Abstract
Background
A single preoperative prophylactic dose of an intravenous antibiotic with antistaphylococcal activity is standard of care for breast and axillary surgical procedures. Some surgeons also prescribe postoperative prophylaxis for all patients with drains to prevent infection despite its lack of proven efficacy.
Methods
A retrospective chart review of patients with breast and/or axillary surgical procedures between July 2004 and June 2006 were included. Data were collected on patient demographics, procedure types, and use of prophylactic antibiotics. Surgical site infection (SSI) was defined by means of Centers for Disease Control and Prevention criteria, including patients meeting the physician diagnosis criterion if an antibiotic was prescribed for a clinical diagnosis of cellulitis. χ2 and Fisher’s exact tests were used to compare SSI rates.
Results
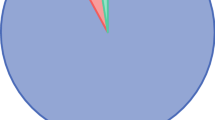
Three hundred fifty-three patients with 436 surgical sites who received either preoperative or both pre- and postoperative antibiotic were analyzed. Overall, the SSI rate was 7.8% (34 of 436 surgical sites). Eighty-five patients (24%) with 127 surgical sites were provided both preoperative and postoperative prophylactic antibiotics. The SSI rates did not differ statistically (P = .67) for the groups that did (95% confidence interval, 4.8–15.0; 11 of 127 surgical sites, 8.7%) and did not receive postoperative antibiotic prophylaxis (95% confidence interval, 5.0–11.0; 23 of 309, 7.4%).
Conclusions
Although the overall number of patients who developed SSI was relatively small, there was no reduction in the SSI rate among those who received postoperative antibiotic prophylaxis. Because of the potential adverse events associated with antibiotic use, further evaluation of this practice is required.
Similar content being viewed by others
References
Bold RJ, Mansfield PF, Berger DH, et al. Prospective, randomized, double-blind study of prophylactic antibiotics in axillary lymph node dissection. Am J Surg. 1998;176:239–43.
Coit DG, Peters M, Brennan MF. A prospective randomized trial of perioperative cefazolin treatment in axillary and groin dissection. Arch Surg. 1991;126:1366–71.
Platt R, Zucker JR, Zaleznik DF, et al. Prophylaxis against wound infection following herniorrhaphy or breast surgery. J Infect Dis. 1992;166:556–60.
Platt R, Zaleznik DF, Hopkins CC, et al. Perioperative antibiotic prophylaxis for herniorrhaphy and breast surgery. N Engl J Med. 1990;322:153–60.
Olsen MA, Chu-Ongsakul S, Brandt KE, et al. Hospital-associated costs due to surgical site infection after breast surgery. Arch Surg. 2008;143:53–60.
Pittet B, Montandon D, Pittet D. Infection in breast implants. Lancet Infect Dis. 2005;5:94–106.
Hedrick TL, Smith PW, Gazoni LM, Sawyer RG. The appropriate use of antibiotics in surgery: a review of surgical infections. Curr Probl Surg. 2007;44:635–75.
Sevin A, Senen D, Sevin K, Erdogan B, Orhan E. Antibiotic use in abdominoplasty: prospective analysis of 207 cases. J Plast Reconstr Aesthet Surg. 2007;60:379–82.
Adams WP Jr, Rios JL, Smith SJ. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: six-year prospective clinical study. Plast Reconstr Surg. 2006;117:30–6.
Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg. 2003;112:467–76.
Halvorson EG, Disa JJ, Mehrara BJ, et al. Outcome following removal of infected tissue expanders in breast reconstruction: a 10-year experience. Ann Plast Surg. 2007;59:131–6.
Macadam SA, Clugston PA, Germann ET. Retrospective case review of capsular contracture after two-stage breast reconstruction: is colonization of the tissue expander pocket associated with subsequent implant capsular contracture? Ann Plast Surg. 2004;53:420–4.
Perrotti JA, Castor SA, Perez PC, Zins JE. Antibiotic use in aesthetic surgery: a national survey and literature review. Plast Reconstr Surg. 2002;109:1685–93.
Wilke LG, McCall LM, Posther KE, et al. Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol. 2006;13:491–500.
Vilar-Compte D, Jacquemin B, Robles-Vidal C, Volkow P. Surgical site infections in breast surgery: case-control study. World J Surg. 2004;28:242–6.
Beatty JD, Robinson GV, Zaia JA, et al. A prospective analysis of nosocomial wound infection after mastectomy. Arch Surg. 1983;118:1421–4.
Felippe WA, Werneck GL, Santoro-Lopes G. Surgical site infection among women discharged with a drain in situ after breast cancer surgery. World J Surg. 2007;31:2293–9.
Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgical site infection after major breast operation. J Am Coll Surg. 2008;207:326–35.
Mansel RE, Fallowfield L, Kissin M, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006;98:599–609.
Lucci A, McCall LM, Beitsch PD, et al, American College of Surgeons Oncology Group. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007;25:3657–63.
Simpson SA, Ying BL, Ross LA, et al. Incidence of complications in outpatient mastectomy with immediate reconstruction. J Am Coll Surg. 2007;205:463–7.
Barton MB, West CN, Liu IL, et al. Complications following bilateral prophylactic mastectomy. J Natl Cancer Inst. Monogr. 2005:61–6.
Sullivan SR, Fletcher DR, Isom CD, Isik FF. True incidence of all complications following immediate and delayed breast reconstruction. Plast Reconstr Surg. 2008;122:19–28.
Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, Faucher A. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg. 2006;59:1017–24.
May AK, Fleming SB, Carpenter RO, et al. Influence of broad-spectrum antibiotic prophylaxis on intracranial pressure monitor infections and subsequent infectious complications in head-injured patients. Surg Infect (Larchmt). 2006;7:409–17.
Mandal AK, Montano J, Thadepalli H. Prophylactic antibiotics and no antibiotics compared in penetrating chest trauma. J Trauma. 1985;25:639–43.
Maxwell RA, Campbell DJ, Fabian TC, et al. Use of presumptive antibiotics following tube thoracostomy for traumatic hemopneumothorax in the prevention of empyema and pneumonia—a multi-center trial. J Trauma. 2004;57:742–8.
Olgac G, Aydogmus U, Mulazimoglu L, Kutlu CA. Antibiotics are not needed during tube thoracostomy for spontaneous pneumothorax: an observational case study. J Cardiothorac Surg. 2006;1:43.
LoCurto JJ Jr, Tischler CD, Swan KG, et al. Tube thoracostomy and trauma—antibiotics or not? J Trauma. 1986;26:1067–72.
Brunner RG, Vinsant GO, Alexander RH, Laneve L, Fallon WF Jr. The role of antibiotic therapy in the prevention of empyema in patients with an isolated chest injury (ISS 9-10): a prospective study. J Trauma. 1990;30:1148–53.
Nichols RL, Smith JW, Muzik AC, et al. Preventive antibiotic usage in traumatic thoracic injuries requiring closed tube thoracostomy. Chest. 1994;106:1493–8.
Acknowledgment
We thank Marilyn Churchward for her help preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Throckmorton, A.D., Boughey, J.C., Boostrom, S.Y. et al. Postoperative Prophylactic Antibiotics and Surgical Site Infection Rates in Breast Surgery Patients. Ann Surg Oncol 16, 2464–2469 (2009). https://doi.org/10.1245/s10434-009-0542-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-009-0542-1