding risk of interventional techniques in chronic pain. Pain Physician. 2011. 14: 317-29
135. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012. 15: 131-40
136. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. Complications of fluoroscopically directed facet joint nerve blocks: A prospective evaluation of 7,500 episodes with 43,000 nerve blocks. Pain Physician. 2012. 15: E143-50
137. Manchikanti L, Pampati V, Bakhit C, Rivera J, Beyer C, Damron K. Effectiveness of lumbar facet joint nerve blocks in chronic low back pain: A randomized clinical trial. Pain Physician. 2001. 4: 101-17
138. Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: Analysis of utilization trends and medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 2013. 38: 157-68
139. Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: A randomized, controlled, double blind trial with a two-year follow-up. Pain Physician. 2012. 15: 273-86
140. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Fluoroscopic caudal epidural injections in managing post lumbar surgery syndrome: Two-year results of a randomized, double-blind, active-control trial. Int J Med Sci. 2012. 9: 582-91
141. Manchikanti L, Singh V, Cash KA, Pampati V, Falco FJ. A randomized, double-blind, active-control trial of the effectiveness of lumbar interlaminar epidural injections in disc herniation. Pain Physician. 2014. 17: E61-74
142. Manchikanti L, Singh V, Falco FJ, Cash KA, Fellows B. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: A randomized, double. blind controlled trial. Pain Physician. 2010. 13: 437-50
143. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V, Fellows B. The role of thoracic medial branch blocks in managing chronic mid and upper back pain: A randomized, double-blind, active-control trial with a 2-year follow-up. Anesthesiol Res Pract 2012. 2012. p.
144. Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: A randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010. 7: 124-35
145. Manchikanti L, Singh V. Periradicular infiltration for sciatica. Spine (Phila Pa 1976). 2002. 27: 215-7
146. Manchikanti L, Singh V. Periradicular infiltration for sciatica. Spine (Phila Pa 1976). 2002. 27: 335-6
147. Manning DC, Hopwood MB. Corticosteroid injections for sciatica. N Engl J Med. 1997. 337: 1242-
148. Mao J, Chen LL. Systemic lidocaine for neuropathic pain relief. Pain. 2000. 87: 7-17
149. Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K. Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: A national database analysis between 2002 and 2011. Spine (Phila Pa 1976). 2014. 39: 476-81
150. Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W. Expenditures and health status among adults with back and neck problems. JAMA. 2008. 299: 656-64
151. Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine (Phila Pa 1976). 2009. 34: 2077-84
152. McCahon RA, Ravenscroft A, Hodgkinson V, Evley R, Hardman J. A pilot study of the dose-response of caudal methylprednisolone with levobupivacaine in chronic lower back pain. Anaesthesia. 2011. 66: 595-603
153. Meadeb J, Rozenberg S, Duquesnoy B, Kuntz JL, Le Loët X, Sebert JL. Forceful sacrococcygeal injections in the treatment of postdiscectomy sciatica. A controlled study versus glucocorticoid injections. Joint Bone Spine. 2001. 68: 43-9
154. Mehta S, Khalil AA, Alshekhlee A. Air myelopathy following a cervical epidural injection. Pain Med. 2010. 11: 1678-9
155. Melzack R, Coderre TJ, Katz J, Vaccarino AL. Central neuroplasticity and pathological pain. Ann N Y Acad Sci. 2001. 933: 157-74
156. Mendelson J, Muppidi S, Silberstein S. Multiple intracerebral hemorrhages after cervical epidural injections. Neurology. 2008. 70: 2415-6
157. Miedema HS, Chorus AM, Wevers CW, van der Linden S. Chronicity of back problems during working life. Spine. 1998. 23: 2021-8
158. Minamide A, Tamaki T, Hashizume H, Yoshida M, Kawakami M, Hayashi N. Effects of steroids and lipopolysaccharide on spontaneous resorption of herniated intervertebral discs: An experimental study in the rabbit. Spine (Phila Pa 1976). 1998. 23: 870-6
159. Nam HS, Park YB. Effects of transforaminal injection for degenerative lumbar scoliosis combined with spinal stenosis. Ann Rehabil Med. 2011. 35: 514-23
160. . National Government Services, Inc. LCD for Pain Management (L28529). Effective Date 01/01/2009. p.
161. Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain. A randomized, double-blind, controlled trial. Spine (Phila Pa 1976). 2005. 30: 857-62
162. . Noridian Healthcare Solutions, LLC. Local Coverage Determination (LCD). Lumbar Epidural Injections L33836. p.
163. Ohayon MM, Stingl JC. Prevalence and comorbidity of chronic pain in the German general population. J Psychiatr Res. 2012. 46: 444-50
164. Orlando MP, Sherman MO. Corticosteroid injections for sciatica. N Engl J Med. 1997. 337: 1242-
165. Owlia MB, Salimzadeh A, Alishiri G, Haghighi A. Comparison of two doses of corticosteroid in epidural steroid injection for lumbar radicular pain. Singapore Med J. 2007. 48: 241-5
166. Parr AT, Manchikanti L, Hameed H, Conn A, Manchikanti KN, Benyamin RM. Caudal epidural injections in the management of chronic low back pain: A systematic appraisal of the literature. Pain Physician. 2012. 15: E159-98
167. Pasqualucci A, Varrassi G, Braschi A, Peduto VA, Brunelli A, Marinangeli F. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: Single injection versus continuous infusion. Clin J Pain. 2007. 23: 551-7
168. Pasqualucci A. Experimental and clinical studies about the preemptive analgesia with local anesthetics. Possible reasons of the failure. Minerva Anestesiol. 1998. 64: 445-57
169. Pasquier MM, Leri D. Injection intra-et extradurales de cocaine a dose minime daus le traitments dela sciatique. Bull Gen Ther. 1901. 142: 196-
170. Patel N, Karppinen J. Periradicular infiltration for sciatica. A randomized controlled trial. Spine 26, 1059-1067:2001. Spine (Phila Pa 1976). 2002. 27: 1588-9
171. Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005. 57: 753-8
172. Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ. Epidural corticosteroid injections in the management of sciatica: A systematic review and meta-analysis. Ann Intern Med. 2012. 157: 865-77
173. Plastaras CT, Heller DS, Sorosky BS, Houle TT. Pain reproduction during lumbosacral transforaminal epidural steroid injection does not affect outcome. J Back Musculoskeletal Rehab. 2006. 19: 57-60
174. Price C, Arden N, Coglan L, Rogers P. Cost-effectiveness and safety of epidural steroids in the management of sciatica. Health Technol Assess. 2005. 9: 1-58
175. Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012. 37: 67-76
176. Raza K. Corticosteroid injections for sciatica. N Engl J Med. 1997. 337: 1241-
177. Revel M, Auleley GR, Alaoui S, Nguyen M, Duruoz T, Eck-Michaud S. Forceful epidural injections for the treatment of lumbosciatic pain with post-operative lumbar spinal fibrosis. Rev Rhum Engl Ed. 1996. 63: 270-7
178. Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000. 82-A: 1589-93
179. Roberts ST, Willick SE, Rho ME, Rittenberg JD. Efficacy of lumbosacral transforaminal epidural steroid injections: A systematic review. PM R. 2009. 1: 657-68
180. Saripanidis S, Lversen T. Re: Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011. 343: d5278-
181. Sato C, Sakai A, Ikeda Y, Suzuki H, Sakamoto A. The prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic pain. Anesth Analg. 2008. 106: 313-20
182. Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: A prospective, randomized, double-blind clinical trial. Spine (Phila Pa 1976). 2009. 34: 1441-7
183. Shah RV. Paraplegia following thoracic and lumbar transforaminal epidural steroid injections: How relevant are particulate steroids?. Pain Pract. 2014. 14: 297-300
184. Shah RV. Paraplegia following thoracic and lumbar transforaminal epidural steroid injections: How relevant is physician negligence?. J Neurointerv Surg. 2014. 6: 166-8
185. Sicard MA. Les injections medicamenteuse extradurales par voie saracoccygiene. Comptes Renues des Seances de la Societe de Biologie et de ses Filliales (Paris). 1901. 53: 452-3
186. Singh K, Nandyala SV, Marquez-Lara A, Fineberg SJ. Epidemiological trends in the utilization of bone morphogenetic protein in spinal fusions from 2002 to 2011. Spine (Phila Pa 1976). 2014. 39: 491-6
187. Smith RM, Schaefer MK, Kainer MA, Wise M, Finks J, Duwve J. Fungal infections associated with contaminated methylprednisolone injections. N Engl J Med. 2013. 369: 1598-609
188. Snoek W, Weber H, Jørgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta Orthop Scand. 1977. 48: 635-41
189. Staal JB, de Bie RA, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low back pain: An updated Cochrane review. Spine (Phila Pa 1976). 2009. 34: 49-59
190. Sugimoto M, Uchida I, Mashimoto T. Local anaesthetics have different mechanisms and sites of action at the recombinant NMDA receptors. Br J Pharmacol. 2003. 138: 876-82
191. Tachihara H, Sekiguchi M, Kikuchi S, Konno S. Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation. Spine (Phila Pa 1976). 2008. 33: 743-7
192. Tafazal S, Ng L, Chaudhary N, Sell P. Corticosteroids in peri-radicular infiltration for radicular pain: A randomised double blind controlled trial. One year results and subgroup analysis. Eur Spine J. 2009. 18: 1220-5
193. Thelin A, Holmberg S, Thelin N. Functioning in neck and low back pain from a 12-year perspective: A prospective population-based study. J Rehabil Med. 2008. 40: 555-61
194. Last accessed on 2015 Jan 27. Available from: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM394286.pdf .
195. . US Burden of Disease Collaborators. The state of US health, 1999-2010: Burden of diseases, injuries, and risk factors. JAMA. 2013. 310: 591-608
196. van Tulder MW, Suttorp M, Morton S, Bouter LM, Shekelle P. Empirical evidence of an association between internal validity and effect size in randomized controlled trials of low-back pain. Spine (Phila Pa 1976). 2009. 34: 1685-92
197. Ward A, Watson J, Wood P, Dunne C, Kerr D. Glucocorticoid epidural for sciatica: Metabolic and endocrine sequelae. Rheumatology (Oxford). 2002. 41: 68-71
198. Wilkinson IM, Cohen SP. Epidural steroid injections. Curr Pain Headache Rep. 2012. 16: 50-9
199. Wilson-MacDonald J, Burt G, Griffin D, Glynn C. Epidural steroid injection for nerve root compression: A randomized, controlled trial. J Bone Joint Surg Br. 2005. 87-B: 352-5
200. Wittenberg RH, Greskötter KR, Steffen R, Schoenfeld BL. Is epidural injection treatment with hypertonic saline solution in intervertebral disk displacement useful? (The effect of NaCl solution on intervertebral disk tissue). Z Orthop Ihre Grenzgeb. 1990. 128: 223-6
201. Yamashita T, Takahashi K, Yonenobu K, Kikuchi S. Prevalence of neuropathic pain in cases with chronic pain related to spinal disorders. J Orthop Sci. 2014. 19: 15-21
202. Yi Y, Hwang B, Son H, Cheong I. Low bone mineral density, but not epidural steroid injection, is associated with fracture in postmenopausal women with low back pain. Pain Physician. 2012. 15: 441-9
203. Yland MJ, Iversen T. Re: Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011. 343: d5278-
204. Zhang Y, Baik SH, Fendrick AM, Baicker K. Comparing local and regional variation in health care spending. N Engl J Med. 2012. 367: 1724-31