Abstract
Background
In December 2007, the National Institute for Health and Clinical Excellence and the National Patient Safety Agency in the UK (NICE-NPSA) published guidance that recommends all adults admitted to hospital receive medication reconciliation, usually by pharmacy staff. A costing and report tool was provided indicating a resource requirement of £12.9 million for England per year. Pediatric patients are excluded from this guidance.
Objective
To determine the clinical significance of medication reconciliation in children on admission to hospital.
Methods
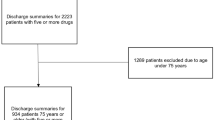
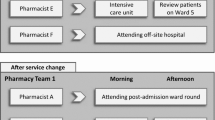
A prospective observational study included pediatric patients admitted to a neurosurgical ward at Birmingham Children’s Hospital, Birmingham, England, between September 2006 and March 2007. Medication reconciliation was conducted by a pharmacist after the admission of each of 100 consecutive eligible patients aged 4 months to 16 years. The clinical significance of prescribing disparities between pre-admission medications and initial admission medication orders was determined by an expert multidisciplinary panel and quantified using an analog scale. The main outcome measure was the clinical significance of unintentional variations between hospital admission medication orders and physician-prescribed pre-admission medication for repeat (continuing) medications.
Results
Initial admission medication orders for children differed from prescribed pre-admission medication in 39% of cases. Half of all resulting prescribing variations in this setting had the potential to cause moderate or severe discomfort or clinical deterioration. These results mirror findings for adults.
Conclusions
The introduction of medication reconciliation in children on admission to hospital has the potential to reduce discomfort or clinical deterioration by reducing unintentional changes to repeat prescribed medication. Consequently, there is no justification for the omission of children from the NICE-NPSA guidance concerning medication reconciliation in hospitals, and costing tools should include pediatric patients.


Similar content being viewed by others
References
Department of Health. Responsibility for prescribing between hospitals and GPs. EL (91) 127. London: Department of Health, 1991 Nov 1
British Medical Association. Prescribing and the primary and secondary care interface: guidance for GPs. London: BMA, 2007 Feb
McFadzean E, Isles C, Moffat J, et al. Is there a role for a prescribing pharmacist in preventing prescribing errors in a medical admission unit? Pharm J 2003; 270(7255): 896–9
Dodds LJ. An objective assessment of the role of the pharmacist in medication and compliance history taking. Br J Pharm Pract 1982; 4: 12–24
Department of Health. National service framework for children, young people and maternity services. London: Department of Health, 2004
National Institute for Health and Clinical Excellence, National Patient Safety Agency. Technical patient safety solutions for medicines reconciliation on admission of adults to hospital. Guidance 12. London: NICE, Dec 2007
National Institute for Health and Clinical Excellence, National Patient Safety Agency. Technical patient safety solutions for medicines reconciliation on admission of adults to hospital: costing template and report. Implementing NICE guidance. London: NICE, 2007 Dec
Ong SW, Fernandes OA, Cesta A, et al. Drug-related problems on hospital admission: relationship to medication information transfer. Ann Pharma-cother 2006; 40(3): 408–13
Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 2005; 165: 424–9
National Patient Safety Agency. Review of patient safety for children and young people. London: NPSA, 2009 Jun
National Prescribing Centre. Medicines management services: why are they so important? MeReC Bulletin 2002; 12(6): 21–3
Ahmed S, Harding J. Investigating the procedures, drawbacks and implications of seamless primary-secondary care. Qual Prim Care 2005; 13(1): 51–5
Hospital Pharmacists’ Group of Royal Pharmaceutical Society of Great Britain. Medicines management during patient admission to the ward. London: Royal Pharmaceutical Society of Great Britain, 2003
Royal Pharmaceutical Society of Great Britain. Medicines management during patient discharge. London: Royal Pharmaceutical Society of Great Britain, 2003
Winter SD, Spriet I, Indevuyst C, et al. Pharmacist- versus physician-acquired medication history: a prospective study at the emergency department. Qual Saf Health Care. Epub 2010 Jul 1
Royal Pharmaceutical Society of Great Britain. Moving patients’ medicines safely. Discharge and transfer planning workbook. London: Royal Pharmaceutical Society of Great Britain, 2006
Stone BL, Boehme S, Mundorff MB, et al. Hospital admission medication reconciliation in medically complex children: an observational study. Arch Dis Child 2010; 95: 250–5
Medicines policy. Birmingham: Birmingham Children’s Hospital, 2008
South Birmingham PCT. Prescribing and medicines management strategy 2005–2008 (SB-PCT). Birmingham: South Birmingham PCT, 2005 Nov 9
Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Soc 1927; 22: 209–12
National Prescribing Centre. Modernising medicines management, 2002 [online]. Available from URL: http://www.npc.co.uk/publications/MMS%20Presentation.pps#1 [Accessed 2008 Feb 8]
Robinson C. The medicines management collaborative. Prim Care Briefing 2004; (19): 4–8
Dean B, Schachter M, Vincent C, et al. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002; 359(9315): 1373–8
Glintborg B, Andersen SE, Dalhoff K. Insufficient communication about medication use at the interface between hospital and primary care. Qual Saf Health Care 2007; 16: 34–9
MacDonald A, Manji N, Evans S, et al. Home delivery of dietary products in inherited metabolic disorders reduces prescription and dispensing errors. J Hum Nutr Diet 2006; 19(5): 375–81
Dutton K, Hedger N, Wills S, et al. Prevent medication errors on admission. Clin Governance 2003; 8: 128–37
Fortesque E, Kaushal R, Landrigan C. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics 2003; 111 (Pt 1): 722–9
Gleason KM, Groszek JM, Sullivan C, et al. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health Syst Pharm 2004; 61: 1689–95
Stebbing C, Wong I, Kaushal R, et al. The role of communication in paediatric drug safety. Arch Dis Child 2007; 92: 440–5
Santell JP. Reconciliation failures lead to medication errors. Jt Comm J Qual Patient Saf 2006; 32: 225–9
Vira T, Colquhoun M, Etchells E. Reconcilable differences: correcting medication errors at hospital admission and discharge. Qual Saf Health Care 2006; 15(2): 122–6
Sanghera N, Chan PY, Khaki ZF, et al. Interventions of hospital pharmacists in improving drug therapy in children: a systematic literature review. Drug Saf 2006; 29(11): 1031–47
McRorie T. Quality drug therapy in children: formulations and delivery. Drug Inf J 1996; 30(4): 1173–7
Young SL. Providing pharmaceutical care to the pediatric patient. J Pharm Pract 1996; 9(1): 3–13
Miller MR, Robinson KA, Lubomski LH, et al. Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care 2007; 16: 116–26
Acknowledgements
We thank Carole Cummins and Claire Norton for their assistance with the design of this study and Maya Patel for her technical assistance in undertaking medication reconciliation. No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the content of this study. An application has been made to the Neonatal and Paediatrics Pharmacists’ Group (UK) to support an extension of this study at additional sites.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terry, D.R.P., Solanki, G.A., Sinclair, A.G. et al. Clinical Significance of Medication Reconciliation in Children Admitted to a UK Pediatric Hospital. Pediatr-Drugs 12, 331–337 (2010). https://doi.org/10.2165/11316230-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11316230-000000000-00000