Abstract
The aims of this systematic review were to study the analgesic effect of real acupuncture and to explore whether sham acupuncture (SA) type is related to the estimated effect of real acupuncture for musculoskeletal pain. Five databases were searched. The outcome was pain or disability immediately (≤1 week) following an intervention. Standardized mean differences (SMDs) with 95% confidence intervals were calculated. Meta-regression was used to explore possible sources of heterogeneity. Sixty-three studies (6382 individuals) were included. Eight condition types were included. The pooled effect size was moderate for pain relief (59 trials, 4980 individuals, SMD −0.61, 95% CI −0.76 to −0.47; P < 0.001) and large for disability improvement (31 trials, 4876 individuals, −0.77, −1.05 to −0.49; P < 0.001). In a univariate meta-regression model, sham needle location and/or depth could explain most or all heterogeneities for some conditions (e.g., shoulder pain, low back pain, osteoarthritis, myofascial pain and fibromyalgia); however, the interactions between subgroups via these covariates were not significant (P < 0.05). Our review provided low-quality evidence that real acupuncture has a moderate effect (approximate 12-point reduction on the 100-mm visual analogue scale) on musculoskeletal pain. SA type did not appear to be related to the estimated effect of real acupuncture.
Similar content being viewed by others
Introduction
Musculoskeletal disorders and the related pain are major causes of disability in both developed and developing countries1. Neck pain (NP), low back pain (LBP), osteoarthritis (OA), rheumatoid arthritis (RA), lateral epicondylitis, fibromyalgia (FM) and myofascial pain (MP) are common in our society2,3,4. Although mortality from these conditions is generally low, they have a major effect on disability, medical costs and patient quality of life, largely due to the associated musculoskeletal pain5. As the population continues to increase in age, the influence of musculoskeletal disorders on society will also increase. Currently, there is limited understanding of the mechanisms that cause musculoskeletal pain and few therapies are available to treat musculoskeletal pain.
Acupuncture is commonly used for pain relief. The treatment is based on the theory that illness results from imbalances in energy flow, or qi and fine needles are inserted at specific points on the body to correct these imbalances and restore harmony6. The incidences of side effects and adverse events with acupuncture are lower than that with opioid analgesics and anti-inflammatory medications7. Acupuncture has been claimed to be effective for a wide range of conditions, such as pain, musculoskeletal disorders and several neurologic diseases8. Gate control theory and the release of endogenous opioids have been suggested as explanations for the apparent analgesic effect of acupuncture9,10,11. Acupuncture has both physiologic and psychological effects12,13 that are described as either specific or non-specific. The specific effects refer to the analgesic effects produced by needling a specific site at a proper depth for an appropriate duration and number of treatment sessions. The psychological non-specific effects are associated with patient perceptions, beliefs, experiences and expectations of patients. Therefore, sham acupuncture (SA) is needed to assess the specific effects of acupuncture. “Sham” or “placebo” is used to describe any control procedure that is used to blind treatment allocation in clinical trials of acupuncture14. Several sham procedures are now available, such as the use of penetrating acupuncture on non-acupoints, superficial penetration of the skin on acupoints and nonpenetration on acupoints with sham needle devices14.
Several reviews15,16,17 have evaluated the effects of acupuncture for musculoskeletal pain. However, all of them focused on only one disorder and almost all of them lacked analysis of the impact of SA type on the assessment of real acupuncture for musculoskeletal pain. Thus, we sought to analyze all previous studies of acupuncture for musculoskeletal pain that included a SA control group. Our objectives were to study the analgesic effect of real acupuncture and to explore whether SA type is related to the estimated effect of real acupuncture.
Methods
This systematic review was registered with number CRD42014010760 (http://www.crd.york.ac.uk/PROSPERO).
Criteria used to consider studies for this review
Types of studies
Only randomized clinical trials met our inclusion criteria. Both parallel and crossover studies were included. We included full articles with sufficient data for extraction, including the number of patients, the means and standard deviations for continuous outcomes in each group, and/or the number of patients in each group for dichotomous outcomes. There were no language restrictions.
Trials were excluded based on the following criteria: animal experiments, non-randomized or quasi-randomized (patients were allocated by registration number or date of birth) clinical trials, case report/series, news reports, letters, conference abstracts, or qualitative studies.
Types of participants
Patients suffering from pain associated with musculoskeletal disorders, defined broadly as pain that affects the muscles, ligaments and tendons and bones, were included. The following conditions related to musculoskeletal disorders were included: OA, NP, LBP, cervical spondylosis, whiplash, shoulder pain (SP), lateral epicondylalgia, FM, ankylosing spondylitis, RA, gouty arthritis and MP.
Patients with postoperative pain were excluded. Pregnant women with pelvic pain were also excluded.
Types of intervention
We pragmatically defined real (true, verus, genuine) acupuncture as an intervention in which needles were inserted into the skin at selected real acupuncture points at definite therapeutic depths. Trials with intervention groups that were treated with transcutaneous electrical nerve stimulation (TENS) or lasers were excluded.
Types of placebo
We defined SA as the use of “sham” or “placebo” needles. Sham groups exposed to sham TENS or lasers were excluded. We included trials that compared either acupuncture alone with SA alone or acupuncture plus one or more therapies with SA plus the same therapies.
Types of outcome measures
We only included studies that measured “follow-up pain or disability” immediately after the end of an intervention period (within 1 week) because studies with a shorter follow-up period would allow the detection of significant changes in pain. Our primary outcome was pain intensity (e.g., visual analogue scale, VAS; numerical rating scale, NRS; McGill Pain Questionnaire, MPQ). Our secondary outcome was disability (e.g., Oswestry Disability Index, ODI; Western Ontario and McMaster Universities Osteoarthritis (WOMAC) Index; Northwick Neck Pain Questionnaire, NPQ; Roland Morris Disability Questionnaire, RMQ). For each measurement, the closer the score was to 0, the more favorable the result.
Search methods for study identification
We conducted our systematic review in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline18. We searched the following databases: MEDLINE, EMBASE, the Cochrane Library, the Traditional Chinese Medical Literature Analysis and Retrieval System (TCMLARS), the China National Knowledge Infrastructure (CNKI) and the Wan Fang database. The search was conducted from the inception of each database. No language or date restriction was applied. The reference lists of the included trials and previous systematic reviews were systematically searched for citations of potentially eligible trials. The authors of the articles were contacted if there were any questions about the trials.
Our search strategies were iteratively developed using ‘acupuncture’, synonyms of ‘sham’, ‘randomized clinical trial’ and ‘musculoskeletal disorders’ (see supplementary file).
Data extraction, selection and coding
Identified studies were selected on the basis of titles and abstracts by two independent reviewers (QLY and MLY). Once a decision was made, full articles were checked. The kappa value statistic was used to measure agreement between the two reviewers. If there was any disagreement, either a consensus was reached or a third party (YGZ) became involved.
Two reviewers (QLY and LL) independently extracted the data from the studies using pilot-tested standardized data charts and disagreement was resolved by negotiation or a third party (PW). Missing information was collected by contacting the corresponding authors of the studies.
The duration of pain was defined as follows: (1) chronic (≥3 months), (2) sub-acute (~1–3 months) and (3) acute (<1 month).
Primary outcomes included pain intensity (e.g., VAS and NRS) and disability (e.g., ODI).
We extracted and analyzed only comparisons that were based on outcomes measured immediately after an intervention (≦1 week); measurements taken more than 1 week after the end of an intervention period were not included in the analysis. We preferred post-treatment data (at the immediate term, ≦1 week) because follow-up data (>1 week) may be more prone to bias due to patients leaving a trial, the diminution of the effect and the few studies reporting a longer follow-up period.
The study details (author and publication year), treatments, conditions (e.g., OA, NP and LBP), populations (demographic details) and outcome characteristics (including follow-up times) were summarized in tables.
The study (author and publication year), treatment, conditions (e.g., osteoarthritis, neck pain, low back pain), population (demographic details) and outcome characteristics (including follow-up times) were summarized in tables.
Specifically, the basic characteristics of acupuncture and SA were extracted according to Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA)19; these included theory of acupuncture, needle depth, needle location, name and number of acupoints selected, De Qi and number and duration of treatment sessions.
For randomized crossover trials, only data from the first period were included because of the carry-out effect.
Risk of bias (quality) assessment
Two reviewers (WTW and YSC) independently assessed the risk of bias in each study and discrepancies were resolved by discussion or consensus with a third party (FS or BBX). The quality of each individual trial was evaluated according to the criteria of the Cochrane Back Review Group20. There were 12 items in total and each item received 1 point for “yes” or 0 points for “unclear” or “no” (Supplementary Table S1). If the total score of a trial was equal to or larger than 6 points, the quality was considered high; a lower score would indicate low quality. The levels of agreement for each item and for the overall items were evaluated using the kappa value statistic.
Strategy for data synthesis
The results were grouped according to condition (e.g., NP, LBP and OA), pain persistence (e.g., acute, sub-acute, or chronic), SA type (e.g., needle depth or needle location) and trial location (based on continent).
The data were grouped into continuous and dichotomous variables and were pooled using a random effects model (DerSimonian-Laird method for standardized mean differences (SMDs), Mantel-Haenszel method for odds ratios (ORs)) to give a more conservative estimate of the effect of real acupuncture therapy on musculoskeletal disorders while allowing for any heterogeneity between studies. We preferred final values but used changes from baseline values only if these were the only available data. We preferred continuous data but used dichotomous data if the former were not available. We analyzed ordinal data as continuous data. If the means or standard deviations (SDs) were not reported and not available after contacting the authors, we used the data that were available, such as the median and its interquartile (IQR) or P values and confidence intervals, to calculate these values according to the methods recommended by the Cochrane Handbook, Version 5.1.021. If mean values were reported without SDs, the SDs of baseline data were used. Engauge Digitizer 3.0 (by Mark Mitchell) software was used to extract data from figures for studies in which exact data were not shown in the text or listed in tables. Data acquired with these methods were verified and only those data with the same direction of effect as the original article were included.
If the trials presented in a single paper included two or more real acupuncture arms or SA arms, the real acupuncture arms or SA arms were combined to avoid a unit-of-analysis error.
Heterogeneity between studies was evaluated using the I2 statistic with a cutoff point of ≥50% and a P value <0.10 on the χ2 test was defined as a significant degree of heterogeneity.
Random effects univariate and multivariate meta-regressions were used to explore the source of heterogeneity if possible; this was accomplished by fitting covariables to participant details (i.e., age, sex, continent, baseline pain, acupuncture-naïve status, condition and sample size); number of treatment sessions; treatment duration; sham needle location (i.e., same acupoints as real acupuncture, lateral to real acupoints and acupoints of different or irrelevant conditions); sham needle depth (i.e., non-penetrating, penetrating superficially, or penetrating normally); trial quality (i.e., allocation concealment, blinding, use of intention-to-treat (ITT) analysis and dropout rate of patients); and source of data (i.e., direct and indirect (from figures or calculated)). Then, all covariates were entered into a multivariate meta-regression model using a backward elimination approach with a removal criterion of P > 0.05. Additionally, continuous covariates were obtained from the meta-regression analyses to investigate whether relationships were linear and consistent with the results of the categorical analysis. The proportion of total between-study variances was explained by the models and reported as R2. We used meta-regression models to test between-subgroup interactions and a P value ≤0.05 indicated a significant difference.
Subgroup analyses were performed according to the source of heterogeneity or using covariates if possible. Condition type was used as the primary variable for the subgroup analyses.
Sensitivity analyses were performed to identify trials that disproportionately contributed to the observed heterogeneity. This was accomplished using jack-knife analysis, omitting each study one by one to assess its impact on the summary estimate. Galbraith plots were used to conduct a visual inspection of possible outlier studies that had excessive influence on the overall estimate. Metatrim analysis was used to explore possible missing trials to verify the robustness of the results after these trials were added.
Publication bias was explored using a contour-enhanced funnel plot and Egger’s test if there were up to 10 eligible studies included in the meta-analysis.
All results were shown with 95% confidence intervals. All analyses were performed with STATA 12.0 software (StataCorp LP, College Station, TX).
Best evidence synthesis
The clinical significance for the SMD was rated as small (<0.40), moderate (0.40 ~ 0.70) or large (>0.70) according to variation in Cohen’s interpretation of effect size22.
Based on the results of our systematic review, we used the GRADE system to rate the quality of the evidence23. The relative importance of each outcome was scored as critical to the decision (7–9), important but not critical to the decision (4–6), or not important to the decision (1–3). The quality of evidence for each outcome was scored as high, moderate, low, or very low (see Supplementary Tables S2 and S3). Although the evidence based on the included randomized controlled trials (RCTs) was initially rated as high quality, the quality could be downgraded based on the following five factors: study limitations, inconsistency, directness, preciseness, or reporting bias. Similarly, the quality could be upgraded based on three factors: large effect size, dose-response gradient, or plausible confounders that would have reduced the effect. Eventually, GRADEpro 3.6 software24 was used to compile and analyze the evidence.
Results
Literature search
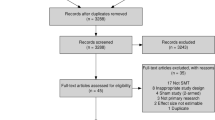
Our search strategy identified 3252 potentially eligible articles (Fig. 1). A total of 731 duplicates were excluded and 2205 additional records were also excluded based on their titles or abstracts for reasons such as not related to acupuncture or musculoskeletal disorders, not SA controlled, or not an RCT. After full-text articles were assessed for eligibility, 253 records were excluded for reasons such as irrelevance of the specified PICO (patient intervention comparison outcome), not an RCT, or in systematic review format. Eventually, 63 RCTs25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87 (6382 participants) were included in our systematic review. Of these, 61 (59 trials reporting pain and 31 reporting disability) reported continuous data and performed a meta-analysis and 240,42 reported pain as dichotomous data. The latter were also subjected to qualitative analysis. Fifty-nine trials that reported pain as continuous data were also included in the meta-regression. The kappa value for the agreement between reviewers (QLY and JTM) was 0.91, which indicated excellent agreement.
Study characteristics
All of the included studies were published between 1975 and 2013 (median 2007). The sample sizes ranged from 10 to 745 individuals (median 42, IQR 28 to 99, total 6382). Eight types of conditions were included: NP, SP, LBP, OA, RA, arm pain (AP), FM and MP (Table 1). The basic characteristics of the included trials are shown in Supplementary Table S4; the demographic characteristics are shown in Supplementary Table S5; the acupuncture and SA characteristics are shown in Supplementary Tables S6 and S7; the reasons for trial exclusion are shown in Supplementary Table S8; and the data conversion and data extraction from figures are shown in Supplementary Table S9.
Participant characteristics
The proportions of females ranged from 0% to 100% (median 70.3%). Six studies included only women, one included only men, 53 included both women and men and 3 did not report gender. The mean age ranged from 20.86 to 76.01 years (median 47.9) and all the participants were adults (age ≥18 years). Sixty-three studies reported the mean pain intensity at baseline, which ranged from 2.73 to 8.94 (median 6.05) on the VAS 10 cm. Four studies reported acute pain (<3 months, NP = 1, LBP = 3) from the duration of pain at baseline; others reported chronic pain (≥3 months).
Intervention characteristics
For all trials, there was a range of 1 to 24 treatment sessions (median 8, IQR 3.5 to 10); the total treatment periods ranged from 1 to 26 weeks (median 4, IQR 3 to 6); and the treatment frequencies ranged from 1 to 7 times/week (median 2, IQR 1 to 2). The most common treatment duration for each one-treatment session was 20 or 30 minutes. For some of the trials, the numbers of acupoints were not clearly reported, especially for individualized acupuncture groups in which the number of acupoints varied from patient to patient. Therefore, gross estimations were made on the basis of the descriptions included in the trial reports. The number of points ranged from 1 to 19 (median 9, IQR 4.7 to 12).
Sham acupuncture characteristics
Currently, SA is typically designed according to two factors: sham needle location (i.e., the same acupoints as real acupuncture, lateral to real acupoints, or acupoints of different or irrelevant conditions) and sham needle depth (i.e., non-penetration, superficial penetration, or normal penetration). After permutation and combination were calculated, eight SA types were identified. Twenty-five (39.7%) trials used a sham blunt needle with non-penetration at the same acupoints as in the intervention group.
Risk of bias and methodological design
The quality scores of all of the studies ranged from 4 to 11 (median 8, IQR 6 to 9) (Supplementary Table S10, Fig. 2). Sixteen studies were of low quality (score ≤6) and the remaining 47 studies were of high quality (score >6). The dropout rates ranged from 0% to 33.3% (median 3.84%, IQR 0% to 14.6%); 50 studies reported less than 15% attrition. Thirty-two studies carried out ITT analyses, 29 did not and 2 were unclear. Forty-nine studies reported their methods of randomization (computer or central call) and the other 14 trials were unclear. Thirty-three trials reported right allocation concealments (opaque seals and central call); the remaining 30 did not report this clearly. Fifty-five trials were double-blinded (patients and assessors were blinded); however, none of the studies had the caregivers blinded. Three of the included trials had a crossover design, while the others had a parallel design. One or more additional treatments, such as the use of non-steroidal anti-inflammatory drugs (NSAIDs), were added to both groups in many of the trials.
Risk of bias for the included studies.
Q, question. Q1, Was the method of randomization adequate? Q2, Was the treatment allocation concealed? Q3, Were the groups similar at baseline regarding the most important prognostic indicators? Q4, Was the patient blinded to the intervention? Q5, Was the care provider blinded to the intervention? Q6, Was the outcome assessor blinded to the intervention? Q7, Were co-interventions avoided or similar? Was the compliance acceptable in all groups? Was the dropout rate described and acceptable? Was the timing of the outcome assessment similar in all groups? Was intention-to-treat analysis included? Are reports of the study free from suggestion of selective outcome reporting?
Effects of acupuncture and meta-regression under different conditions
All conditions (overall summary effects)
After all of the trials were pooled, statistically significant differences in favor of the intervention group for both pain relief (59 trials, 4980 individuals, SMD −0.61, 95% CI, −0.76 to −0.47; P < 0.001) and disability improvement (31 trials, 4876 individuals, −0.77, −1.05 to −0.49; P < 0.001) were found and in both cases seemed to be of moderate to large clinical significance based on the variance of Cohen’s definitions. However, both cases showed significant heterogeneities (P < 0.001), with I2 values of 80.4% for pain and 94.7% for disability. Therefore, these analyses suggested that real acupuncture had a greater effect on pain relief and disability improvement than did SA. Forest plots (see Figures S1 and S2 in supplementary information file) were used to show the effect sizes, confidence intervals and proportion weightings in both pain and disability for individual trials and for all the trials pooled. The largest weightings for any individual trial were 2.49% for pain and 3.72% for disability. The number of trials that showed significant differences favoring real acupuncture over SA were 30 (50.85%) for pain and 13 (41.94%) for disability. One trial38 (Goldman 2008) reported that SA was superior to real acupuncture for pain associated with lateral epicondylitis. The subgroup and sensitivity analyses were shown in Table 2 (for pain) and Table 3 (for disability). The results of the meta-regression and the possible sources of heterogeneities for each individual pain condition were also summarized (Tables 4 and 5).
Neck pain
Six studies25,26,27,28,29,30 (n = 413) reported mean pain scores and were pooled with a moderate effect in favor of real acupuncture over SA (SMD −0.42, −0.62 to −0.22; P < 0.001) (Fig. 3) with no significant heterogeneity (I2 = 0%, P = 0.84).The jack-knife analysis did not change the results significantly. Egger’s test showed no evidence of publication bias (coefficient = −0.63; P = 0.39).
For disability, five studies25,27,28,29,30 (n = 368) were pooled and the SMD was −0.33 (−0.54 to −0.13, P = 0.002) (Fig. 4). This result indicated that real acupuncture had a small effect on disability improvement compared to SA. No significant heterogeneity was found (I2 = 0%, P = 0.979). The jack-knife analysis did not change the results significantly. Egger’s test suggested no evidence of publication bias (coefficient = −0.01; P = 0.99).
Shoulder pain
Five trials31,32,33,34,35 with a total of 495 participants compared mean pain scores between real acupuncture and SA. The SMD was −0.63 (−0.91 to −0.36, P < 0.001) (Fig. 5), indicating that there was a moderate effect favoring real acupuncture over SA. There was no evidence of significant heterogeneity (I2 = 34.9%, P = 0.19). The result was still robust after jack-knife analysis. No significant publication bias was found using Egger’s test (coefficient = −1.50; P = 0.23). We performed a meta-regression to explore the likely source of heterogeneity and found that sham needle location had an R2 of 100%, which indicated that this covariate could explain all the heterogeneity.
Two studies32,34 reported disability and were pooled (n = 129), with a SMD of −1.50 (−5.46 to 2.46). No significant difference was found between groups (P = 0.46). However, significant heterogeneity was shown (I2 = 96.1%, P < 0.001).
Neck pain and shoulder pain
Two studies36,37 (n = 58) reported pain intensity in patients with both NP and SP. We pooled the studies and found no significant difference between groups (SMD −0.52, −1.31 to 0.28; P = 0.20). The heterogeneity was not significant (I2 = 53.3%, P = 0.14).
We then pooled these two studies with the studies noted above that reported NP or SP, resulting in 13 trials (n = 966) with an SMD of −0.49 (−0.62 to −0.36, P < 0.001) (Fig. 6). This suggests that real acupuncture has a moderate effect on NP and SP compared to SA. All of the trials were statistically homogeneous (I2 = 0%, P = 0.47). The jack-knife analysis did not result in significant changes in the results. Both Egger’s test and the contour-enhanced funnel plot indicated no presence of publication bias (coefficient = −1.50; P = 0.23) (Fig. 7).
Low back pain
Ten studies41,43,45,46,47,48,49,50,51,52 (n = 1435) reported mean pain scores for LBP. The pooled SMD was −0.61 (−0.91 to −0.32, P < 0.001) (Fig. 8), which indicated a moderate effect favoring real acupuncture. However, the results were significantly heterogeneous (I2 = 79.2%, P < 0.001). The meta-regression identified sham needle depth (i.e., non-penetration, superficial penetration, or normal penetration) as the main source of the heterogeneity (R2 = 62.69%), explaining 62.69% of the heterogeneity. The pooled SMDs within the sham needle subgroups were −1.23 (−1.98 to −0.48) for non-penetration, −0.19 (−0.31 to −0.08) for superficial penetration and −0.50 (−0.85 to −0.14) for normal penetration. Publication bias was identified by Egger’s test (coefficient = −3.01; P = 0.003). Metatrim analysis found that two studies with positive effects favoring real acupuncture were missing. After these trials were filled, a larger effect was found (SMD −0.84, −1.26 to −0.42). A subgroup analysis was also performed according to condition duration (acute or chronic). Eight of these studies43,46,47,48,49,50,51,52 focused on chronic LBP, with a pooled SMD of −0.47 (−0.76 to −0.19, P = 0.001). This result indicated that real acupuncture was more effective than SA, but the effect decreased to moderate. The heterogeneity was still significant (I2 = 73.0%, P = 0.001) and sham needle depth was still the source of heterogeneity (R2 = 80.15%). The jack-knife analysis indicated that the results were robust. Egger’s test suggested publication bias (coefficient = −2.54; P = 0.01). Nevertheless, we conducted trim and fill analysis and no study was filled. This indicated that the publication bias had a non-significant effect on the results. One study47 (Itoh 2006) with a smaller sample size (n = 19) but a very large effect size (SMD = −3.43) was found to be the source of heterogeneity based on the Galbraith plot. After removing this study, the result was still robust (SMD −0.30, −0.45 to −0.15, P < 0.001) and significant heterogeneity (I2 = 22.6%, P = 0.26) was not found, although publication bias was present (coefficient = −1.67; P = 0.01). Two of these ten trials41,45 reported on acute LBP and both had a favorable result for real acupuncture. The pooled SMD was −1.07 (−2.11 to −0.02, P = 0.045). The heterogeneity was not significant (I2 = 22.6%, P = 0.26). In addition, one study42 reported on acute LBP with dichotomous data and no significant difference was found between groups (OR 1.19, 0.62 to 2.28, P = 0.61).
Eight trials41,42,44,45,46,47,49,51 (n = 1800) reported on disability in LBP, with a pooled SMD of −0.29 (−0.57 to −0.01, P = 0.04) (Fig. 9), which suggested that real acupuncture had a small effect compared to SA. However, heterogeneity was present (I2 = 83.5%, P < 0.001). The jack-knife analysis suggested the results changed significantly and removal of any one of the five individual trials could result in non-significance (P > 0.05). Five of these eight trials44,46,47,49,51 (n = 1536) reported disability in chronic LBP and non-significant differences were found between groups (SMD −0.15, −0.46 to 0.16, P = 0.34). The results were heterogeneous across trials (I2 = 83%, P < 0.001). Egger’s test suggested a publication bias (coefficient = −4.18; P = 0.01). The contour-enhanced funnel plot showed an asymmetry due to the small-study effect. We adjusted this bias by removal of the small study47 (n = 19) (Itoh 2006) and the publication bias was eliminated (coefficient = −3.64; P = 0.11), the heterogeneity was lowered (I2 = 66%, P = 0.03) and the pooled SMD was 0.00 (−0.20 to 0.20). For acute LBP, the remaining three studies41,42,45 (n = 264) achieved a pooled SMD of −0.50 (−1.05 to 0.05, P = 0.07), which suggested no significant difference between groups. However, significant heterogeneity was still present (I2 = 77.5%, P = 0.01).
Osteoarthritis
Fourteen studies53,54,55,56,57,58,59,60,62,63,64,65,66,67 (n = 1656) reported pain in patients with osteoarthritis (1 hip OA66, 12 knee, 1 both67). The pooled SMD was −0.77 (−1.12 to −0.41, P < 0.001) (Fig. 10), which indicated that real acupuncture had a larger effect on OA pain than SA. The jack-knife analysis showed the results were robust and had no significant change. However, there was high heterogeneity (I2 = 89.9%, P < 0.001). Univariate meta-regression was used to evaluate the continents on which the studies took place, the publication years and the sample sizes and we found that these factors could explain the heterogeneity with R2 values of 16.95%, 29.87% and 11.83%, respectively. Multivariate meta-regression indicated that these three covariates could explain the majority of the heterogeneity (R2 = 62.52%), suggesting that these covariates were the source of the heterogeneity. The contour-enhanced funnel plot suggested an asymmetry (Fig. 11) and Egger’s test indicated publication bias (coefficient = −3.71; P = 0.02). However, metatrim analysis found that no study was missing or should be added.
Twelve trials53,54,55,57,58,59,60,61,62,63,64,66 (n = 2256) reported on disability in OA (1 hip66, 11 knee) with a pooled SMD of −1.19 (−1.79 to −0.59, P < 0.001) (Fig. 12). This suggested that real acupuncture had a larger effect on individuals with OA than did SA. The jack-knife analysis found that the results did not change significantly on the removal of any individual study. However, a high heterogeneity was observed across these studies (I2 = 97.3%, P < 0.001). Univariate meta-regression indicated that sham needle location, pain at baseline (≥6 or <6) and an acupuncture-naive status (yes or unclear) had R2 values of 19.10%, 8.04% and 6.39%, respectively. We then assessed these three covariates using multivariate meta-regression and calculated a R2 of 51.68%, which indicated that these covariates could explain the majority of the heterogeneity. Asymmetry was observed in the contour-enhanced plot and evidence of publication bias was found with Egger’s test (coefficient = −6.92; P = 0.03). Metatrim analysis indicated that three trials with positive effects were missing (Fig. 13). Adding these trials into the pooling yielded a larger benefit from real acupuncture, with a pooled SMD of −1.61 (−2.46 to −0.77).
Temporomandibular joint pain (myofascial pain)
Thirteen studies75,76,77,78,79,80,81,82,83,84,85,86,87 (n = 414) were pooled to compare real acupuncture with SA in patients with MP. The real acupuncture showed a favorable effect on pain relief. The pooled SMD was −1.00 (−1.43 to −0.57, P < 0.001) (Fig. 14), with significant heterogeneity (I2 = 74.6%, P < 0.001). This result indicated that real acupuncture had a larger effect than SA. The removal of any one of the studies did not significantly affect the results, which had means ranging from −0.86 to −1.10 (P < 0.001) in the jack-knife analysis. We used univariate meta-regression to explore the likely source of heterogeneity and two covariates (sham needle location and depth) were identified with R2 values of 46.46% and 47.20%, respectively. We then assessed these two covariates with multivariate meta-regression and calculated an R2 of 99.52%. This suggested that these covariates could explain 99.52% of the heterogeneity. Egger’s test did not suggest publication bias (coefficient = −1.50; P = −0.23). However, it should be noted that no studies reported disability scores.
Fibromyalgia
Five studies70,71,72,73,74 (n = 631) were included for analysis of pain associated with FM. The pooled SMD was 0.01 (−0.35 to 0.37, P = 0.96) (Fig. 15), suggesting a non-significant difference between real acupuncture and SA. There was no evidence of significant heterogeneity (I2 = 39.3%, P = 0.16). Meta-regression indicated that sham needle depth could explain all of the heterogeneity (R2 = 100%). No evidence of publication bias was found using Egger’s test (coefficient = 0.75; P = −0.72). The jack-knife analysis indicated that the results did not change significantly.
Two studies72,73 (n = 163) were pooled for analysis of disability associated with FM, with a SMD of −0.38 (−0.72 to −0.05, P = 0.03). Non-significant heterogeneity was found (I2 = 0%, P = 0.35).
Lateral epicondylitis (tennis elbow or arm pain)
Two trials38,39 (n = 160) reported both pain and disability arising from lateral epicondylitis (tennis elbow), with non-significant SMDs of −0.18 (−1.33 to 0.97, P = 0.76) for pain and −1.63 (−5.37 to 2.11, P = 0.39) for disability. Both pain and disability had high heterogeneities, with I2 values of 90% and 98%, respectively. One trial39 (n = 118) (Fink 2002) showed a positive effect in favor of real acupuncture for both pain (SMD −0.80, −1.43 to −0.17) and disability (SMD −3.57, −4.56 to −2.58). However, another trial38 (Goldman 2008) (n = 42) reported that SA was superior to real acupuncture for pain relief (SMD 0.38, 0.01 to 0.74) and showed no difference for disability (SMD 0.25, −0.12 to 0.61). Additionally, one trial40 (n = 48) (Mosberger 1994) reported pain using dichotomous data, with an OR of 11.40 (2.95 to 44.00) favoring real acupuncture.
Rheumatic arthritis
Two studies68,69 (n = 76) investigated pain in patients with rheumatic disorders, with a SMD of −0.14 (−0.60 to 0.33, P = 0.57). No significant difference was found between the real and sham groups and no statistical heterogeneity was observed (I2 = 0%, P = 0.32). Disability was not reported.
Meta-regressions for exploring specific covariates for pain in overall conditions
Meta-regression of heterogeneity was possible only for the outcome of pain intensity, as it was our primary outcome measurement and was also more clinically relevant. The outcome of disability was reported in too few trials for the analysis to be robust and too few conditions for inclusive coverage of all the conditions. With regard to the number of SMDs used in each meta-regression, almost all the covariates were analyzed with 59 SMDs, but four of the covariates were excluded because some trials did not report data for these covariates (for example, one trial65 did not report data on age at baseline; therefore, only 58 SMDs were available for meta-regression analysis of age at baseline). These covariates were age at baseline (58 SMDs), pain at baseline (55 SMDs), proportion of females at baseline (56 SMDs) and sham needle depth (58 SMDs).
For univariate meta-regression of categorical covariates (Table 6), sample size of trial (<80 or ≥80) (R2 = 17.14%), year of publication (<2009 or ≥2009) (R2 = 10.48%), continent on which a trial was conducted (R2 = 6.79%), sham needle depth (R2 = 9.85%), sham needle location (R2 = 4.86%) and allocation concealment (R2 = 5.92%) appeared to be responsible for some of the heterogeneity in pain intensity. However, only three covariates (i.e., sample size of trial, year of publication and continent) showed significant differences in interactions between subgroups (P < 0.05). Regarding trial sample size, the SMD for the smaller sample size (<80) was 0.53 lower than that for the larger sample size (≥80) (P = 0.01). Regarding year of publication, the SMD for the past five years (≥2009) was 0.50 lower than that for previous years (<2009) (P = 0.02). Finally, regarding continent on which the trial was conducted, the SMD for Asia was 0.37 lower than that for Europe and 0.73 lower than that for America (P = 0.04). Additionally, for the sham needle depth or location, even though these two covariates could explain some heterogeneities, no significant difference was found between subgroups via these covariates (both sham needle depth and location) (P for interactions were 0.09 for sham needle depth and 0.19 for sham needle location) (Table 6). Consequently, the SA type seemed to be not related to the estimated effect of real acupuncture.
We analyzed the strengths of the linear associations between the intervention effects (SMD) on pain intensity and each of the continuous study-level covariates (i.e., year of publication, mean age, mean pain at baseline, treatment session, treatment duration, study quality, sample size and proportion of females). Year of publication explained 10.18% of the variation in effect sizes (P = 0.02): the SMD was an average of 0.03 lower for each 10-year increase in year of publication (coefficient = −0.033) (Fig. 16A). Treatment session explained 9.81% of the heterogeneity (P = 0.03): the SMD was 0.039 greater for each 1-treatment increase in treatment session (coefficient = 0.039) (Fig. 16B). However, this association was not significant across the sample sizes of trials (coefficient = 0.001, P = 0.054, R2 = 8.55%) (Fig. 16C). None of the other continuous covariates had a significant association with the sizes of the intervention effects (all P ≥ 0.17, R2 = 0.00%) (Fig. 17).
Overall publication bias
All the trials included in the meta-analyses were also included in the publication bias analyses (59 trials for pain, 31 trials for disability). For pain, the contour-enhanced funnel plot of the SMD showed a significant asymmetric scatter consistent with publication bias (Fig. 18A) (Egger’s test, coefficient = −2.23, P < 0.001). Nevertheless, we could not rule out the possibility of the small-study effect, as the asymmetry was attributable not only to three studies with small sample sizes and positive effects but also to one study54 (Mavrommatis 2012) with a larger sample size and a positive effect. We then performed metatrim analysis and found that three trials with positive effects were missing. After these three missing trials were filled, an even larger positive effect was found with a SMD of −0.68 (−0.84 to −0.53, P < 0.001). And these missing trials were likely to have had little effect on our findings, meaning that our result was still robust.
For disability, evidence of publication bias was also shown in the asymmetric contour-enhanced funnel plot (Fig. 18B) and in Egger’s test (coefficient = −4.79, P < 0.001). However, this bias could not be explained by the small-study effect because two larger studies54,62 (Witt 2005, Mavrommatis 2012) were also responsible for this bias. Metatrim analysis revealed that four trials with larger sample sizes and positive effects were missing; after these were filled, the difference favoring real acupuncture achieved an even greater positive effect with a SMD of −0.98 (−1.35 to −0.62, P < 0.001). This indicated that our results were still robust even with the presence of publication bias.
Rating of the evidence
Eight types of musculoskeletal disorders were included in our review. As pain was the critical outcome measurement, the evidence was rated on the basis of pain. The levels of GRADE evidence and the reasons for upgrade and downgrade were shown (Table 7). The evidence quality for the overall conditions was rated as low because there were obvious heterogeneities (clinical and statistical) and publication biases. The levels of evidence quality were high for NP and SP; moderate for LBP, MP and FM; low for OA; and very low for AP and RA.
Discussion
Key findings
Based on currently available evidence, our meta-analysis found that, overall, acupuncture was superior to SA in terms of pain relief and disability reduction for patients with musculoskeletal disorders. However, acupuncture was superior to SA for pain relief in only some of the individual conditions (chronic NP, SP, chronic LBP, OA and MP). There were no differences between the groups for FM, AP, or RA and we could not reach clear conclusion for acute NP, acute LBP, AP and RA for a small number of trials (≤2). For disability reduction, acupuncture was superior to SA in some conditions (chronic NP and OA), but there were no differences between groups for LBP and we could not reach clear conclusion regarding acute NP, SP, FM, AP and MP for a few trials (≤2).
In a univariate meta-regression model, for individual conditions, sham needle location and/or depth could explain most or all of the heterogeneities for some conditions (SP, LBP, OA, MF and FM), while other conditions were not applicable due to no heterogeneity (NP) or too few trials (RA and AP). For all conditions, a small portion of heterogeneity was explained by continent on which the study took place, year of publication, sample size, sham needle depth and location.
For sham needle depth or location, although these two covariates could explain some heterogeneity, no difference was found between subgroups via these covariates (both sham needle depth and sham needle location) (P for all interactions >0.05) (Tables 5 and 6). Consequently, SA type did not appear to be related to the estimated effect of real acupuncture.
We found a difference among the continent subgroups. The treatment effect in China was superior to that in other countries. The following speculations might account for this finding: acupuncture originated in China and was based on a set of relevant theories and practice experiences; and acupuncturists from China and adjacent countries usually had a five-year course of study. Additionally some other factors, such as psychological effect and publication bias, might also play a role in this difference.
The pooled SMD after 2009 was larger than it was before this date, which might have been the beneficial result of recent guidelines for quality control of acupuncture (STRICTA)19. This indicates that a good quality control of clinical acupuncture trial is needed.
Design of sham acupuncture
Acupuncture causes both specific effects (real therapeutic effects) and non-specific effects (placebo effects). The factors influencing these specific effects include individual condition, type of pain, treatment duration and session number, selection of acupoints, needle apparatus, depth and angle of needle insertion and quantity of stimulus88. The factors influencing the non-specific effects include patient responses to 1) being cared for and evaluated (i.e., the Hawthorne effect), 2) the use of placebo therapy and 3) the physician-patient relationship89,90,91. The above theory may also be applicable to SA.
Klaus Linde et al.92 conducted a systematic review of 61 clinical trials to compare the efficacy of SA (19 trials) with those of other placebos (42 trials, including pharmacological and other physical placebos). The results showed that SA had a larger effect than other placebos. Thus, we speculated that so-called SA might have a specific effect beyond the placebo effect (i.e., a psychological effect). It was very difficult to evaluate the size of the specific effect of SA compared to that of real acupuncture. In addition, for each SA type applied, the psychological effects of real acupuncture and SA should be assessed individually in case a test was partial to either party.
Hence, the ideal SA must meet two primary criteria in clinical acupuncture trials: 1) the presence of no or only a small specific effect, thereby removing the influence on the evaluation of the acupuncture effect; and 2) no difference or high similarity between all other aspects to allow successful implementation of blinding.
SA needle depth involves either superficial penetration or non-penetration. In the former, the needle is inserted approximately 2 mm into the skin, while the latter uses a blunt needle that contacts the skin without penetrating it.
In the theory of traditional Chinese medicine, superficial penetration is a type of acupuncture that can be adopted to overcome the limitations imposed by some anatomical structures, such as the head, wrist and ankle. Wu et al. found that superficial needling produced a good therapeutic effect for knee joint pain compared with routine acupuncture93. Likewise, superficial acupuncture was reported to be favorable for shoulder periarthritis by Lu and colleagues94. Additionally, Harris et al.70 found that superficial penetration stimulated specific regions of the brain and thereby had an analgesic effect. It is worth mentioning that, at the present time, the tissue layer or structure where acupuncture analgesia occurs and the functions of different tissue structures or layers in acupuncture analgesia remain unclear. It has been demonstrated that lightly touching the skin stimulates mechanoreceptors that are coupled to slow-conducting unmyelinated (C) afferents, resulting in activity in the insular region but not in the somatosensory cortex95. Activity in these C tactile afferents was deemed to induce a ‘limbic touch’ response, resulting in emotional and hormonal reactions. It is likely that control procedures in many acupuncture studies that were meant to be inert were in fact activating these C tactile afferents and, consequently, alleviating the affective component of pain95. Moreover, superficial acupuncture has yet to be strictly defined. Therefore, the decision to regard superficial acupuncture as a placebo is arbitrary.
The needling points used for non-penetration blunt-needle SA96 are different than those used in real acupuncture because the needles are not inserted into the skin and there are no small hemorrhagic spots that may be detected by patients undergoing SA. This may also affect the implementation of patient blinding. For instance, individuals with more experience undergoing acupuncture therapy or greater knowledge about acupuncture were more likely to correctly guess the type of needle they received at ST36 compared to other points97. Thus, patients included in trials should be acupuncture-naïve; in other words, they should neither have knowledge of nor have received acupuncture treatment. In addition, acupoints should be selected at locations that patients cannot see.
Another type of SA uses needling points above 1.5 cm lateral to therapeutic acupoints and out of the meridian system while maintaining essentially the same manipulation technique and needle-insertion depth (approximately 10–20 mm) as real acupuncture67. This type of SA was designed according to the theory that sham acupoints have no therapeutic effect and that the meridian system is an effective factor. Controlled clinical trials have indicated that both acupoints and non-acupoints can produce therapeutic effects67,98. The possible mechanisms for this include changes in local circular and immune functions and the triggering of neural pathways that lead to diffuse noxious inhibitory controls99,100. A functional MRI study identified different reaction zones between acupoint needling and non-acupoint needling101, but there were considerable overlaps among the brain signals that arose in reaction to different acupoints. These findings seem to illustrate that the specificity of an acupoint is relative and that, even if the specificity of an acupoint really exists, the precise acupoint used is not that important for acupuncture’s effect.
Overall, many deficiencies exist in the currently available SA designs. The optimal type of SA design remains unclear. Future trials should compare different SA designs directly to provide more conclusive evidence regarding the optimal type of SA design.
Comparison with other studies
Consistent with our current report, some previous systematic reviews have also found real acupuncture to be superior to SA for NP102, LBP102,103, OA104 and MP105. Two newly published meta-analyses106,107 found that real acupuncture had a more favorable effect than SA for LBP, with SMDs of −0.47107 and −0.58106. Our finding that real acupuncture was more effective than SA for NP and LBP was also verified by a more recent systematic review102.
We identified one trial38 (Goldman 2008) reporting that SA was superior to real acupuncture for pain associated with lateral epicondylitis. In the referenced trial, participants with persistent AP (N = 123) were randomly assigned to receive either real acupuncture or SA via 8 treatments over 4 weeks. A sham needle device (a blunt tip and retractable needle) was used. The reasons for the superiority of the SA device are not clear. One possibility is that the treatment effects were blunted in the real acupuncture group because of the higher rates of side effects, particularly mild pain during treatment. We speculate that this discomfort may have been due to the placement of needles in the arm that were in close proximity to the areas already experiencing pain.
Most side effects of acupuncture undergo spontaneous remission over several minutes or hours. Adverse reactions to acupuncture were rarely observed. Two prospective studies, with a total of 60,000 treatment sessions, did not find any serious side effects108,109. The total occurrence rate for meaningful minor side effects, including pain at acupuncture points, nausea and vomiting and dizziness or syncope, was less than 0.1%.
Strengths and weaknesses
A main strength of this study was its simultaneous assessment of acupuncture effectiveness (SA as the control group) in patients with almost all musculoskeletal disorders related to pain. This design provided a comprehensive review of the effects of acupuncture based on a registered number (CRD42014010760), using meta-regression analyses while considering possible sources of heterogeneity. Two independent reviewers extracted and analyzed the data and assessed the methodological quality. The majority of the studies were of high quality.
Moreover, our systematic review was conducted in strict accordance with the PRISMA statement18. The detailed characteristics of acupuncture or SA were extracted rigorously on the basis of the STRICTA statement19. Meta-regression was performed to explore possible sources of heterogeneity and to conduct indirect comparisons among subgroups. Metatrim analysis was conducted to sensitively assess publication bias. Furthermore, various statistical methods were employed according to Cochrane Handbook 5.1.0110 to convert existing data into available data, which eliminated possible selection bias. In particular, we conducted a meta-regression analysis of the characteristics of SA and found that differences in SA might not affect the evaluation of the effect size of acupuncture. At present, no other systematic review has used this approach.
The main weakness of this study was the relative paucity of high-quality RCTs. About half of the trials did not perform ITT analyses or correct allocation concealments. None of the studies blinded the caregivers because of the intrinsic characteristics of acupuncture. Furthermore, data on major clinical outcomes regarding pain for some conditions were available from only relatively few studies, especially for AP and RA (2 trials each). The small number of participating studies meant that the statistical power to detect differences was suboptimal. However, it remains possible that important differences exist in some conditions (i.e., NP, SP, LBP, OA and MP). Moreover, the patients in many of the trials received additional treatments while undergoing acupuncture, such as NSAIDs as needed. Although these additional interventions were available in almost all parallel groups, they might have been unbalanced between groups, potentially minimizing the effect size of the outcome. Furthermore, the vast majority of the included studies did not report side effects or only reported equivocally, making it difficult to evaluate the side effects.
Although the subgroup and meta-regression analyses explained certain variations between studies, they could not explain all of them and some variations were still unclear. Counter-enhanced funnel plots found small-study effects, which might have led to overrated effect sizes. On account of the relatively large number of a priori assumptions that were made, the reliability of the positive subgroup differences obtained should be lowered.
Finally, for patient-reported outcomes (e.g., pain and disability), patient expectations, preferences and satisfaction levels associated with treatment might have influenced the therapeutic effect or even acted as a dominant determinant111. However, almost none of the included studies evaluated and compared patient expectations between groups before or after acupuncture treatment.
Future research and ongoing trials
Future studies should put the STRICTA statement into greater effect, such as when evaluating the qualification and experience levels of acupuncturists. Moreover, close attention should be paid to two points: 1) candidate patients’ expectations, preferences and satisfaction levels associated with treatment should be taken into consideration112 and balanced between groups at baseline and 2) acupuncture should be compared with other non-pharmaceutical therapies. Moreover, future systematic reviews should evaluate the effect of acupuncture compared with SA and the optimum design of SA for all pain-related disorders. Additionally, future studies should try to identify an ideal SA based on the influential factors of acupuncture and consider all of these factors comprehensively to minimize the specific effects of SA.
Careful monitoring by acupuncturists, including observation of treatments and frequent meetings to support them throughout a trial, is necessary to maintain a high degree of quality control113. Although numerous outcome measurements had been developed that were relevant to musculoskeletal pain care, whether these measures were appropriate for use by acupuncturists is still unclear. Further studies are warranted to explore whether established outcome measurements are useful for evaluating musculoskeletal pain following acupuncture, such as for chronic LBP114.
Conclusion
Our review provided low-quality evidence that acupuncture has a moderate effect (approximately a 12-point pain reduction on the VAS 100 mm) on relieving pain associated with musculoskeletal disorders. Acupuncture was more effective than SA at relieving pain caused by chronic NP (high-level evidence), SP (high), chronic LBP (moderate), MP (moderate) and OA (low). There was no difference between groups for FM (moderate). There was not enough evidence for AP, RA, acute NP and acute LBP. The type of SA used did not seem to be related to the estimated effect of real acupuncture.
Additional Information
How to cite this article: Yuan, Q.-l. et al. Acupuncture for musculoskeletal pain: A meta-analysis and meta-regression of sham-controlled randomized clinical trials. Sci. Rep. 6, 30675; doi: 10.1038/srep30675 (2016).
References
Turk, D. C. & Melzack, R. Handbook of Pain Assessment 315–332 (The Guilford Press, New York, 1992).
Lawrence, R. C., Helmick, C. G. & Arnett, F. C. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum 41, 778–799 (1998).
Wolfe, F., Ross, K. & Anderson, J. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 38, 19–28 (1995).
Skootsky, S. A., Jaeger, B. & K., O. R. Prevalence of myofascial pain in general internal medicine practice. West J Med 151, 157–160 (1989).
Scudds, R. J. & Robertson, J. M. Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain 75, 229–235 (1998).
Kaptchuk, T. J. Acupuncture: Theory, efficacy and practice. Ann Intern Med 136, 374–383 (2002).
Ernst, E. & White, A. R. Prospective studies of the safety of acupuncture: A systematic review. Am J Med 110, 481–485, 10.1016/s0002-9343(01)00651-9 (2001).
Ernst, E., Pittler, M. H. & Wider, B. Complementary therapies for pain management: an evidence-based approach (Mosby Elsevier, Edinburgh (UK), 2007).
Han, J. S. Acupuncture and endorphins: mini review. Neurosci Lett 361, 258–261 (2004).
Melzack, R. Acupuncture and pain mechanisms. Anaesthesist 25, 204–207 (1976).
Melzack, R. & Wall, P. D. Pain mechanisms: a new theory. Science 150, 171–179 (1965).
Vincent, C. A. Acupuncture as a treatment for chronic pain. In Clinical research methodology for complementary therapies (eds Lewith, G. T. & Aldridge, D. ) 289–308 (Hodder and Stoughton, London, 1993).
Lewith, G. T. & Machin, D. On the evaluation of the clinical effects of acupuncture. Pain 16, 111–127 (1983).
Vincent, C. & Lewith, G. Placebo controls for acupuncture studies. J R Soc Med 88, 199–202 (1995).
Cao, L., Zhang, X. L., Gao, Y. S. & Jiang, Y. Needle acupuncture for osteoarthritis of the knee. A systematic review and updated meta-analysis. Saudi Med J 33, 526–532 (2012).
Selfe, T. K. & Taylor, A. G. Acupuncture and osteoarthritis of the knee: a review of randomized, controlled trials. Fam Community Health 31, 247–254, 10.1097/01.FCH.0000324482.78577.0f (2008).
Trinh, K. V. et al. Acupuncture for neck disorders. Cochrane Database Syst Rev, CD004870, 10.1002/14651858.CD004870.pub3 (2006).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, T. P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6, e1000097, 10.1371/journal.pmed.1000097 (2009).
MacPherson, H., Altman, D. G., Hammerschlag, R., Youping, L. & Taixiang, W. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT Statement. PLoS Med 7, e1000261, 10.1371/journal.pmed.1000261 (2010).
Furlan, A. D., Pennick, V., Bombardier, C. & van Tulder, M. updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 34, 1929–1941, 10.1097/BRS.0b013e3181b1c99f (2009).
Higgins, J. P. T. & Deeks, J. J. Chapter 7: Selecting studies and collecting data. In Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011] (eds Higgins, J. P. T. & Green, S. ) (The Cochrane Collaboration, 2011).
Cohen, J. Statistical Power Analysis in the Behavioral Sciences (2nd edition). (Lawrence Erlbaum Associates, Inc., Hillsdale (NJ), 1988).
Guyatt, G. H., Oxman, A. D. & Vist, G. E. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926, 10.1136/bmj.39489.470347.AD (2008).
GRADE Working Group. GRADE profiler 3.6 for Windows: The Grading of Recommendations Assessment, Development and Evaluation (short GRADE). McMaster University and Evidence Prime Inc., Ontario, Canada. URL http://www.gradeworkinggroup.org/ (2014).
Liang, Z., Zhu, X., Yang, X., Fu, W. & Lu, A. Assessment of a traditional acupuncture therapy for chronic neck pain: a pilot randomised controlled study. Complement Ther Med 19 Suppl 1, S26–S32, 10.1016/j.ctim.2010.11.005 (2011).
Sahin, N., Ozcan, E., Sezen, K., Karatas, O. & Issever, H. Efficacy of acupunture in patients with chronic neck pain–a randomised, sham controlled trial. Acupunct Electrother Res 35, 17–27 (2010).
Itoh, K., Katsumi, Y., Hirota, S. & Kitakoji, H. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement Ther Med 15, 172–179 (2007).
Zhu, X. M. & Polus, B. A controlled trial on acupuncture for chronic neck pain. Am J Chin Med 30, 13–28, 10.1142/s0192415x02000028 (2002).
Fu, W. B., Liang, Z. H., Zhu, X. P., Yu, P. & Zhang, J. F. Analysis on the effect of acupuncture in treating cervical spondylosis with different syndrome types. Chin J Integr Med 15, 426–430, 10.1007/s11655-009-0426-z (2009).
Tough, E. A., White, A. R., Richards, S. H. & Campbell, J. L. Myofascial trigger point needling for whiplash associated pain–a feasibility study. Man Ther 15, 529–535, 10.1016/j.math.2010.05.010 (2010).
Molsberger, A. F., Schneider, T., Gotthardt, H. & Drabik, A. German Randomized Acupuncture Trial for chronic shoulder pain (GRASP) - a pragmatic, controlled, patient-blinded, multi-centre trial in an outpatient care environment. Pain 151, 146–154, 10.1016/j.pain.2010.06.036 (2010).
Lathia, A. T., Jung, S. M. & Chen, L. X. Efficacy of acupuncture as a treatment for chronic shoulder pain. J Altern Complement Med 15, 613–618, 10.1089/acm.2008.0272 (2009).
Dyson-Hudson, T. A. et al. Acupuncture for chronic shoulder pain in persons with spinal cord injury: a small-scale clinical trial. Arch Phys Med Rehabil 88, 1276–1283, 10.1016/j.apmr.2007.06.014 (2007).
Guerra de Hoyos, J. A. et al. Randomised trial of long term effect of acupuncture for shoulder pain. Pain 112, 289–298, 10.1016/j.pain.2004.08.030 (2004).
Kleinhenz, J. et al. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendonitis. Pain 83, 235–241 (1999).
He, D., Veiersted, K. B., Hostmark, A. T. & Medbo, J. I. Effect of acupuncture treatment on chronic neck and shoulder pain in sedentary female workers: a 6-month and 3-year follow-up study. Pain 109, 299–307, 10.1016/j.pain.2004.01.018 (2004).
Nabeta, T. & Kawakita, K. Relief of chronic neck and shoulder pain by manual acupuncture to tender points–a sham-controlled randomized trial. Complement Ther Med 10, 217–222 (2002).
Goldman, R. H. et al. Acupuncture for treatment of persistent arm pain due to repetitive use: a randomized controlled clinical trial. Clin J Pain 24, 211–218, 10.1097/AJP.0b013e31815ec20f (2008).
Fink, M., Wolkenstein, E., Karst, M. & Gehrke, A. Acupuncture in chronic epicondylitis: a randomized controlled trial. Rheumatology (Oxford) 41, 205–209 (2002).
Molsberger, A. & Hille, E. The analgesic effect of acupuncture in chronic tennis elbow pain. Br J Rheumatol 33, 1162–1165 (1994).
Hasegawa, T. M., Baptista, A. S., de Souza, M. C., Yoshizumi, A. M. & Natour, J. Acupuncture for acute non-specific low back pain: a randomised, controlled, double-blind, placebo trial. Acupunct Med 32, 109–115, 10.1136/acupmed-2013-010333 (2013).
Vas, J. et al. Acupuncture in patients with acute low back pain: a multicentre randomised controlled clinical trial. Pain 153, 1883–1889, 10.1016/j.pain.2012.05.033 (2012).
Miyazaki, S., Hagihara, A., Kanda, R., Mukaino, Y. & Nobutomo, K. Applicability of press needles to a double-blind trial: a randomized, double-blind, placebo-controlled trial. Clin J Pain 25, 438–444, 10.1097/AJP.0b013e318193a6e1 (2009).
Cherkin, D. C. et al. A randomized trial comparing acupuncture, simulated acupuncture and usual care for chronic low back pain. Arch Intern Med 169, 858–866, 10.1001/archinternmed.2009.65 (2009).
Kennedy, S. et al. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med 16, 139–146, 10.1016/j.ctim.2007.03.001 (2008).
Haake, M. et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med 167, 1892–1898, 10.1001/archinte.167.17.1892 (2007).
Itoh, K., Katsumi, Y., Hirota, S. & Kitakoji, H. Effects of trigger point acupuncture on chronic low back pain in elderly patients–a sham-controlled randomised trial. Acupunct Med 24, 5–12 (2006).
Inoue, M. et al. Relief of low back pain immediately after acupuncture treatment–a randomised, placebo controlled trial. Acupunct Med 24, 103–108 (2006).
Brinkhaus, B. et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med 166, 450–457, 10.1001/.450 (2006).
Molsberger, A. F., Mau, J., Pawelec, D. B. & Winkler, J. Does acupuncture improve the orthopedic management of chronic low back pain–a randomized, blinded, controlled trial with 3 months follow up. Pain 99, 579–587 (2002).
Leibing, E. et al. Acupuncture treatment of chronic low-back pain – a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain 96, 189–196 (2002).
Mendelson, G. et al. Acupuncture treatment of chronic back pain: a double-blind placebo-controlled trial. Am J Med 74, 49–55 (1983).
Horng, H. C. et al. The effects of collateral meridian therapy for knee osteoarthritis pain management: a pilot study. J Manipulative Physiol Ther 36, 51–56, 10.1016/j.jmpt.2012.12.003 (2013).
Mavrommatis, C. I., Argyra, E., Vadalouka, A. & Vasilakos, D. G. Acupuncture as an adjunctive therapy to pharmacological treatment in patients with chronic pain due to osteoarthritis of the knee: a 3-armed, randomized, placebo-controlled trial. Pain 153, 1720–1726, 10.1016/j.pain.2012.05.005 (2012).
Suarez-Almazor, M. E. et al. A randomized controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider communication. Arthritis Care Res (Hoboken) 62, 1229–1236, 10.1002/acr.20225 (2010).
Lu, T. W. et al. Immediate effects of acupuncture on gait patterns in patients with knee osteoarthritis. Chin Med J (Engl) 123, 165–172 (2010).
Ahsin, S., Saleem, S., Bhatti, A. M., Iles, R. K. & Aslam, M. Clinical and endocrinological changes after electro-acupuncture treatment in patients with osteoarthritis of the knee. Pain 147, 60–66, 10.1016/j.pain.2009.08.004 (2009).
Jubb, R. W. et al. A blinded randomised trial of acupuncture (manual and electroacupuncture) compared with a non-penetrating sham for the symptoms of osteoarthritis of the knee. Acupunct Med 26, 69–78 (2008).
Itoh, K., Hirota, S., Katsumi, Y., Ochi, H. & Kitakoji, H. Trigger point acupuncture for treatment of knee osteoarthritis–a preliminary RCT for a pragmatic trial. Acupunct Med 26, 17–26 (2008).
Foster, N. E. et al. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. BMJ 335, 436, 10.1136/bmj.39280.509803.BE (2007).
Scharf, H. P. et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med 145, 12–20 (2006).
Witt, C. et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet 366, 136–143, 10.1016/s0140-6736(05)66871-7 (2005).
Vas, J. et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ 329, 1216, 10.1136/bmj.38238.601447.3A (2004).
Berman, B. M. et al. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med 141, 901–910 (2004).
Takeda, W. & Wessel, J. Acupuncture for the treatment of pain of osteoarthritic knees. Arthritis Care Res 7, 118–122 (1994).
Fink, M. G., Kunsebeck, H., Wipperman, B. & Gehrke, A. Non-specific effects of traditional Chinese acupuncture in osteoarthritis of the hip. Complement Ther Med 9, 82–89, 10.1054/ctim.2001.0442 (2001).
Gaw, A. C., Chang, L. W. & Shaw, L. C. Efficacy of acupuncture on osteoarthritic pain: A controlled, double-blind study. N Engl J Med 293, 375–378, 10.1056/nejm197508212930803 (1975).
Zanette Sde, A., Born, I. G., Brenol, J. C. & Xavier, R. M. A pilot study of acupuncture as adjunctive treatment of rheumatoid arthritis. Clin Rheumatol 27, 627–635, 10.1007/s10067-007-0759-y (2008).
Tam, L. S., Leung, P. C., Li, T. K., Zhang, L. & Li, E. K. Acupuncture in the treatment of rheumatoid arthritis: a double-blind controlled pilot study. BMC Complement Altern Med 7, 35, 10.1186/1472-6882-7-35 (2007).
Harris, R. E. et al. Traditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on mu-opioid receptors (MORs). Neuroimage 47, 1077–1085, 10.1016/j.neuroimage.2009.05.083 (2009).
Harris, R. E. et al. Dynamic levels of glutamate within the insula are associated with improvements in multiple pain domains in fibromyalgia. Arthritis Rheum 58, 903–907, 10.1002/art.23223 (2008).
Martin, D. P., Sletten, C. D., Williams, B. A. & Berger, I. H. Improvement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trial. Mayo Clin Proc 81, 749–757, 10.4065/81.6.749 (2006).
Harris, R. E. et al. Treatment of fibromyalgia with formula acupuncture: investigation of needle placement, needle stimulation and treatment frequency. J Altern Complement Med 11, 663–671, 10.1089/acm.2005.11.663 (2005).
Assefi, N. P. et al. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med 143, 10–19 (2005).
Tekin, L. et al. The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo-controlled trial. Clin Rheumatol 32, 309–315, 10.1007/s10067-012-2112-3 (2013).
Couto, C., de Souza, I. C., Torres, I. L., Fregni, F. & Caumo, W. Paraspinal Stimulation Combined With Trigger Point Needling and Needle Rotation for the Treatment of Myofascial Pain: A Randomized Sham-controlled Clinical Trial. Clin J Pain 30, 214–223, 10.1097/AJP.0b013e3182934b8d (2013).
Chou, L. W. et al. Remote therapeutic effectiveness of acupuncture in treating myofascial trigger point of the upper trapezius muscle. Am J Phys Med Rehabil 90, 1036–1049, 10.1097/PHM.0b013e3182328875 (2011).
Tsai, C. T. et al. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil 89, 133–140, 10.1097/PHM.0b013e3181a5b1bc (2010).
Sun, M. Y. et al. The therapeutic effects of acupuncture on patients with chronic neck myofascial pain syndrome: a single-blind randomized controlled trial. Am J Chin Med 38, 849–859, 10.1142/s0192415x10008299 (2010).
Shen, Y. F., Younger, J., Goddard, G. & Mackey, S. Randomized clinical trial of acupuncture for myofascial pain of the jaw muscles. J Orofac Pain 23, 353–359 (2009).
Chou, L. W., Hsieh, Y. L., Kao, M. J. & Hong, C. Z. Remote influences of acupuncture on the pain intensity and the amplitude changes of endplate noise in the myofascial trigger point of the upper trapezius muscle. Arch Phys Med Rehabil 90, 905–912, 10.1016/j.apmr.2008.12.020 (2009).
Shen, Y. F. & Goddard, G. The short-term effects of acupuncture on myofascial pain patients after clenching. Pain Pract 7, 256–264 (2007).
Goddard, G., Karibe, H., McNeill, C. & Villafuerte, E. Acupuncture and sham acupuncture reduce muscle pain in myofascial pain patients. J Orofac Pain 16, 71–76 (2002).
Birch, S. & Jamison, R. N. Controlled trial of Japanese acupuncture for chronic myofascial neck pain: assessment of specific and nonspecific effects of treatment. Clin J Pain 14, 248–255 (1998).
McMillan, A. S., Nolan, A. & Kelly, P. J. The efficacy of dry needling and procaine in the treatment of myofascial pain in the jaw muscles. J Orofac Pain 11, 307–314 (1997).
Smith, P., Mosscrop, D., Davies, S., Sloan, P. & Al-Ani, Z. The efficacy of acupuncture in the treatment of temporomandibular joint myofascial pain: a randomised controlled trial. J Dent 35, 259–267, 10.1016/j.jdent.2006.09.004 (2007).
Diracoglu, D., Vural, M., Karan, A. & Aksoy, C. Effectiveness of dry needling for the treatment of temporomandibular myofascial pain: a double-blind, randomized, placebo controlled study. J Back Musculoskelet Rehabil 25, 285–290, 10.3233/bmr-2012-0338 (2012).
Guo, Y. Experimental Acupuncture. 239–249 (Chinese Press of Traditional Chinese Medicine, Beijing, 2010).
Miller, F. G. & Kaptchuk, T. J. The power of context: reconceptualizing the placebo effect. J R Soc Med 101, 222–225, 10.1258/jrsm.2008.070466 (2008).
Hrobjartsson, A. What are the main methodological problems in the estimation of placebo effects. J Clin Epidemiol 55, 430–435 (2002).
Kaptchuk, T. J. Powerful placebo: the dark side of the randomized controlled trial. Lancet 351, 1722–1725 (1998).
Linde, K., Niemann, K. & Meissner, K. Are sham acupuncture interventions more effective than (other) placebos? A re-analysis of data from the Cochrane review on placebo effects. Forsch Komplementmed 17, 259–264, 10.1159/000320374 (2010).
Wu, Y. Y. & Liao, J. P. Treatment of knee joint pain with superficial needling. Zhongguo Zhen Jiu 25, 261–262 (2005).
Lu, J. et al. Transient therapeutic effect and safety of superficial needling therapy for treatment of periarthritis of shoulder. Zhongguo Zhen Jiu 28, 414–416 (2008).
Lund, I. & Lundeberg, T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med 24, 13–15 (2006).
Streitberger, K. Inroducing a placebo needle into acupuncture research. Lancet 352, 364–365 (1998).
Lee, H. et al. Non-penetrating sham needle, is it an adequate sham control in acupuncture research? Complement Ther Med 19 Suppl 1, S41–S48, 10.1016/j.ctim.2010.12.002 (2011).
Richardson, P. H. & Vincent, C. A. Acupuncture for the treatment of pain: a review of evaluative research. pain 24, 15–40 (1986).
Le Bars, D., Villaneuva, L. & Bouhassira, D. Diffuse noxious inhibitory control (DNIC) in animals and in man. Patol Fiziol Eksp Ter 1992, 4 (1992).
Stewart, D., Thompson, J. & Oswald, I. Acupuncture analgesia: an experimental investigation. BrMed J 1, 67–70 (1977).
Fang, J. L., Krings, T., Weidemann, J., Meister, I. G. & Thron, A. Functional MRI in healthy subjects during acupuncture: different effects of needle rotation in real and false acupoints. Neuroradiology 46, 359–362, 10.1007/s00234-003-1125-7 (2004).
Yuan, Q. L., Guo, T. M., Liu, L., Sun, F. & Zhang, Y. G. Traditional Chinese medicine for neck pain and low back pain: a systematic review and meta-analysis. PLoS One 10, e0117146, 10.1371/journal.pone.0117146 (2015).
Lam, M., Galvin, R. & Curry, P. Effectiveness of acupuncture for nonspecific chronic low back pain: a systematic review and meta-analysis. Spine 38, 2124–2138, 10.1097/01.brs.0000435025.65564.b7 (2013).
Muramatsu, S. Acupuncture and knee osteoarthritis. Ann Intern Med 146, 147, author reply 148–149 (2007).
Kietrys, D. M. et al. Effectiveness of Dry Needling for Upper-Quarter Myofascial Pain: A Systematic Review and Meta-analysis. J Orthop Sports Phys Ther 43, 620–634, 10.2519/jospt.2013.4668 (2013).
Manheimer, E., White, A., Berman, B., Forys, K. & Ernst, E. Meta-analysis: acupuncture for low back pain. Ann Intern Med 142, 651–663 (2005).
Furlan, A. D. et al. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev CD001351, 10.1002/14651858.CD001351.pub2 (2005).
White, A., Hayhoe, S., Hart, A., Ernst, E. & BMAS and AACP. Survey of adverse events following acupuncture (SAFA): a prospective study of 32,000 consultations. Acupunct Med 19, 84–92 (2001).
MacPherson, H., Thomas, K. & Walters, S. The York acupuncture safety study: prospective survey of 34000 treatments by traditional acupuncturists. BMJ 323, 486–487 (2001).
Higgins, J. P. T. & Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. (The Cochrane Collaboration, 2011).
George, S. Z. & Robinson, M. E. Preference, expectation and satisfaction in a clinical trial of behavioral interventions for acute and sub-acute low back pain. J Pain 11, 1074–1082, 10.1016/j.jpain.2010.02.016 (2010).
Linde, K. et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain 128, 264–271, 10.1016/j.pain.2006.12.006 (2007).
McManus, C. A. et al. Experiences of acupuncturists in a placebo-controlled, randomized clinical trial. J Altern Complement Med 13, 533–538, 10.1089/acm.2007.6309 (2007).
Stomski, N. J., Mackintosh, S. & Stanley, M. Acupuncturists’ perspectives on outcome measures to evaluate acupuncture care for chronic low back pain. Complement Ther Med 18, 28–41, 10.1016/j.ctim.2009.11.002 (2010).
Acknowledgements
This study was supported by grants (No. 81371987 and 81171761) from the National Natural Science Foundation of China and the China Scholarship Council. We thank Prof. Xiong Guo, Key Laboratory of Environment and Genes Related to Disease of Education Ministry, Medical College of Xi’an Jiaotong University, for providing important assistance with statistical analysis.
Author information
Authors and Affiliations
Contributions
Q.-l.Y. and P.W. were responsible for study conception and design, acquisition of data, analysis and interpretation of data and drafting the manuscript. Y.-g.Z., F.S. and B.-b.X. critically revised the manuscript for important intellectual content. L.L., M.-l.Y. and J.-t.M. were responsible for the analysis and interpretation of data. W.-t.W. and Y.-s.C. were responsible for study conception and design; acquisition, analysis and interpretation of data; and critical revision of the manuscript for important intellectual content. All authors read and approved the final version of the manuscript and had full access to all of the data in the study.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Yuan, Ql., Wang, P., Liu, L. et al. Acupuncture for musculoskeletal pain: A meta-analysis and meta-regression of sham-controlled randomized clinical trials. Sci Rep 6, 30675 (2016). https://doi.org/10.1038/srep30675
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep30675
This article is cited by
-
Factors and Their Impact on Treatment Effect of Acupuncture in Different Outcomes: A Meta-Regression of Acupuncture Randomized Controlled Trials
Chinese Journal of Integrative Medicine (2024)
-
Acupuncture for post-stroke depression: a systematic review and meta-analysis
BMC Complementary Medicine and Therapies (2021)
-
Effectiveness of acupuncture on anxiety disorder: a systematic review and meta-analysis of randomised controlled trials
Annals of General Psychiatry (2021)
-
Acupuncture is ineffective for chronic low back pain? A critical analysis and rethinking
Frontiers of Medicine (2021)
-
A critical examination of the main premises of Traditional Chinese Medicine
Wiener klinische Wochenschrift (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.