-
PDF
- Split View
-
Views
-
Cite
Cite
Sandra Verelst, Pieter-Jan Moonen, Didier Desruelles, Jean-Bernard Gillet, Emergency Department Visits Due to Alcohol Intoxication: Characteristics of Patients and Impact on the Emergency Room, Alcohol and Alcoholism, Volume 47, Issue 4, July/August 2012, Pages 433–438, https://doi.org/10.1093/alcalc/ags035
Close - Share Icon Share
Abstract
Aims: The aim of the study was to describe the epidemiology, management and cost of emergency department (ED) visits due to alcohol intoxication. Methods: A retrospective review of medical records of all episodes of alcohol intoxication was made, excepting those where another diagnosis such as trauma or psychiatric illness was primary, in patients older than 16 years, who presented to the ED of a large university hospital in Belgium over a 12-month period from 1 January 2009. Results: A total of 635 such patients accounted for 1.2% of all ED visits; 429 were males and 48.3% were aged between 41 and 60 years; 63.8% of the patients had a history of alcohol use disorder and 60.3% had a history of psychiatric disorder; 74.3% of the patients received some form of medical treatment and 62% were seen by a psychiatrist. Of the total, 57.5% of the patients were admitted to the ED observation ward, with a mean length of stay of 8.4 h. The estimated total cost was €318 838.25, with an average of €541.32 per patient. Conclusion: Alcohol intoxication leads to a financial burden on the community. In addition to imposing physical, social and psychological stress on the community, the often agitated or aggressive patient imposes stress on ED staff. Close surveillance of trends in alcohol abuse is warranted, and the ED should consider implementing a questionnaire method of screening for alcohol abuse.
INTRODUCTION
Alcohol-related problems place a high burden on emergency departments (EDs) (Pirmohamed et al., 2000). Depending on the investigative method and the mixture of the target population, an estimated 0.6–40% of all ED visits are due to alcohol-related problems (Pirmohamed et al., 2000; Charalambous, 2002; Pletcher et al., 2004). Excessive acute and chronic alcohol intakes can lead to alcohol use disorders (AUDs), i.e. alcohol dependence and harmful use of alcohol as outlined in the International Statistical Classification of Disease 10th revision (ICD-10) (WHO, 2007).
EDs are in a potentially pivotal position to detect and refer to patients who misuse alcohol (Lockart, 1997; Whiterman et al., 2000). Furthermore, EDs are an appropriate place to offer patients initial help about their drinking habits (Green et al., 1993). The purpose of this article was to analyze the burden, in terms of resource utilization, imposed on the ED of a large university hospital in Belgium by patients presenting with alcohol intoxication. Our aim in this analysis is to formulate a uniform approach for treating alcohol-intoxicated patients presenting to the ED.
MATERIALS AND METHODS
Study design
This observational single-center study involved a retrospective medical record review of all patients presenting to the ED over a 12-month period from 1 January 2009 because of alcohol intoxication. Using physician discharge diagnosis codes, we identified all ED visits that appeared to be made primarily for alcohol intoxication. The WHO International Classification of Diseases, 10th Revision, codes that were considered to be indicative of such a visit, when used as the primary physician diagnosis, were acute alcohol intoxication (code F10.0) and dependence syndrome (code F10.2). Unless further specified, the term ‘alcohol intoxication’ used throughout the paper relates to these groups of patients.
Setting and study population
The university hospital subject to this study is situated in the city of Leuven, Belgium. The ED of our 1800-bed academic teaching hospital has an annual census of ∼55,000 patients and has a 23-unit observation ward that includes seven intensive care unit (ICU) beds. The priority in which presenting patients should be treated is determined by triage acuity. The physician in the ED treats acutely intoxicated patients. However, if a patient presents with a request for detoxification or with another psychiatric disorder, the patient is immediately referred to a psychiatrist at the ED. Patients who present themselves following trauma or medical condition, whether or not related to alcohol intoxication, are treated by the trauma or internal medicine resident, respectively. Since potential alcohol intoxication in these patients is a secondary diagnosis, they are not included in the present study. Blood alcohol concentration (BAC) levels are routinely obtained by the physician in the ED if the alcohol use is suspected. In cases where a psychiatrist is the treating physician, the BAC is obtained only when the patient needs an immediate psychiatric hospital admission. In contrast, whenever alcohol intoxication is a secondary diagnosis, the BAC levels are usually not routinely measured.
In general, the treating physician routinely asks the patient about the alcohol consumption level. However, no specific training is provided to nurses or physicians for detecting the alcohol misuse, nor do we apply specific screening tools such as the Paddington Alcohol Test (PAT) (Smith et al., 1996).
As a hospital policy, patients requiring observation for alcohol intoxication are admitted to the ED observation ward. Only in cases in which the estimated length of hospital stay exceeds 36–48 h, an ICU or medical ward transfer is requested. Therefore, an admission to the ED observation ward will be regarded as a hospital admission.
All patients older than 16 years visiting the ED with a primary history of alcohol intoxication were included in the study. If a patient presented several times with the same discharge diagnosis during the study period, each visit was considered as a separate case. Data on patients who presented with deliberate self-poisoning and who co-ingested alcohol were excluded from the study.
The study was approved by the hospital Ethics Committee. Given the observational design of the study, informed consent was waived.
Data collection and outcome measures
The following data elements were extracted from the hospital information system for each registered patient: demographic data (age, sex); referral source; time of arrival (including season, month of year, day of week, time of day) and time of discharge; triage category according to the Emergency Severity Index (ESI) (Wuerz et al., 2000); ED and total hospital length of stay; and final destination. Medical records of patients who presented to the ED during the above-described study period were reviewed for the following data: medical history according to the Charlson Comorbidity Index (CCI) (Charlson et al., 1987) and any history of previous AUD and/or psychiatric disorder. To estimate resource utilizations and outcomes, we analyzed the data on laboratory and radiology testing; consults from specialty services (including trauma and psychiatric care); treatment provided; and hospital admission. The BAC levels were classified according to the Y90 WHO coding (ICD-10) (Room, 2009). Costs of the ED stay were made available by our hospital's finance department. Direct medical costs (transportation costs, physicians' fees, technical procedures and treatment costs) were analyzed. Costs were determined by using the billing data. Costs related to revisits (psychiatric follow-up and others) following the primary visit to the ED were excluded. With the Belgian social security system, a part of medical expenses is reimbursed to insured patients. Cost calculation for uninsured patients is different. Therefore, this small group was excluded from cost calculation, since comparison with a large group of insured patients was not possible.
Primary data analysis
All retrieved data were transferred to a MicroSoft Excel® spreadsheet for further analysis. Statistics were performed using SPSS, version 17.0 (SPSS, IBM, New York). Descriptive statistics for continuous data included central tendency measures (mean or median), and the percentage frequency of occurrence was used for categorical-level data. Student's t-test and χ2 test were used for comparison of the groups. For multiple group comparisons, we used analysis of variance.
RESULTS
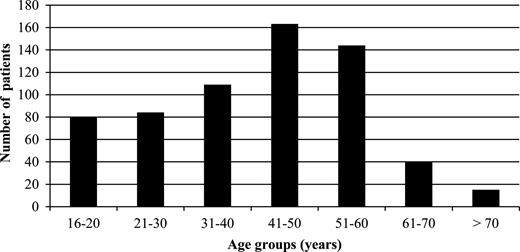
We retrieved a total of 680 patients who had a primary diagnosis of alcohol intoxication. Forty-five patients were excluded from the study for several reasons: 2 patients had their blood alcohol level taken on police demand only; 3 patients left the ED without being diagnosed; 23 patients were deliberately self-poisoned with alcohol as a co-ingestant; 11 patients had incorrect physician discharge diagnosis codes and 6 patients had no data available. As a result, 635 patients were included, representing 1.2% of all ED visits for the study period. Four hundred and twenty-nine patients were male, resulting in a male-to-female ratio of 2.08:1. The age range of patients was 16–87 years, with a mean age of 42 years. The age distribution of patients showed a marked skew toward the middle-aged groups, with 48.3% (n = 307) being between the ages of 41 and 60 (Fig. 1).
Most of the cases (48.9%) were transported to the ED by ambulance, 40.0% were transported by a layman, 4.3% by the police and 6.8% by an ambulance escorted by a mobile emergency team (i.e. an emergency physician and a nurse with the ability to provide an advanced life support). Patients brought in by ambulance had higher BAC levels than patients brought in by a layman.
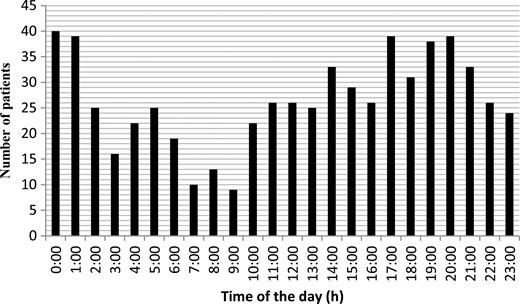
Patterns of alcohol intoxication visits were analyzed by month, day of the week and hour of the day. There was an equal distribution of visits throughout the day, with only a 2-h period between 7 and 9 a.m. when fewer patients were seen (Fig. 2). Likewise, there were no significant daily or monthly differences in visits across the included patients. Table 1 shows the distribution of the triage category according to age and gender at the time of ED arrival. There were 230 missing triage category data, leaving 405 (63.8%) patients with an ESI level. ESI levels showed a rather equal distribution between categories 2–5, both for male and for female patients. Triage category 1 was assigned to only 1.2% of the patients. Except for one, all of these patients had a Glasgow Coma Scale (GCS) of <6. Patients brought in by ambulance, with or without advanced life support assistance, received higher triage acuity levels than patients accompanied by a layman.
ESI triage category according to age, gender and method of arrival
| . | Age group (years) . | . | . | . | . | . | . | . | . | . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | 16–20 . | 21–30 . | 31–40 . | 41–50 . | 51–60 . | 61–70 . | >70 . | Male . | Female . | Total . | Lay. . | Amb. . | ALS . | Police . | Other . | Total . |
| Triage 1 | 0 (0.0%) | 2 (5.8%) | 0 (0.0%) | 1 (0.8%) | 2 (1.8%) | 0 (0.0%) | 0 (0.0%) | 4 (1.4%) | 1 (0.9%) | 5 (1.2%) | 0 (0.0%) | 3 (1.9%) | 3 (13.7%) | 0 (0.0%) | 0 (0.0%) | 6 (1.5%) |
| 2 | 2 (13.3%) | 13 (37.1%) | 28 (35.0%) | 25 (20.7%) | 21 (19.0%) | 8 (23.5%) | 0 (0.0%) | 70 (24.5%) | 27 (22.5%) | 97 (24.0%) | 32 (15.8%) | 47 (29.2%) | 11 (50.0%) | 6 (33.3%) | 0 (0.0%) | 96 (23.7%) |
| 3 | 6 (40.0%) | 9 (25.7%) | 15 (18.8%) | 29 (23.9%) | 29 (26.1%) | 17 (50.0%) | 4 (44.4%) | 72 (25.3%) | 37 (30.8%) | 109 (26.9%) | 35 (17.2%) | 63 (39.1%) | 6 (27.3%) | 3 (16.7%) | 0 (0.0%) | 107 (26.4%) |
| 4 | 5 (33.4%) | 7 (20.0%) | 22 (27.4%) | 35 (29.0%) | 32 (28.8%) | 6 (17.7%) | 5 (55.6%) | 82 (28.8%) | 30 (25.0%) | 112 (27.7%) | 74 (36.5%) | 35 (21.7%) | 1 (4.5%) | 4 (22.2%) | 0 (0.0%) | 114 (28.2%) |
| 5 | 2 (13.3%) | 4 (11.4%) | 15 (18.8%) | 31 (25.6%) | 27 (24.3%) | 3 (8.8%) | 0 (0.0%) | 57 (20.0%) | 25 (20.8%) | 82 (20.2%) | 62 (30.5%) | 13 (8.1%) | 1 (4.5%) | 5 (27.8%) | 1 (100.0%) | 82 (20.2%) |
| Total | 15 (3.7%) | 35 (8.6%) | 80 (19.8%) | 121 (29.9%) | 111 (27.4%) | 34 (8.4%) | 9 (2.2%) | 285 (70.3%) | 120 (29.7%) | 405 | 203 (50.1%) | 161 (39.8%) | 22 (5.4%) | 18 (4.4%) | 1 (0.3%) | 405 |
| . | Age group (years) . | . | . | . | . | . | . | . | . | . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | 16–20 . | 21–30 . | 31–40 . | 41–50 . | 51–60 . | 61–70 . | >70 . | Male . | Female . | Total . | Lay. . | Amb. . | ALS . | Police . | Other . | Total . |
| Triage 1 | 0 (0.0%) | 2 (5.8%) | 0 (0.0%) | 1 (0.8%) | 2 (1.8%) | 0 (0.0%) | 0 (0.0%) | 4 (1.4%) | 1 (0.9%) | 5 (1.2%) | 0 (0.0%) | 3 (1.9%) | 3 (13.7%) | 0 (0.0%) | 0 (0.0%) | 6 (1.5%) |
| 2 | 2 (13.3%) | 13 (37.1%) | 28 (35.0%) | 25 (20.7%) | 21 (19.0%) | 8 (23.5%) | 0 (0.0%) | 70 (24.5%) | 27 (22.5%) | 97 (24.0%) | 32 (15.8%) | 47 (29.2%) | 11 (50.0%) | 6 (33.3%) | 0 (0.0%) | 96 (23.7%) |
| 3 | 6 (40.0%) | 9 (25.7%) | 15 (18.8%) | 29 (23.9%) | 29 (26.1%) | 17 (50.0%) | 4 (44.4%) | 72 (25.3%) | 37 (30.8%) | 109 (26.9%) | 35 (17.2%) | 63 (39.1%) | 6 (27.3%) | 3 (16.7%) | 0 (0.0%) | 107 (26.4%) |
| 4 | 5 (33.4%) | 7 (20.0%) | 22 (27.4%) | 35 (29.0%) | 32 (28.8%) | 6 (17.7%) | 5 (55.6%) | 82 (28.8%) | 30 (25.0%) | 112 (27.7%) | 74 (36.5%) | 35 (21.7%) | 1 (4.5%) | 4 (22.2%) | 0 (0.0%) | 114 (28.2%) |
| 5 | 2 (13.3%) | 4 (11.4%) | 15 (18.8%) | 31 (25.6%) | 27 (24.3%) | 3 (8.8%) | 0 (0.0%) | 57 (20.0%) | 25 (20.8%) | 82 (20.2%) | 62 (30.5%) | 13 (8.1%) | 1 (4.5%) | 5 (27.8%) | 1 (100.0%) | 82 (20.2%) |
| Total | 15 (3.7%) | 35 (8.6%) | 80 (19.8%) | 121 (29.9%) | 111 (27.4%) | 34 (8.4%) | 9 (2.2%) | 285 (70.3%) | 120 (29.7%) | 405 | 203 (50.1%) | 161 (39.8%) | 22 (5.4%) | 18 (4.4%) | 1 (0.3%) | 405 |
Lay, layman; Amb, ambulance; ALS, advanced life support.
ESI triage category according to age, gender and method of arrival
| . | Age group (years) . | . | . | . | . | . | . | . | . | . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | 16–20 . | 21–30 . | 31–40 . | 41–50 . | 51–60 . | 61–70 . | >70 . | Male . | Female . | Total . | Lay. . | Amb. . | ALS . | Police . | Other . | Total . |
| Triage 1 | 0 (0.0%) | 2 (5.8%) | 0 (0.0%) | 1 (0.8%) | 2 (1.8%) | 0 (0.0%) | 0 (0.0%) | 4 (1.4%) | 1 (0.9%) | 5 (1.2%) | 0 (0.0%) | 3 (1.9%) | 3 (13.7%) | 0 (0.0%) | 0 (0.0%) | 6 (1.5%) |
| 2 | 2 (13.3%) | 13 (37.1%) | 28 (35.0%) | 25 (20.7%) | 21 (19.0%) | 8 (23.5%) | 0 (0.0%) | 70 (24.5%) | 27 (22.5%) | 97 (24.0%) | 32 (15.8%) | 47 (29.2%) | 11 (50.0%) | 6 (33.3%) | 0 (0.0%) | 96 (23.7%) |
| 3 | 6 (40.0%) | 9 (25.7%) | 15 (18.8%) | 29 (23.9%) | 29 (26.1%) | 17 (50.0%) | 4 (44.4%) | 72 (25.3%) | 37 (30.8%) | 109 (26.9%) | 35 (17.2%) | 63 (39.1%) | 6 (27.3%) | 3 (16.7%) | 0 (0.0%) | 107 (26.4%) |
| 4 | 5 (33.4%) | 7 (20.0%) | 22 (27.4%) | 35 (29.0%) | 32 (28.8%) | 6 (17.7%) | 5 (55.6%) | 82 (28.8%) | 30 (25.0%) | 112 (27.7%) | 74 (36.5%) | 35 (21.7%) | 1 (4.5%) | 4 (22.2%) | 0 (0.0%) | 114 (28.2%) |
| 5 | 2 (13.3%) | 4 (11.4%) | 15 (18.8%) | 31 (25.6%) | 27 (24.3%) | 3 (8.8%) | 0 (0.0%) | 57 (20.0%) | 25 (20.8%) | 82 (20.2%) | 62 (30.5%) | 13 (8.1%) | 1 (4.5%) | 5 (27.8%) | 1 (100.0%) | 82 (20.2%) |
| Total | 15 (3.7%) | 35 (8.6%) | 80 (19.8%) | 121 (29.9%) | 111 (27.4%) | 34 (8.4%) | 9 (2.2%) | 285 (70.3%) | 120 (29.7%) | 405 | 203 (50.1%) | 161 (39.8%) | 22 (5.4%) | 18 (4.4%) | 1 (0.3%) | 405 |
| . | Age group (years) . | . | . | . | . | . | . | . | . | . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | 16–20 . | 21–30 . | 31–40 . | 41–50 . | 51–60 . | 61–70 . | >70 . | Male . | Female . | Total . | Lay. . | Amb. . | ALS . | Police . | Other . | Total . |
| Triage 1 | 0 (0.0%) | 2 (5.8%) | 0 (0.0%) | 1 (0.8%) | 2 (1.8%) | 0 (0.0%) | 0 (0.0%) | 4 (1.4%) | 1 (0.9%) | 5 (1.2%) | 0 (0.0%) | 3 (1.9%) | 3 (13.7%) | 0 (0.0%) | 0 (0.0%) | 6 (1.5%) |
| 2 | 2 (13.3%) | 13 (37.1%) | 28 (35.0%) | 25 (20.7%) | 21 (19.0%) | 8 (23.5%) | 0 (0.0%) | 70 (24.5%) | 27 (22.5%) | 97 (24.0%) | 32 (15.8%) | 47 (29.2%) | 11 (50.0%) | 6 (33.3%) | 0 (0.0%) | 96 (23.7%) |
| 3 | 6 (40.0%) | 9 (25.7%) | 15 (18.8%) | 29 (23.9%) | 29 (26.1%) | 17 (50.0%) | 4 (44.4%) | 72 (25.3%) | 37 (30.8%) | 109 (26.9%) | 35 (17.2%) | 63 (39.1%) | 6 (27.3%) | 3 (16.7%) | 0 (0.0%) | 107 (26.4%) |
| 4 | 5 (33.4%) | 7 (20.0%) | 22 (27.4%) | 35 (29.0%) | 32 (28.8%) | 6 (17.7%) | 5 (55.6%) | 82 (28.8%) | 30 (25.0%) | 112 (27.7%) | 74 (36.5%) | 35 (21.7%) | 1 (4.5%) | 4 (22.2%) | 0 (0.0%) | 114 (28.2%) |
| 5 | 2 (13.3%) | 4 (11.4%) | 15 (18.8%) | 31 (25.6%) | 27 (24.3%) | 3 (8.8%) | 0 (0.0%) | 57 (20.0%) | 25 (20.8%) | 82 (20.2%) | 62 (30.5%) | 13 (8.1%) | 1 (4.5%) | 5 (27.8%) | 1 (100.0%) | 82 (20.2%) |
| Total | 15 (3.7%) | 35 (8.6%) | 80 (19.8%) | 121 (29.9%) | 111 (27.4%) | 34 (8.4%) | 9 (2.2%) | 285 (70.3%) | 120 (29.7%) | 405 | 203 (50.1%) | 161 (39.8%) | 22 (5.4%) | 18 (4.4%) | 1 (0.3%) | 405 |
Lay, layman; Amb, ambulance; ALS, advanced life support.
A history of AUD was present in 63.8% of all included patients, whereas 60.3% had a history of psychiatric disorder or prior psychiatric admission. Three hundred and forty-one patients (53.7%) had a history of both AUD and psychiatric disorder. Seventy-three patients (11.5%) visited the ED more than once within the study period, accounting for 193 of 635 visits (30.4%). These patients had an average of 2.6 visits, ranging from 2 to 10 visits within the study period. Highest rates of repeaters were found in the 41–50- and 51–60-year age groups. The mean age unadjusted CCI score was 0.47; the mean age adjusted CCI score was 0.97. Sixty-four patients (10.1%) had sustained a head injury at the time of ED visit, whereas 37 patients (5.8%) suffered an injury of the extremities. Two hundred and fifteen (33.9%) of 635 patients were immediately referred for psychiatric care within the ED. Of these patients, 161 (74.9%) suffered from AUD, representing 25.4% of all patients included in this study.
Systolic blood pressure was within normal limits in 266 (65.9%) of the patients. The mean values of saturation, heart rate and temperature appeared to be within the normal range. The majority of patients (93.9%) had a normal pupil size, and 501 patients (85.6%) had a GCS >13. However, patients brought in by ambulance, whether or not accompanied by a medical emergency team, were found to have a significantly lower GCS (P < 0.001) and blood pressure (P = 0.022).
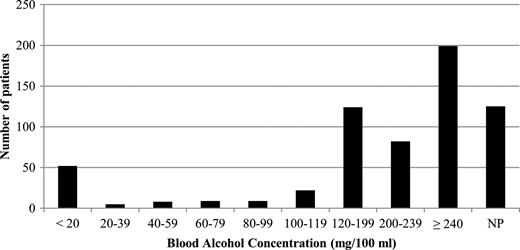
A blood sample was taken in 83.1% of the patients. The most frequently requested laboratory tests were the liver (67.9%) and kidney (72.3%) function tests, electrolytes (73.2%) and complete blood count (72.9%). A BAC was requested in 80.3% of the cases. Almost one-third of the study population had a BAC equal or higher than 240 mg/100 ml (Fig. 3). Patients younger than 40 years of age tended to have higher median blood alcohol levels than older patients. Some form of X-ray was performed in 23.2% of the cases; more than half of these (13.4%) were chest X-rays. Furthermore, 20.3% of the patients received an electrocardiogram (ECG), and in 12.3% of the cases a computed tomography (CT) of the skull was taken. Higher blood alcohol levels were associated significantly with the number of laboratory tests performed (P < 0.001) and with the request for an ECG (P = 0.016). Likewise, higher acuity levels and increasing age were associated with more laboratory tests and technical investigations.
Range of blood alcohol concentration levels according to the Y90 WHO coding (ICD-10) (Room, 2009). NP, not performed.
Half of the patients (57.5%) were admitted to the ED observational ward, and 74.3% received some form of medical treatment. The most frequently applied treatments were administration of fluids (67.7%), vitamin B1 (47.9%) and benzodiazepines (43.6%). Vitamin B1 was given intravenously in 79.3% of instances and orally in 20.7%. In 53.1% of the cases, benzodiazepines were given in the acute setting of aggression or suicidal ideation (72.1%) or in the setting of delirium tremens (27.9%). In the remaining cases, benzodiazepines were given as a preventive measure. Anti-psychotic drugs (6.1%) were mainly given in the acute setting of aggression. Eight patients (1.3%) required endotracheal intubation, whereas 10.4% needed wound care. Three hundred and ninety-four (62%) were seen by a psychiatrist at the ED observation ward. Of these, 215 (33.9%) were subsequently admitted to a psychiatric ward. Social services were contacted in 5.8% of all visits. Four patients (0.6%) were transferred to the ICU, and 75 patients (11.8%) left the hospital against medical advice. One 62-year-old patient (0.2%) died from a cerebral hemorrhage.
The overall median and mean length of stay at the ED observation ward were 5.5 and 8.4 h, respectively (range: 10 min–3 days, 21 h 22 min).
The treatment cost was available for 589 (92.8%) of 635 patients. The remaining 46 patients were uninsured. The estimated total cost of treating 589 patients from ED presentation to ED discharge was €318 838.25, with an average of €541.32 per patient. Given our social security system, 16.3% of this cost was charged to the patient; the remaining was charged to the community.
DISCUSSION
Alcohol intoxication represented 1.2% of all ED visits during the 12-month study period. This is consistent with a survey performed by Pletcher et al. (2004) in which 0.8% of ED visits were primarily related to alcohol intoxication. In contrast, alcohol-related problems accounted for 12% of all ED attendances in the 2-month prospective survey of Pirmohamed et al. (2000). In a 1-month prospective survey performed in a single university hospital in Belgium, Calle et al. (2006) determined that 7.4% of ED attendances were related to alcohol abuse. However, as these surveys included patients with health problems related to alcohol consumption and patients experiencing trauma as a result of their excess alcohol consumption, comparison with the current study was not possible.
The ED visit rate of alcohol-intoxicated men was twice that of women, which is consistent with previous work (Pletcher et al., 2004; Calle et al., 2006; Freitas et al., 2008; Lee et al., 2009; Rehm et al., 2009; Yoonhee et al., 2009). Likewise, we found a consistently higher representation of middle-aged adults, with 48.3% of patients being between the ages of 41 and 60 (Pletcher et al., 2004; Calle et al., 2006).
A significant number of patients received some form of technical investigation, such as an X-ray, a CT of the skull or an ECG. Alcohol impairs the clinical assessment and a patient's perception of pain. As a result, occult, yet important injuries might go unnoticed. Therefore, technical investigations are warranted, especially in patients severely impaired due to high BAC levels (Giovanardi et al., 2005; Savola et al., 2005; Macdonald et al., 2006; Freitas et al., 2008; Shults et al., 2009; Yoonhee et al., 2009). Likewise, Aasebo et al. (2007) demonstrated that several changes in the ECG due to high BAC levels might be associated with an increased risk of arrhythmias. Seventy-four percent of our patients received some form of treatment in the current study. The frequent administration of benzodiazepines in our study was largely attributable to agitated intoxicated patients presenting to the ED. In this regard, Moritz et al. (1999) similarly observed a high incidence of alcohol intoxication in the agitated patient population admitted to their ED. Other reasons for the administration of benzodiazepines were a clinically visible tremor, paroxysmal sweating, mild-to-severe anxiety attacks or mild-to-severe hallucinations. However, a formal clinical assessment for the detection of withdrawal signs as described in the Clinical Institute Withdrawal Assessment for Alcohol scale was not performed. Despite the dramatic use of psychiatric services in the present study (62% of our patients were seen by a psychiatrist at the ED observation ward), 11.5% of patients visited the ED more than once within the study period. Although outpatient follow-up consultations are provided by the psychiatrist and psychiatric nurse in our hospital, no systematic use is made of Alcohol Health workers in order to reduce alcohol-related unscheduled ED re-attendances. Since Crawford et al. found that patients receiving an appointment with an alcohol health worker had lower levels of alcohol consumption over the following 6 months, and reduced re-attendances at the ED, implementation of these experienced mental health nurses should be considered (Crawford et al., 2004). Furthermore, Bernstein and Bernstein described the evolution of a universal screening, brief intervention and referral to treatment in the ED. Excessive drinkers in the intervention group reported significantly fewer drinks per week (Bernstein and Bernstein, 2009). Likewise, the Department of Health in England refers to alcohol screening and brief interventions as an important plank in combating the harm caused by alcohol misuse in England (Lavoie, 2010). As a consequence, the American College of Surgeons Committee on Trauma required Level I and II trauma centers to have a mechanism for identifying patients with alcohol problems and Level I centers to have the capability to provide a brief counseling intervention for patients identified as problem drinkers (Committee on Trauma, 2006). Finally, the UK website on Screening and Intervention Programme for Sensible drinking provides important information on screening tools, intervention tools and assessment tools for practitioners in various settings (UK website).
The findings of this study are subject to a number of limitations. First, the selection of cases might have been incomplete, since it depended on the accuracy of the physician discharge diagnosis codes. Moreover, the study was performed in only one Belgian university hospital. The estimation of true prevalence rates and resources used for alcohol-intoxicated patients in Belgium was therefore impossible. Secondly, patients with alcohol intoxication as a secondary diagnosis were not included in our study. In addition, alcohol misuse among patients attending hospital is common but frequently undetected since physicians are not taught to recognize the symptoms and sings of alcoholism (Barrison et al., 1980, 1982; Paton, 1989). Moreover, since no brief test for alcohol misuse such as the PAT was performed, patients with presenting conditions of fall or minor head injury are an important group of patients that might have been missed (Huntley et al., 2001). This obviously leads to a significant underestimation of alcohol-related problems (Chick, 1993). Indeed, Drummond et al. (2005) reported the mean incidence of hazardous drinking among patients attending UK EDs as 43%, rising to 70% at peak times when proactively looking for the alcohol misuse. Thirdly, in contrast to most surrounding hospitals, our university hospital has an ED psychiatric service available 24/7. Therefore, our ED serves as a referral center for patients with AUD. Fourthly, due to the retrospective study design, potentially important data could have been missed because of incomplete medical records. Finally, the estimated cost of treating alcohol-intoxicated patients presenting to the ED does not reflect the results of a complete financial analysis, as we provided only an estimate of costs generated within the ED. Potential in-hospital or outpatient costs were not calculated, nor were costs included of patients with alcohol as a secondary diagnosis. Including such costs and patients into our cost analysis would have affected the total cost due to alcohol intoxication.
CONCLUSION
We have analyzed the characteristics of patients with alcohol intoxication seen in the ED of a large university hospital in Belgium. Findings on demographic data can be compared with previous studies. In essence, the presenting patients were mainly middle-aged men.
Our study population had a remarkable high incidence of prior AUD and/or a history of psychiatric disorder. In addition, repeaters represented a significant proportion of our ED visits for alcohol intoxication. Although our 24/7 availability of the psychiatric service can contribute to an easier accessibility, we noticed a dramatic use of psychiatric services in the present study. Moreover, one-third of the included patients were subsequently admitted to a psychiatric ward. Together with the frequent administration of vitamin B1 and benzodiazepines, we can conclude that a significant part of our study population was in fact alcohol dependent. These findings highlight the importance of the detection of alcohol misuse in the ED and early intervention to prevent the development of dependency. Therefore, our ED should consider a screening tool such as the PAT (Smith et al., 1996). This would certainly contribute to a more efficient detection of alcohol-related problems in an earlier state for which brief intervention by the psychiatrist can be implemented. Furthermore, the follow-up of the detected alcohol misuse needs to be stressed for which the patient's primary care physician should be informed.
Finally, the often agitated or aggressive intoxicated patient imposes a significant stress on ED staff. In addition, in 2009, the estimated total ED cost was €318 838.25 for patients with alcohol intoxication, thereby putting a significant financial burden on the community. Whether this problem could be mitigated by raising taxes on alcohol is a topic for debate.
Acknowledgements
We thank Mr Jochen Bergs, R.N. for providing patient data using the hospital information system. We also thank Prof. Katrien Kesteloot and Mr Guido Peers from the hospital financial department for providing figures on ED costs.
REFERENCES
- alcohol abuse
- alcohol intoxication
- medical records
- psychological stress
- epidemiology
- belgium
- emergency service, hospital
- hospitals, university
- length of stay
- mental disorders
- patients' rooms
- wounds and injuries
- diagnosis
- stress
- agitation
- alcohol use disorder
- surveillance, medical
- psychiatrists
- community
- medical management