Abstract
BACKGROUND: African-American and low-income women have lower rates of cancer screening and higher rates of late-stage disease than do their counterparts.
OBJECTIVE: To examine the effects of primary care, health insurance, and HMO participation on adherence to regular breast, cervical, and colorectal cancer screening.
DESIGN: Random-digit-dial and targeted household telephone survey of a population-based sample.
SETTING: Washington, D.C. census tracts with ≥30% of households below 200% of federal poverty threshold.
PARTICIPANTS: Included in the survey were 1,205 women over age 40, 82% of whom were African American.
MAIN OUTCOME MEASURES: Adherence was defined as reported receipt of the last 2 screening tests within recommended intervals for age.
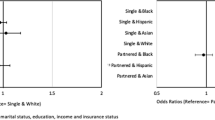
RESULTS: The survey completion rate was 85%. Overall, 75% of respondents were adherent to regular Pap smears, 66% to clinical breast exams, 65% to mammography, and 29% to fecal occult blood test recommendations. Continuity with a single primary care practitioner, comprehensive service delivery, and higher patient satisfaction with the relationships with primary care practitioners were associated with higher adherence across the 4 screening tests, after considering other factors. Coordination of care also was associated with screening adherence for women age 65 and over, but not for the younger women. Compared with counterparts in non-HMO plans, women enrolled in health maintenance organizations were also more likely to be adherent to regular screening (e.g., Pap, odds ratio [OR] 1.89, 95% confidence interval [CI] 1.11 to 3.17; clinical breast exam, OR 2.04, 95% CI 1.21 to 3.44; mammogram, OR 1.95, 95% CI 1.15 to 3.31; fecal occult blood test, OR 1.70, 95% CI 1.01 to 2.83.)
CONCLUSIONS: Organizing healthcare services to promote continuity with a specific primary care clinician, a comprehensive array of services available at the primary care delivery site, coordination among providers, and better patient-practitioner relationships are likely to improve inner-city, low-income women’s adherence to cancer screening recommendations.
Similar content being viewed by others
References
Cancer Statistics ReviewCS. 1973–1987. SEER Program. Bethesda Md: U.S. Department of Health and Human Services, PHS, NIH, NCI. NIH publication no. 90-2789;1990.
Axtell LM, Myers M. Contrasts in survival of black and white cancer patients. 1960–1973. J Natl Cancer Inst. 1978;60:1209–15.
Bassett T, Krieger N. Social class and black-white differences in breast cancer survival. Am J Public Health. 1986;76:1400–3.
National Cancer Institute. Cancer Statistics Review 1973–1986: Including a Report on the Status of Cancer Control. Bethesda, Md: U.S. Department of Health and Human Services. National Cancer Institute. NIH publication no. 89-2789;1989.
Eley JW, Hill HA, Chen VW, et al. Racial differences in survival from breast cancer. JAMA. 1994;272:947–54.
Vernon SW, Tiley BC, Neale AV, Steinfledt L. Ethnicity, survival, and delay in seeking treatment for symptoms of breast cancer. Cancer. 1985;55:1563–71.
Nemoto T, Vana J, Bedwani RN, Baker HW, McGregor FH, Murphy GP. Management and survival of female breast cancer: results of a national survey by the American College of Surgeons. Cancer. 1980;45:2917–24.
Calle EE, Flanders WD, Thun MJ, Martin LM. Demographic predictors of mammography and Pap smear screening by US women. Am J Public Health. 1993;83:53–60.
McCarthy EP, Burns RB, Coughlin SS, et al. Mammography use helps to explain differences in breast cancer stage at diagnosis between older black and white women. Ann Intern Med. 1998;128:729–36.
Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9.
Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91:1409–15.
Baker LH. Breast cancer detection demonstration project: five year summary report. Cancer. 1982;32:192–225.
Shapiro S, Strax P, Venet L, Rosen R. Ten-to-fourteen years’ effect of screening on breast cancer mortality. J Natl Cancer Inst. 1982;69:349–55.
Tabar L, Fagerberg CJ, Gad A, et al. Reduction in mortality from breast cancer after mass screening with mammography. Randomized trial from the Breast Cancer Screening Working Group of the Swedish Board of Health and Welfare. Lancet. 1985;8433:829–32.
Shapiro S, Venet W, Strax P, Venet L. Periodic Screening for Breast Cancer: The Health Insurance Plan Project and Its Sequelae, 1963–1986. Baltimore, Md: Johns Hopkins University Press; 1988.
Collette HJA, Day NE, Romback JJ, et al. Evaluation of screening for breast cancer in a non-randomized study (the DOM project) by means of a case-control study. Lancet. 1984;1:1224–6.
O’Malley MD, Fletcher SW, Morrison B. Does screening for breast cancer save lives? Effectiveness of treatment after breast cancer detection following screening by clinical breast examination, mammography, and breast self-examination. In: Lawrence RS, Goldbloom R, eds. Preventing Disease. New York, NY: Springer-Verlag NY Inc.; 1989:251–64.
U.S. Preventive Services Task Force. Guide to services. Clinical Preventive Services. 2nd ed. Baltimore, Md: Williams and Wilkins; 1996.
International Agency for Research on Cancer Working Group on Evaluation of Cervical Cancer Screening Programs. Screening for squamous cervical cancer: duration of low risk after negative results of cervical cytology and its implications for screening policies. BMJ. 1986;293:659–64.
Anderson LM, May DS. Has the use of cervical, breast and colorectal cancer screening increased in the United States? Am J Public Health. 1995;85:840–2.
Breen N, Kessler L. Trends in cancer screening—1987 and 1992. Oncology (Huntingt). 1996;3:328–30.
Hiatt RA, Pasick RJ. Unsolved problems in early breast cancer detection: focus on the under-served. Breast Cancer Res and Treatment. 1996;40:37–51.
Zapka JG. Promoting participation in breast cancer screening. Am J Public Health. 1994;84:12–3.
Zapka JG, Stoddard A, Maul L, Costanza ME. Interval adherence to mammography screening guidelines. Med Care. 1991;29:697–707.
Breast Cancer Screening Consortium NCI. Screening mammography: a missed clinical opportunity? Results of the NCI breast cancer screening consortium and National Health Interview Survey Studies. JAMA. 1990;264:54–8.
O’Malley AS, Mandelblatt J, Gold K, Cagney K, Kerner J. Continuity of care and the use of breast and cervical cancer screening services in a multi-ethnic community. Arch Intern Med. 1997;157:1462–70.
Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996;86:1748–54.
Bindman AB, Grunbach K, Osmond D, Vranizan K, Stewart A. Primary care and receipt of preventive services. J Gen Intern Med. 1996;11:260–76.
Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36:AS21–30.
Fox SA, Murata PJ, Stein JA. The impact of physician compliance on screening mammography for older women. Arch Intern Med. 1991;151:50–6.
Caplan LS, Wells BL, Haynes S. Breast cancer screening among older racial/ethnic minorities and whites: barriers to early detection. J Gerontol. 1992;47(Special Issue):101–10.
Harlem Study Team, Mandelblatt J, Traxler M, Lakin P, Kanetsky P, Kao R. Mammography and Papanicolaou smear use by elder poor black women. J Am Geriatr Soc. 1992;40:1001–7.
Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–96.
Blumenthal D, Mort E, Edwards J. The efficacy of primary care for vulnerable population groups. Health Serv Res. 1995;30:253–73.
Bastani R, Kaplan CP, Maxwell AE, Nisenbaum R, Pearce J, Marcus AC. Initial and repeat mammography screening in a low income multi-ethnic population in Los Angeles. Cancer Epidemiol Biomarkers Prev. 1995;4:161–7.
Richardson JL, Langholz B, Bernstein C, Burciaga C, Danley K, Ross RK. Stage and delay in breast cancer diagnosis by race, socioeonomic status, age and year. Br J Cancer. 1992;65:922–6.
Gann P, Melville SK, Luckmann R. Characteristics of primary care office systems as predictors of mammography utilization. Ann Intern Med. 1993;118:893–8.
HHS. The 1999 HHS Poverty Guidelines. Federal Register, Vol. 64, No. 52, March 18, 1999:13428–30. http://aspe.hhs.gov/poverty/99poverty.htm. Accessed February, 2000.
O’Malley AS, Forrest CB, O’Malley PG. Low-income women’s prioirites for primary care. J Fam Pract. 2000;49:141–6.
Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39.
Stewart AL, Ware JE, eds. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992.
Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socoeonomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA. 1998;279:1801–7.
National Health Interview Survey (NHIS). National Center for Health Statistics. www.cdc.gov/nchs/nhis.htm. Accessed January, 2000.
Perez-Stable EJ, Otero-Sabogal R, Sabogal F, Napoles-Springer A. Pathways to early cancer detection for Latinas: en accion contra el cancer. Health Educ Q. 1996;23:41S-59S.
American Cancer Society. Update Jan 1992: the American Cancer Society Guidelines for the Cancer-Related Checkup. CA Cancer J Clin. 1992;42:44–5.
Institute of Medicine. Primary Care: America’s Health in a New Era. Washington, D.C.: National Academy of Sciences; 1996.
Starfield B. Primary Care: Balancing health Needs, Services, and Technology. New York: Oxford University Press; 1998.
Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: John Wiley and Sons, Inc.; 1989.
SAS Institute Inc. Cary NC, Version 8.
Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1.
Kahn HA, Sempos CT. Statistical Methods in Epidemiology. New York: Oxford University Press; 1989.
Current Population Survey, March 1999 CPS Data. Annual Demographic Survey (March CPS Supplement) 1999 Methodology and Documentation. Washington, D.C.: U.S. Bureau of the Census; 1999.
Potosky AL, Breen N, Braubard BI, Parsons PE. The association between health care coverage and the use of cancer screening tests. Med Care. 1998;36:257–70.
Bernstein AB, Thompson GB, Harlan LC. Differences in rates of cancer screening by usual source of medical care. Med Care. 1991;29:196–209.
Phillips KA, Mayer ML, Aday LA. Barriers to care among racial/ethnic groups under managed care. Health Aff (Millwood). 2000;19:65–75.
Solanki G, Shauffler HH, Miller LS. The direct and indirect effects of cost-sharing on the use of preventive services. Health Serv Res. 2000;34:1331–50.
HCFA. Medicare and You: Medicare Preventive Services. Publication #HCFA-10110, Revised May 2000. www.medicare.gov/Basics. Accessed January, 2001.
Henson RM, Wyatt SW, Lee NC. The national breast and cervical cancer early detection program: a comprehensive public health response to two major health issues for women. J Public Health Manag Pract. 1996;2:36–47.
US Census for Washington, D.C. STF1. http://www.census.gov/hhes/www/housing/census/historic/phone.html. Accessed February, 2000.
Gordon NP, Hiatt RA, Lampert DI. Concordance of self-reported data and medical record audit for six cancer screening procedures. J Natl Cancer Inst. 1993;85:566–70.
Mandelson MT, LaCroix AZ, Anderson LA, Nadel MR, Lee NC. Comparison of self-reported fecal occult blood testing with automated laboratory records among older women in a health maintenance organization. Am J Epidemiol. 1999;150:617–21.
McGovern PG, Lurie N, Margolis KKL, Slater JS. Accuracy of self-report of mammography and pap smear in a low-income urban population. Am J Prev Med. 1998;14:201–8.
Fleiss JL. Statistical Methods for Rates and Proportions. New York: John Wiley and Sons; 1973.
www2.cdc.gov/nccdphp/brfss/age.asp/cat=WH&yr=34/2&state=DC. Accessed January, 2001.
Health Care Financing Administration. Medicare Denominator File. Washington, D.C.: Health Care Financing Administration; 1999.
Johnson NL. Letter from Rep. Nancy L. Johnson. Washington Post. October 27, 2000:A34.
Weisman CS. Women’s primary care. Health Aff (Millwood). 1997;16:276–7.
Teitelbaum MA, Weisman CS, Klassen AC, Celentano D. Pap testing intervals. Specialty differences in physicians’ recommendations in relation to women’s pap testing behavior. Med Care. 1988;26:607–18.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was funded in part by grant no. 17-97-1-7131 from the U.S. Department of the Army (ASO) and by grants RO3 CA83338-02 (ASO) and RO1 CA72908 (JM) from the National Cancer Institute.
Rights and permissions
About this article
Cite this article
O’Malley, A.S., Forrest, C.B. & Mandelblatt, J. Adherence of low-income women to cancer screening recommendations. J GEN INTERN MED 17, 144–154 (2002). https://doi.org/10.1046/j.1525-1497.2002.10431.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2002.10431.x