Abstract
Acute migraine treatment is given to abolish ongoing attacks, while prophylactic migraine treatment is given on a daily basis to prevent the occurrence of migraine attacks as far as possible. The majority of migraine patients do not use the specific acute anti-migraine drugs, the triptans. Thus, only 10% (Denmark) to 35% (France) of migraine patients use triptans. This is most likely due to relatively low efficacy. Thus, in randomized controlled trials (RCTs) pain freedom after 2 hours ranges from 12% (frovatriptan 2.5 mg) to 40% (rizatriptan 10 mg). For prophylactic treatment (propranolol, valproate, topiramate) a response (at least a 50% reduction in migraine frequency) is observed in 40–50%. In addition, prophylactic treatment is hampered by adverse events and withdrawals.
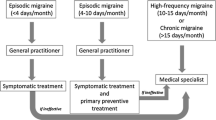
[There is a need for new acute anti-migraine drugs and targets are already available and there are more to come. It has been estimated that approximately 2% of the adult population need prophylactic treatment because of frequent migraine attacks. For prophylactic migraine drugs there is an even greater need for new drugs than for acute drug treatment.



Similar content being viewed by others
References
Dahlöf C, Hogenhuis L, Olesen J, et al. Early clinical experience with subcutaneous naratriptan in the acute treatment of migraine: a dose-ranging study. Eur J Neurol 1998; 5: 469–77
Tfelt-Hansen P. Parenteral versus oral sumatriptan and naratriptan: plasma levels and efficacy in migraine. A comment. J Headache Pain 2007; 8: 273–6
Tfelt-Hansen P. Maximum effect of triptans? A comment. Cephalalgia 2008; 28: 767–8
Treatment of migraine attacks with sumatriptan: the Subcutaneous Sumatriptan International Study Group. N Eng J Med 1991; 325: 316–21
Cady RK, Wendt JK, Kirchner JR, et al. Treatment of acute migraine with subcutaneous sumatriptan. JAMA 1991; 265: 2831–5
Tfelt-Hansen P. Excellent tolerability but relative low initial efficacy of telcagepant in the treatment of migraine. Headache 2011; 51: 118–23
Ferrari MD, Goadsby PJ, Roon KI, et al. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of a meta-analysis of 53 trials. Cephalalgia 2002; 22: 633–56
Saxena PR, Tfelt-Hansen P. Triptans, 5HT1B/1D agonists in the acute treatment of migraine. In: Olesen J, Goadsby PJ, Ramadan NM, et al., editors. The headaches. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2006: 469–503
Poolsup N, Leelasangaluk V, Jittangtrong J, et al. Efficacy of tolerability of frovatriptan in acute migraine treatment: systematic review of randomized controlled trials. J Clin Pharm Ther 2005; 30: 521–32
Kramer MS, Matzura-Wolf D, Polis A, et al. A placebo-controlled crossover study of rizatriptan in the treatment of multiple migraine attacks: Rizatriptan Multiple Attack Study Group. Neurology 1998; 51: 773–81
Diener H-C, Barbanti P, Dahlöf C, et al. BI 44370 TA, an oral CGRP antagonist for the treatment of acute migraine attacks: results from a phase II study. Cephalalgia 2011; 31: 573–84
Tfelt-Hansen P, Block G, Dahlöf C, et al. Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia 2000; 20: 765–86
Lipton RB, Stewart WF. Acute migraine therapy: do doctors understand what patients with migraine want from therapy? Headache 1999; 39 Suppl. 2: S20–6
Lantéri-Minet M, Massiou H, Romatet S, et al. An instrument to assess patient perception of satisfaction with acute migraine treatment (EXPERT Study). Headache 2011; 51: 590–601
Tfelt-Hansen P, Steiner TJ. Over-the-counter triptans for migraine: what are the implications? CNS Drugs 2007; 21: 877–83
Bigal ME, Borucho S, Serrano D, et al. The acute treatment of episodic and chronic migraine in the US. Cephalalgia 2009; 29: 891–7
Mathew NT, Kailasam J, Meadors L. Early treatment of migraine with rizatriptan: a placebo controlled study. Headache 2004; 44: 669–73
Goadsby PJ, Zanchin G, Geraud G, et al. Early vs. non-early intervention in acute migraine: ‘act when mild (AwM)’. A double-blind, placebo-controlled trial of almotriptan. Cephalalgia 2008; 28: 383–91
Silberstein SD, Mannix LX, Goldstein J, et al. Multi-mechanism (sumatriptan-naproxen) early intervention for the acute treatment of migraine. Neurology 2008; 71: 114–21
Tfelt-Hansen P, Rolan P. b-Adrenoceptor blocking drugs in migraine prophylaxis. In: Olesen J, Goadsby PJ, Ramadan NM, et al., editors. The headaches. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2006: 519–28
Holroyd KA, Penzien DB, Cordingley GE. Propranolol in the management of recurrent migraine: a meta-analytic review. Headache 1991; 31: 333–40
Diener HC, Tfelt-Hansen P, Dahlöf C. Topiramate in migraine prophylaxis: results from a placebo-controlled trial with propranolol as an active control. Eur Neurol 2004; 251: 943–50
Toda N, Tfelt-Hansen P. Calcium antagonists in migraine prophylaxis. In: Olesen J, Goadsby PJ, Ramadan NM, et al., editors. The headaches. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2006: 539–44
Celano CM, Freudenreich O, Fernandez-Robles C, et al. Depressogenic effects of medications: a review. Dialogues Clin Neurosci 2011; 13: 109–25
Silberstein SD, Tfelt-Hansen P. Antiepileptic drugs in migraine prophylaxis. In: Olesen J, Tfelt-Hansen P, Goadsby PJ, et al., editors. The headaches. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2006: 545–51
Mathew NT, Saper JR, Silberstein SD, et al. Migraine prophylaxis with divalproex. Arch Neurol 1995; 52: 281–6
Klapper JA. Divalproex sodium in migraine prophylaxis: a dose-controlled study. Cephalalgia 1997; 17: 103–8
Freitag FG, Collins SD, Carlson HA, et al. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology 2003; 58: 1652–9
McNamara JO. Drugs effective in the therapy of the epilepsies. In: Hardman JG, Limbird LE, Molinoff PB, et al., editors. Goodman and Gilman’s: the pharmacological basis of therapeutics. 9th ed. New York (NY): McGraw Hill, 1996: 461–80
Edvinsson L, Linde M. New drugs in migraine treatment and prophylaxis: telcagepant and topiramate. Lancet 2010; 376: 645–55
Adelman J, Freitag FG, Lainez M, et al. Analysis of safety and tolerability data obtained from over 1,500 patients receiving topiramate for migraine prevention in controlled trials. Pain Med 2008; 9: 175–85
Holroyd KA, Cottrell C, O’Donnel FJ, et al. Effect of preventive (β blocker) treatment, behavioural migraine management, or their combination on outcomes of optimized acute treatment in frequent migraine: randomised controlled trial. BMJ 2010; 341: c4871
Shuhendler AJ, Lee S, Siu M, et al. Efficacy of botulinum toxin type A for the prophylaxis of episodic migraine headaches: a meta-analysis of randomized, double-blind, placebo-controlled trials. Pharmacotherapy 2009; 29: 784–91
Lipton RB, Hamelsky SW, Dayno JM. What do patients with migraine want from acute migraine treatment? Headache 2002; 42 Suppl. 1: S3–9
International Headache Society Committee on Clinical Trials in Migraine (Tfelt-Hansen P, Chairman). Guidelines for controlled trials of drugs in migraine: first edition. Cephalalgia 1991; 11: 1–12
Andlin-Sobocki P, Jonsson B, Wittchen HU, et al. Cost of disorders of the brain in Europe. Eur J Neurol 2005; 12 Suppl. 1: 1–27
Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. Epub 2011 Dec 5
Lyngberg AC, Rasmussen BK, Jørgensen T, et al. Secular changes in health care utilization and work absence for migraine and tension-type headache: a population based study. Eur J Epidemiol 2005; 20: 1007–14
Durham PL, Vause CV. Calcitonin gene-related peptide (CGRP) receptor antagonists in the treatment of migraine. CNS Drugs 2010; 24: 539–48
Ferrari MD, Färkkilä M, Reuter U; European COL-144 Investigators. Acute treatment of migraine with the selective 5-HT1F receptor agonist lasmiditan: a randomised proof-of-concept trial. Cephalalgia 2010; 30: 1170–8
Lipton RB, Bigal ME, Diamond M, et al.AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007; 68: 343–9
Olesen J, Tfelt-Hansen P, Ashina M. Finding new drug targets for the treatment of migraine attacks. Cephalalgia 2009; 29: 909–20
Wienecke T, Olesen J, Oturai PS, et al. Prostaglandin E2(PGE2) induces headache in healthy subjects. Cephalalgia 2009; 29: 509–19
Antonova M, Wienicke T, Maubach K, et al. The pharmacological effect of BGC-1531, a novel prostanoid EP (4) receptor antagonist, in the prostaglandin E (2) human model of headache. J Headache Pain 2011; 12: 551–9
Ploug KB, Baun M, Hay-Schmidt A. Presence and vascular pharmacology of KATP channel subtypes in rat central and peripheral tissues. Eur J Pharmacol 2010; 637: 109–17
Anttila V, Stefansson H, Kallela M, et al.; International Headache Genetic Consortium. Genome-wide association study of migraine implicates a common susceptibility variant on 8q22. 1. Nat Genet 2010; 42: 869–73
Goadsby PJ, Charbit AR, Andreou AP, et al. Neurobiology of migraine. Neuroscience 2009; 161: 327–41
Acknowledgements
No sources of funding were used to prepare this article. The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tfelt-Hansen, P., Olesen, J. Taking the Negative View of Current Migraine Treatments. CNS Drugs 26, 375–382 (2012). https://doi.org/10.2165/11630590-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11630590-000000000-00000