Abstract
Background
Inflammation is associated with a worse outcome in cancer and neutrophil:lymphocyte ratio (NLR) is a strong prognostic value. In cancer, nonsteroidal anti-inflammatory drugs (NSAIDs) could be of interest. We investigated the prognostic significance of NLR and the impact of intraoperative NSAIDs in cancer surgeries.
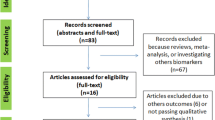
Methods
We performed an observational study in early breast, kidney, and lung cancers (357, 227, and 255 patients) with uni- and multivariate analyses (Cox model).
Results
In breast cancer (Centre 1), NLR ≥ 4 is associated with a higher risk of relapse (hazards ratio (HR) = 2.41; 95 % confidence interval (CI) 1.01–5.76; P = 0.048). In breast cancer (Centre 2), NLR ≥ 3 is associated with a higher risk of relapse (HR = 4.6; 95 % CI 1.09–19.1; P = 0.04) and higher mortality (HR = 4.0; 95 % CI 1.12–14.3; P = 0.03). In kidney cancer, NLR ≥ 5 is associated with a higher risk of relapse (HR = 1.63; 95 % CI 1.00–2.66; P = 0.05) and higher mortality (HR = 1.67; 95 % CI 1.0–2.81; P = 0.05). In lung cancer, NLR ≥ 5 is associated with higher mortality (HR = 1.45; 95 % CI 1.02–2.06; P = 0.04). The intraoperative use of NSAIDs in breast cancer patients (Centre 1) is associated with a reduced recurrence rate (HR = 0.17; 95 % CI 0.04–0.43; P = 0.0002) and a lower mortality (HR = 0.25; 95 % CI 1.08–0.75; P = 0.01). NSAIDs use at the beginning of the surgery is independently associated with a lower metastases risk after lung cancer surgery (HR = 0.16; 95 % CI 0.04–0.63; P = 0.009). Ketorolac use is independently associated with longer survival (HR = 0.55; 95 % CI 0.31–0.95; P = 0.03).
Conclusions
In these cohorts, these analyses show that NLR is a strong perioperative prognosis factor for breast, lung, and kidney cancers. In this context, intraoperative NSAIDs administration could be associated with a better outcome.








Similar content being viewed by others
References
Demaria S, Pikarsky E, Karin M, Coussens LM, Chen YC, El-Omar EM, Trinchieri G, Dubinett SM, Mao JT, Szabo E, Krieg A, Weiner GJ, Fox BA, Coukos G, Wang E, Abraham RT, Carbone M, Lotze MT. Cancer and inflammation: promise for biologic therapy. J Immunother. 2010;33(4):335–51.
Gibson PH, Croal BL, Cuthbertson BH, Small GR, Ifezulike AI, Gibson G, Jeffrey RR, Buchan KG, El-Shafei H, Hillis GS. Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass grafting. Am Heart J. 2007;154(5):995–1002.
Azab B, Chainani V, Shah N, McGinn JT. Neutrophil-lymphocyte ratio as a predictor of major adverse cardiac events among diabetic population: a 4-year follow-up study. Angiology. 2012. (in press).
Hung HY, Chen JS, Yeh CY, Changchien CR, Tang R, Hsieh PS, Tasi WS, You JF, You YT, Fan CW, Wang JY, Chiang JM. Effect of preoperative neutrophil-lymphocyte ratio on the surgical outcomes of stage II colon cancer patients who do not receive adjuvant chemotherapy. Int J Colorectal Dis. 2011;26(8):1059–65.
Tomita M, Shimizu T, Ayabe T, Yonei A, Onitsuka T. Preoperative neutrophil to lymphocyte ratio as a prognostic predictor after curative resection for non-small cell lung cancer. Anticancer Res. 2011;31(9):2995–8.
Sharaiha RZ, Halazun KJ, Mirza F, Port JL, Lee PC, Neugut AI, Altorki NK, Abrams JA. Elevated preoperative neutrophil:lymphocyte ratio as a predictor of postoperative disease recurrence in esophageal cancer. Ann Surg Oncol. 2011;18(12):3362–9.
Kim HS, Han KH, Chung HH, Kim JW, Park NH, Song YS, Kang SB. Neutrophil to lymphocyte ratio for preoperative diagnosis of uterine sarcomas: a case-matched comparison. Eur J Surg Oncol. 2010;36(7):691–8.
Garcea G, Ladwa N, Neal CP, Metcalfe MS, Dennison AR, Berry DP. Preoperative neutrophil-to-lymphocyte ratio (NLR) is associated with reduced disease-free survival following curative resection of pancreatic adenocarcinoma. World J Surg. 2011;35(4):868–72.
Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, Terjanian T, Widmann WD. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol. 2011;19(1):217–24.
Keizman D, Ish-Shalom M, Huang P, Eisenberger MA, Pili R, Hammers H, Carducci MA. The association of pre-treatment neutrophil to lymphocyte ratio with response rate, progression free survival and overall survival of patients treated with sunitinib for metastatic renal cell carcinoma. Eur J Cancer. 2011;48(2):202–8.
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS, Foulis AK, Horgan PG, McMillan DC. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow inflammation outcome study. Eur J Cancer. 2011;47(17):2633–41.
Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, Eccles D, Evans DG, Maher ER, Bertario L, Bisgaard ML, Dunlop MG, Ho JW, Hodgson SV, Lindblom A, Lubinski J, Morrison PJ, Murday V, Ramesar R, Side L, Scott RJ, Thomas HJ, Vasen HF, Barker G, Crawford G, Elliott F, Movahedi M, Pylvanainen K, Wijnen JT, Fodde R, Lynch HT, Mathers JC, Bishop DT; CAPP2 Investigators. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2012;378(9809):2081–7.
Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet. 2011;377(9759):31–41.
Rothwell PM, Wilson M, Price JF, Belch JF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet. 2012;379(9826):1591–601.
Rothwell PM, Price JF, Fowkes FG, Zanchetti A, Roncaglioni MC, Tognoni G, Lee R, Belch JF, Wilson M, Mehta Z, Meade TW. Short-term effects of daily aspirin on cancer incidence, mortality, and non-vascular death: analysis of the time course of risks and benefits in 51 randomised controlled trials. Lancet. 2012;379(9826):1602–12.
American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American society of anesthesiologists task force on acute pain management. Anesthesiology. 2012;116(2):248–73.
De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain. A meta-analysis of randomized trials. Anesth Analg. 2012;114(2), 424–433.
Forget P, Vandenhende J, Berliere M, Machiels JP, Nussbaum B, Legrand C, De Kock M. Do intraoperative analgesics influence breast cancer recurrence after mastectomy? A retrospective analysis. Anesth Analg. 2010;110(6):1630–5.
M Retsky M, Rogers R, Demicheli R, Hrushesky W, Gukas I, Vaidya JS, Baum M, Forget P, DeKock M, Pachmann K. NSAID analgesic ketorolac used perioperatively may suppress earlybreast cancer relapse: something for nothing in breast cancer? [Abstract] San Antonio Breast Cancer Symposium Dec 6–10, 2011. San Antonio, TX, USA.
Yakar I, Melamed R, Shakhar G, Shakhar K, Rosenne E, Abudarham N, Page GG, Ben-Eliyahu S. Prostaglandin e(2) suppresses NK activity in vivo and promotes postoperative tumor metastasis in rats. Ann Surg Oncol. 2003;10(4):469–79.
Poncelet AJ, Cornet J, Coulon C, Collard P, Noirhomme P, Weynand B; groupe d’oncologie thoracique des Cliniques Saint-Luc. Intra-tumoral vascular or perineural invasion as prognostic factors for long-term survival in early stage non-small cell lung carcinoma. Eur J Cardiothorac Surg. 2008;33(5):799–804.
Rutgers EJ. Guidelines to assure quality in breast cancer surgery. Eur J Surg Oncol. 2005;31(6):568–76.
Birido N, Geraghty JG. Quality control in breast cancer surgery. Eur J Surg Oncol. 2005;31(6):577–86.
Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thürlimann B, Senn HJ; Panel members. Meeting highlights: international expert consensus on the primary therapy of early breast cancer 2005. Ann Oncol. 2005;16(10):1569–83.
Goldhirsch A, Wood WC, Gelber RD, Coates AS, Thürlimann B, Senn HJ; 10th St. Gallen conference. Ann Oncol. 2007;18(7):1133–44.
Lee MC, Jasi R. Postmastectomy radiation therapy: indications and controversies. Surg Clin North Am. 2007;87(2):511–26.
Smith BD, Smith GL, Haffty BG. Postmastectomy radiation and mortality in women with T1–2 node-positive breast cancer. J Clin Oncol. 2005;23(7):1409–19.
Tisi G, Friedman P, Peters R, Pearso G, Carr D, Lee R, Selawry O. The American Thoracic Society, clinical staging of primary lung cancer. Am Rev Respir Dis. 1983;127(5):659–64.
Maclennan S, Imamura M, Lapitan MC, Omar MI, Lam TB, Hilvano-Cabungcal AM, Royle P, Stewart F, Maclennan G, Maclennan SJ, Dahm P, Canfield SE, McClinton S, Griffiths TR, Ljungberg B, N’dow J; UCAN Systematic Review Reference Group. Systematic review of perioperative and quality-of-life outcomes following surgical management of localised renal cancer. Eur Urol. 2012;62(6):1097–117.
Mandrekar SJ, Qi Y, Hillman SL, Allen Ziegler KL, Reuter NF, Rowland KM Jr., Kuross SA, Marks RS, Schild SE, Adjei AA. Endpoints in phase II trials for advanced non-small cell lung cancer. J Thorac Oncol. 2010;5(1):3–9.
Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60(3):615–22.
Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med. 1993;118(3):201–10.
Waymack JP, Flescher E, Venkatraman J, Fernandes G, Guzman RF, Yurt RW, Mason AD Jr, Pruitt BA Jr. Effect of prostaglandin E in multiple experimental models. VIII. Effect on host response to metastatic tumor. J Surg Oncol. 1991;48(4):239–45.
Okuno K, Jinnai H, Lee YS, Nakamura K, Hirohata T, Shigeoka H, Yasutomi M. A high level of prostaglandin E2 (PGE2) in the portal vein suppresses liver-associated immunity and promotes liver metastases. Surg Today. 1995;25(11):954–8.
Singh B, Lucci A. Role of cyclooxygenase-2 in breast cancer. J Surg Res. 2002:108(1):173–9.
Waymack JP, Flescher E, Venkatraman J, Fernandes G, Guzman RF, Yurt RW, Mason AD Jr, Pruitt BA Jr. Effect of prostaglandin E in multiple experimental models. VIII. Effect on host response to metastatic tumor. J Surg Oncol. 1991;48(4):239–45.
Melamed R, Rosenne E, Shakhar K, Schwartz Y, Abudarham N, Ben-Eliyahu S. Marginating pulmonary-NK activity and resistance to experimental tumor metastasis: suppression by surgery and the prophylactic use of a beta-adrenergic antagonist and a prostaglandin synthesis inhibitor. Brain Behav Immun. 2005;19(2):114–26.
Ostrand-Rosenberg S, Sinha P. Myeloid-derived suppressor cells: linking inflammation and cancer. J Immunol. 2009;182(8):4499–506.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. The value of histological grade in breast cancer: experience from a large study with long term follow up. Histopathology. 1991; 19:403–10.
Forget P, Tombal B, Scholtes JL, Nzimbala J, Meulders C, Legrand C, Van Cangh P, Cosyns JP, De Kock M. Do intraoperative analgesics influence oncological outcomes after radical prostatectomy for prostate cancer? Eur J Anaesthesiol. 2011;28(12):830–5.
Bischofs E, Lubs D, Fritzsche F, Meyer AS, Bruckner T, Sohn C, Eichbaum MH. In vitro blockade of adhesion of breast cancer cells to endothelial cells using anti-inflammatory drugs. Anticancer Res. 2012;32(3):767–71.
Li X, Gao L, Cui Q, Gary BD, Dyess DL, Taylor W, Shevde LA, Samant RS, Dean-Colomb W, Piazza GA, Xi Y. Sulindac inhibits tumor cell invasion by suppressing NF-κB-mediated transcription of microRNAs. Oncogene. 2012;31(48):4979–86.
Barlow M, Edelman M, Glick RD, Steinberg BM, Soffer SZ. Celecoxib inhibits invasion and metastasis via a cyclooxygenase 2-independent mechanism in an in vitro model of Ewing sarcoma. J Pediatr Surg. 2012;47(6):1223–7.
Acknowledgment
The authors thank Sarah Amar, M.D., Nathalie Blondeel, B.Sc., Monique Huang, M.D., Jean-Paul Lechat, M.D., and Julie Vandenhende, M.D., for their help in collecting the data. This work was supported by the Fondation Saint-Luc, the Departments of Anesthesiology, Oncology, Gynecology and Cardio-vascular and Thoracic Surgery, Saint-Luc Hospital, the Commission du Patrimoine of the Université catholique de Louvain and the Belgian Society of Anaesthesia and Resuscitation.
Conflict of interest
The authors attest no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Forget, P., Machiels, JP., Coulie, P.G. et al. Neutrophil:Lymphocyte Ratio and Intraoperative Use of Ketorolac or Diclofenac are Prognostic Factors in Different Cohorts of Patients Undergoing Breast, Lung, and Kidney Cancer Surgery. Ann Surg Oncol 20 (Suppl 3), 650–660 (2013). https://doi.org/10.1245/s10434-013-3136-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3136-x