Abstract
The size of the elderly population has been increasing steadily for several years. Individuals in this age group often have several concomitant diseases that require treatment with multiple medications. These drugs, for various reasons and especially as a consequence of potential accumulation, may be associated with adverse reactions. Of the numerous factors that can favour the occurrence of these adverse drug reactions, the most important are the pathophysiological consequences of aging, particularly as these apply to the very old.
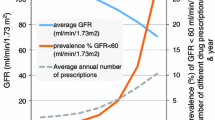
Although absorption of drugs is not usually reduced in the elderly, diffusion, distribution and particularly elimination decline with age. Furthermore, while hepatic metabolic function is fairly normal, renal function is usually markedly depressed in very old individuals, and this can translate into clinical consequences if it is not taken into account. This is why, before administration of any drug in the elderly, evaluation of glomerular filtration rate is essential. Validated estimations such as those obtained from the classical Cockcroft-Gault formula or from more recent methodologies are required.
In addition to reductions in various organ functions, factors connected with very old age such as frailty, falls, abnormal sensitivity to medications and polypathology, all of which tend to be more common in the last years of life, all directly impact on adverse drug reaction occurrence.
Given these characteristics of the elderly population, the best way to reduce the prevalence of adverse drug reactions in this group is to limit drug prescription to essential medications, make sure that use of prescribed agents is clearly explained to the patient, give drugs for as short a period as possible, and periodically re-evaluate all use of drugs in the elderly.



Similar content being viewed by others
References
World population prospects: the 2004 revision population database. United Nations: Population Division, 2004 [online]. Available from URL: http://esa.un.org/unpp/p2kOdata.asp [Accessed 2005 Apr 10]
Robine JM, Vaupel JW. Supercentenarians: slower ageing individuals or senile elderly? Exp Gerontol 2001; 36: 915–30
Robine JM, Saito Y, Jagger C. The emergence of extremely old people: the case of Japan. Exp Gerontol 2003; 38: 735–9
Institut National de la Statistique et des Etudes Economiques (INSEE). Recensement de la population française. Paris, France, 2004 [online]. Available from URL: http://www.recensement.insee.fr [Accessed 2005 Apr 10]
Kinsella K, Suzman R, Robine JM, et al. Demography of older populations in developed countries. In: Evans JG, Williams TF, Beattie BL, et al., editors. Oxford textbook of geriatric medicine. 2nd ed. Oxford: Oxford University Press, 2000: 7–19
EMEA. ICH Topic E2A: clinical safety data management — definitions and standards for expedited reporting. Step 5. London: European Agency for the Evaluation of Medicinal Products, Human Medicines Evaluation Unit, 1995 [online]. Available from URL: http://www.emea.euint/pdfs/human/ich/037795en.pdf [Accessed 2005 Apr 10]
Evans JG, Williams TF, Beattie BL. et al., editors. Oxford textbook of geriatric medicine. 2nd ed. Oxford: Oxford University Press, 2000
Lamy PP. Physiological changes due to age: pharmacodynamic changes of drug action and implications for therapy. Drugs Aging 1991; 1(5): 385–404
Meisami E. Aging of the nervous system: sensory changes. In: Timiras PT, editor. Physiological basis of geriatrics. New York: Macmillan, 1988: 156–78
Dukes MNG, Aronson JK, editors. Meyler’s side effects of drugs. 14th ed. Amsterdam: Elsevier, 2000
Fleg JL. Alterations in cardiovascular structure and function with advancing age. Am J Cardiol 1986; 57: 33C–44C
Rodeheffer RJ, Gerstenblith G, Becker LC, et al. Exercise cardiac output is maintained with advancing age in healthy human subjects: cardiac dilatation and increased stroke volume compensate for diminished heart rate. Circulation 1984; 69: 203–13
Oxenham H, Sharpe N. Cardiovascular aging and heart failure. Eur J Heart Fail 2003; 5: 427–34
Morley JE, Reese SS. Clinical implications of the aging heart. Am J Med 1989; 86: 77–86
Downes TR, Nomeir AM, Smith KM, et al. Mechanism of altered pattern of left ventricular filling with aging in subjects without cardiac disease. Am J Cardiol 1989; 64: 523–7
Goldberg JP, Anderson RJ. Renal metabolism and excretion of drugs. In: Seldin DW, Giebisch G, editors. The kidney: physiology and pathophysiology. New York: Raven Press, 1985: 2097–110
Cusack B, O’Malley K, Lavan J, et al. Protein binding and disposition of lignocaine in the elderly. Eur J Clin Pharmacol 1985; 29: 323–9
Hämmerlein A, Derendorf H, Lowenthal DT. Pharmacokinetic and pharmacodynamic changes in the elderly. Clin Pharmacokinet 1998; 35: 49–64
Jolliet-Riant P, Tillement JP. Drug transfer across the blood-brain barrier and improvement of brain delivery. Fundam Clin Pharmacol 1999; 13: 16–26
Garton MJ, Keir G, Lakshmi MV, et al. Age-related changes in cerebrospinal fluid protein concentrations. J Neurol Sci 1991; 104: 74–80
Mooradian AD. Potential mechanisms of the age-related changes in the blood-brain barrier. Neurobiol Aging 1994; 15: 751–5
Shah GN, Mooradian AD. Age-related changes in the blood-brain barrier. Exp Gerontol 1997; 32: 501–19
Brenner SS, Klots U. P-glycoprotein function in the elderly. Eur J Clin Pharmacol 2004; 60: 97–102
Ebly EM, Hogan DB, Fung TS. Potential adverse outcomes of psychotropic and narcotic drug use in Canadian seniors. J Clin Epidemiol 1997; 50: 857–63
Le Couteur DG, McLean AJ. The aging liver: drug clearance and an oxygen diffusion barrier hypothesis. Clin Pharmacokinet 1998; 34(5): 359–73
Schmucker DL, Woodhouse KW, Wang RK, et al. Effects of age and gender on in vitro properties of human liver microsomal monooxygenases. Clin Pharmacol Ther 1990; 48: 365–74
Grandison MK, Boudinot FD. Age-related changes in protein binding of drugs: implications for therapy. Clin Pharmacokinet 2000; 38(3): 271–90
Kato R, Takanaka A. Effect of phenobarbital on electron transport system, oxidation and reduction of drugs in liver microsomes of rats of different age. J Biochem (Tokyo) 1968; 63: 406–8
Herd B, Wynne H, Wright P, et al. The effect of age on glucuronidation and sulphation of paracetamol by human liver fractions. Br J Clin Pharmacol 1991; 32: 768–70
Wynne HA, Mutch E, James OF, et al. The effect of age upon the affinity of microsomal mono-oxygenase enzymes for substrate in human liver. Age Ageing 1988; 17: 401–5
Wynne HA, Yelland C, Cope LH, et al. The association of age and frailty with the pharmacokinetics and pharmacodynamics of metoclopramide. Age Ageing 1993; 22: 354–9
Tanaka E. In vivo age-related changes in hepatic drug oxidizing capacity in humans. J Clin Pharm Ther 1998; 23: 247–55
Vandel P. Antidepressant drugs in the elderly: role of the cytochrome P450 2D6. World J Biol Psychiatry 2003; 4: 74–80
Landi F, Cesari M, Russo A, et al. Benzodiazepines and the risk of urinary incontinence in frail older persons living in the community. Clin Pharmacol Ther 2002; 72: 729–34
Herrlinger C, Klotz U. Drug metabolism and drug interactions in the elderly. Best Pract Res Clin Gastroenterol 2001; 15(6): 897–918
Tauchi H, Tsuboi K, Okutoni J. Age changes in the human kidney of the different races. Gerontologia 1971; 17: 87–97
Corman B, Meyrier A. Le vieillissement de la fonction rénale. In: Maugourd MF, editor. Gérontologie. Montpellier: Sauramps Médical, 1992: 153–62
Dantoine T, Charmes JP, Merle L. Pharmacokinetic changes during renal failure and in the elderly [letter]. Presse Méd (Paris) 2001; 30: 1462
Rule AD, Larson TS, Bergstralh EJ, et al. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Am J Kidney Dis 2004; 43: 112–9
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31–41
Jelliffe RW, Jelliffe SM. A computer program for estimation of creatinine clearance from unstable serum creatinine levels, age, sex and weight. Math Biosci 1972; 14: 17–24
Jelliffe RW. Creatinine clearance: bedside estimate. Ann Intern Med 1973; 79: 604–5
Fliser D, Bischoff I, Hanses A, et al. Renal handling of drugs in the healthy elderly: creatinine clearance underestimates renal function and pharmacokinetics remain virtually unchanged. Eur J Clin Pharmacol 1999; 55: 205–11
Toto RD. Conventional measurement of renal function utilizing serum creatinine, creatinine clearance, inulin and para-aminohippurate acid clearance. Curr Opin Nephrol Hypertens 1995; 4: 505–9
Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999; 130: 461–70
Merle L, Laroche ML, Dantoine T, et al. Prospective pharmacovigilance study involving 2018 elderlies admitted to hospital [abstract]. Pharmacoepidemiol Drug Saf 2002; 11: S241
Merle L, Laroche ML, Dantoine T, et al. Adverse drug reactions in 90-year-old and over patients admitted to hospital [abstract]. Pharmacoepidemiol Drug Saf 2002, 11: S277
Begaud B, Evreux JC, Jouglard J, et al. Imputation of the unexpected or toxic effects of drags: actualization of the method used in France [in French]. Thérapie 1985; 40(2): 111–8
Lindeman RD, Tobin J, Shock NW. Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc 1985; 33: 278–85
Miura K, Goldstein RS, Morgan DG, et al. Age-related differences in susceptibility to renal ischemia in rats. Toxicol Appl Pharmacol 1987; 87: 284–96
Mimram A. Fonction rénale et vieillissement. Néphrologie 1990; 11: 275–80
Phillips PA, Rolls BJ, Ledingham JG, et al. Reduced thirst after water deprivation in healthy elderly men. N Engl J Med 1984; 311: 753–9
Epstein M, Hollenberg NK. Age as a determinant of renal sodium conservation in normal man. J Lab Clin Med 1976; 87: 411–7
Haller B, Zust H, Shaw S, et al. Effects of posture and ageing on circulating atrial natriuretic peptide levels in man. J Hypertens 1987; 5: 551–6
Steen B, Lundgren BK, Isaksson B. Body water in the elderly [letter]. Lancet, 1985; I: 101
Vestal RE, Wood AJJ, Shand DG. Reduced beta-adrenoceptor sensitivity in the elderly. Clin Pharmacol Ther 1979; 26: 181–6
O’Malley K, Kelly JC, Swift CG. Responsiveness to drugs. In: Swift CG, editors. Clinical pharmacology in the elderly. New York: Marcel Dekker, 1987: 83–101
Tonner PH, Kampen J, Scholz J. Pathophysiological changes in the elderly. Best Pract Res Clin Anaesthesiol 2003; 17: 163–77
Speechley M, Tinetti M. Falls and injuries in frail and vigorous community elderly persons. J Am Geriatr Soc 1991; 39: 46–52
Brocklehurst JC. The geriatric service and the day hospital. In: Brocklehurst JC, editor. Textbook of geriatric medicine and gerontology. 3rd ed. Edinburgh: Churchill Livingstone, 1985: 982–95
Vellas BJ, Baumgartner RN, Romero LJ, et al. Incidence and consequences of falls in free-living healthy elderly persons. Facts Res Gerontol 1993; 7: 131–42
Campbell AJ. Drag treatment as a cause of falls in old age: a review of offending agents. Drags Aging 1991; 1(4): 289–302
Tinetti ME, Doucette J, Claus E, et al. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc 1995; 43: 1214–21
Murphy J, Isaacs B. The post-fall syndrome: a study of 36 elderly patients. Gerontology 1982; 28: 265–70
Tinetti MF. Preventing falls in elderly persons. N Engl J Med 2003; 348: 42–9
Herings RM, Stricker BH, de Boer A, et al. Benzodiazepines and the risk of falling leading to femur fractures: dosage more important than elimination half-life. Arch Intern Med 1995; 155: 1801–7
Passaro A, Volpato S, Romagnoni F, et al. Benzodiazepines with different half-life and falling in a hospitalized population: the GIFA Study. Grappo Italiano di Farmacovigilanza nell’Anziano. J Clin Epidemiol 2000; 53: 1222–9
Linjakumpu T, Hartikainen S, Klaukka T, et al. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol 2002; 55: 809–17
Mannesse CK, Derkx FHM, de Ridder MAJ, et al. Contribution of adverse drag reactions to hospital admission of older patients. Age Ageing 2000; 29: 35–9
Clark D, Layton D, Shakir SAW. Monitoring the safety of over the counter medicines. BMJ 2001; 323: 706–7
Berry D, Raynor T, Knapp P, et al. Over the counter medicines and the need for immediate action: a further evaluation of European Commission recommended wordings for communicating risk. Patient Educ Couns 2004; 53: 129–34
Dave Flockart’s page. Cytochrome P450 drag interaction table [online]. Available from URL: http://medicine.iupui.edu/flockhart/table.htm [Accessed 2005 Apr 10]
Dilger K, Hofmann U, Klotz U. Enzyme induction in the elderly: effect of rifampicin on the pharmacokinetics and pharmacodynamics of propafenone. Clin Pharmacol Ther 2000; 67: 512–20
Lin JH, Lu AY. Interindividual variability in inhibition and induction of cytochrome P450 enzymes. Annu Rev Pharmacol Toxicol 2001; 41: 535–67
Col N, Fanale JE, Kronholm P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch Intern Med 1990; 150(4): 841–5
Stone AA, Shiffman S, Schwartz JE, et al. Patient non-compliance with paper diaries. BMJ 2002; 324: 1193–4
McLane CG, Zyzanski SJ, Flocke SA. Factors associated with medication non-compliance in rural elderly hypertensive patients. Am J Hypertens 1995; 8: 206–9
Morrell RW, Park DC, Kidder DP, et al. Adherence to antihypertensive medications across the life span. Gerontologist 1997; 37(5): 609–19
Hurd PD, Butkovich SL. Compliance problems and the older patient: assessing functional limitations. Drag Intel Clin Pharm 1986; 20: 228–31
van Eijken M, Tsang S, Wensing M, et al. Interventions to improve medication compliance in older patients living in the community: a systematic review of the literature. Drags Aging 2003; 20: 229–40
Lumme-Sandt K, Hervonen A, Jylhä M. Interpretative repertoires of medication among the oldest-old. Soc Sci Med 2000; 50: 1843–50
Britten N. Patients’ ideas about medicines: a qualitative study in a general practice population. Br J Gen Pract 1994; 44: 465–8
Jokisalo E, Enlund H, Halonen P, et al. Factors related to poor control of blood pressure with antihypertensive drag therapy. Blood Press 2003; 12: 49–55
Waeber B, Leonetti G, Kolloch R, et al. Compliance with aspirin or placebo in the Hypertension Optimal Treatment (HOT) study. Hypertension 1999; 17: 1041–5
Mengden T, Köhler C, Uen S, et al. Can drag-compliance and blood pressure control be improved by self-measurement and electronic reminders? [abstract]. Am J Hypertens 2001; 14Suppl. 1: A233
Salas M, In’t Veld BA, van der Linden PD, et al. Impaired cognitive function and compliance with antihypertensive drags in the elderly: the Rotterdam study. Clin Pharmacol Ther 2001; 70: 561–6
Hasan M, Woodhouse K. The accuracy of information on current drug therapy in geriatric out-patients’ records. Arch Gerontol Geriatr 1996; 22: 21–5
Parkin DM, Henney CR, Quirk J, et al. Deviation from prescribed drug treatment after discharge from hospital. BMJ 1976; 2: 686–8
Pearson RM. Who is taking their tablets? BMJ 1982; 285: 757–8
Park DC, Hertzog C, Leventhal H, et al. Medication adherence in rheumatoid arthritis patients: older is wiser. J Am Geriatr Soc 1999; 47: 172–83
Onder G, Pedone C, Landi F, et al. Adverse drug reactions as cause of hospital admissions: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA). J Am Geriatr Soc 2002; 50: 1962–8
Pouyanne P, Haramburu F, Imbs JL, et al. Admissions to hospital caused by adverse drug reactions: cross sectional incidence study. French Pharmacovigilance Centres. BMJ 2000; 320: 1036
Rich MW, McSherry F, Williford WO, et al. Effect of age on mortality, hospitalisations and response to digoxin in patients with heart failure: the DIG study. J Am Coll Cardiol 2001; 38: 806–13
Juntti-Patinen L, Neuvonen PJ. Drug-related deaths in a university central hospital. Eur J Clin Pharmacol 2002; 58: 479–82
Debord J, Charmes JP, Marquet P, et al. Population pharmacokinetics of amikacin in geriatric patients studied with the NPEM-2 algorithm. Int J Clin Pharmacol 1997; 35: 24–7
Leger F, Debord J, Le Meur Y, et al. Maximum a posteriori Bayesian estimation of oral cyclosporin pharmacokinetics in patients with stable renal transplants. Clin Pharmacokinet 2002; 41(1): 71–80
Kovarik JM, Koelle EU. Cyclosporin pharmacokinetics in the elderly. Drugs Aging 1999; 15(3): 197–205
Briesacher BA, Stuart B, Peluso R. Drug use and prescribing problems in the community-dwelling elderly: a study of three state Medicaid programs. Clin Ther 1999; 21: 2156–72
Acknowledgements
Each of the authors participated in this study and none has any conflict of interest to disclose.
We acknowledge the financial support of the French Drugs Agency, AFSSaPS (Agence Française de Sécurité Sanitaire des Produits de Santé).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Merle, L., Laroche, ML., Dantoine, T. et al. Predicting and Preventing Adverse Drug Reactions in the Very Old. Drugs Aging 22, 375–392 (2005). https://doi.org/10.2165/00002512-200522050-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200522050-00003