Abstract
Study design:
Mail survey of participants with incomplete spinal cord injury (SCI).
Objective:
To describe the incidence, circumstances, consequences, and perceived contributory factors associated with falls among ambulatory individuals with incomplete SCI.
Setting:
Southeast region of the United States.
Methods:
A survey instrument was developed largely from existing measures and mailed to individuals with incomplete SCI to collect self-reported information on participant characteristics and fall-related variables.
Results:
Seventy-five percent of study participants sustained at least one fall over the previous year. Even though most injuries were minor, 18% of fallers sustained a fracture and 45% reported reduced ability to get out into the community and engage in productive activity. Factors perceived to contribute to falls most often were decreased strength in the trunk and lower extremities, loss of balance, and hazards in the environment.
Conclusions:
Falls occur frequently and often have significant consequences among ambulatory individuals with SCI. These data may assist rehabilitation professionals to identify those at risk and implement fall prevention strategies.
Sponsorship:
This project was supported by a grant from the South Carolina Spinal Cord Injury Research Fund Grant # 0703.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (SCI) results in immediate and generally permanent changes in sensory and motor functioning, the extent of which depends on the level and neurological completeness of the injury. In some cases, individuals with neurologically incomplete injuries are able to ambulate.1 However, the quality and degree of ambulation may be affected by spasticity, muscle weakness, and coactivation of muscle groups.2 Ambulatory ability may be further impacted as individuals age by declines in the neurologic, musculoskeletal, and cardiovascular systems.3, 4, 5 Thus, ambulation is frequently limited to certain conditions such as within the home, for shorter distances, or with the support of an assistive device.
In a recent study of 1328 persons with traumatic SCI, ambulatory individuals were found to have the highest rate of subsequent injuries due to a variety of causes, including falls.6 Thus, impaired balance or gait may have contributed to the greater occurrence of injuries in this group. Alcohol and prescription drug misuse, which can further affect balance and gait, were also found to be associated with elevated risk for subsequent injuries. Although falls may have accounted for a number of injuries, this study considered injuries due to a variety of causes and did not address falls exclusively.
While falls have not been studied specifically in individuals with SCI, they are a primary health concern among older adults in the general population. Major injuries, including head trauma, soft tissue injuries, fractures, and dislocations, may occur due to a fall; fractures account for 75% of serious injuries.7 Hip fractures cause the most significant health problems8 and may result in the individual being unable to return home and live independently.9 Falls can also lead to a fear of falling and restriction of activity because of fear.10
As a result of the potentially serious consequences of falls, a better understanding of falls and related factors among individuals with incomplete SCI may assist health care professionals to identify individuals at risk and develop interventions to prevent injury. The purpose of this study, therefore, was to examine the incidence, circumstances, consequences, and factors associated with falls among a community sample of ambulatory persons with incomplete SCI.
Methods
Participants
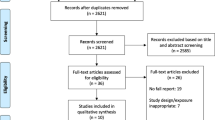
The sample was identified from outpatient files of persons from a large free-standing specialty hospital in the Southeastern United States, who took part in a previous study of subsequent injuries.6 To participate in this study, participants had to meet the following criteria: (1) a traumatic incomplete SCI; (2) ability to ambulate independently for a minimum of 10 m with or without an assistive device; (3) a minimum of one year post-SCI; and (4) age 18 years or older at the time of the study. Of the 281 individuals from the initial study who met the inclusion criteria, 59 could not be located and one was deceased, which reduced the working sample to 221. One hundred and nineteen out of 221 individuals completed the questionnaire, for a response rate of 54%.
Procedure
Prospective participants were sent a letter to explain the purpose of the study and to alert them that a questionnaire on falls and related injuries would be forthcoming. A cover letter, with all of the elements of informed consent, and a survey instrument were mailed 4–6 weeks later. Participants were asked to return the questionnaire within 2 weeks. Nonrespondents received a follow-up mailing if the completed questionnaire was not received after 4 weeks. Participants were offered a $20 incentive to complete the instrument. All procedures were approved by the Institutional Review Boards of the collaborating institutions.
Instrument
A questionnaire was developed through consolidation of several measures and the addition of fall-related items. For the purpose of this study, a fall was defined as an unplanned, unexpected contact with the supporting surface.11 The consolidation of several measures was necessitated by absence of appropriate existing measures as available instruments are performance based and include tests such as the Timed Up and Go;12 Berg Balance Scale;13 and Performance Oriented Mobility Assessment.14 Items were selected from the Falls Assessment Questionnaire15 and the Behavioral Risk Factor Surveillance System (BRFSS),16 a national survey aimed at gathering information on health behaviors of adults. Other items elicited information on medical conditions, medication usage, history of falls, and the nature and severity of fall-related injuries. Participants were asked to rate factors perceived to be associated with a fall on a scale of 1–5, with a score of 1 used to indicate that the factor was not at all related to the fall and 5 to indicate the factor was entirely responsible for the fall.
This questionnaire was developed with the assistance of an expert from the Survey Research Unit of a Southeastern medical university and feedback from experts in the field of physical therapy. It was then pilot tested on a small sample of persons with SCI in order to determine if questions were unclear, incomplete, or misleading and to solicit suggestions for any additional questions that should be included. Further revisions to the questionnaire were made based on feedback from this group. Closed-ended questions were used, which required the respondent to select from among several choices.
Analysis
Descriptive statistics were determined for demographic information, SCI characteristics, health and physical activity data, and incidence of falls for all respondents. Frequency distributions were then determined for factors perceived by the participant to be related to a fall. All calculations were performed using SAS software.17
Results
Participant characteristics
The average age of the study participants was 51.6 years (SD=13.93). The majority of individuals (69%) were male, and most participants (74%) were Caucasian. More than half (54%) of the participants were married, and 71% lived with a spouse of other caregiver. Fifty-six percent of this sample had completed at least some college, and 55% had an annual household income of at least $25000.
The average number of years since the SCI was 13.6 (SD=5.94). Most of the participants (52%) sustained their injury in a motor vehicle accident or from a fall or flying object (28%). Of the study sample, 47% sustained a cervical injury, 36% a thoracic injury, and 17% a lumbar injury. Seventy-eight percent of participants reported full movement in the upper extremities and hands. Seventy percent of participants reported that they ambulated in the community and 71% of participants were able to negotiate stairs.
Falls history
Seventy-five percent of the study participants sustained at least one fall over the previous year. The location of the majority of falls was in the home, and the time of day when most falls occurred was during the afternoon or evening (Table 1). Less severe injuries such as bruises, scrapes, and cuts occurred most frequently followed by muscle/ligament strain or sprain. However, 18% of fallers sustained a fracture as a result of a fall and 45% reported that falls restricted their ability to get out into the community and engage in productive activity.
Factors perceived by the study participants to contribute to falls most often were decreased strength in the trunk and lower extremities, loss of balance, and hazards in the environment (Table 2). Factors such as alcohol or prescription medication use were not perceived to be related to falls.
Discussion
Although this study was descriptive in nature, the results indicate that falls are an important consideration for ambulatory individuals with incomplete SCI both in terms of frequency and consequence. The incidence of falls (75%) was substantially higher than the incidence reported for healthy individuals age 65 and older, which ranges between 25 and 35%.10, 18 Even though fall rates as high as 40–50% are reported for frail, institutionalized elderly age 80 and older,19 these rates are lower than for our sample of ambulatory individuals with incomplete SCI. The incidence of falls for those with incomplete SCI are also greater than those for individuals with neurological diseases such as peripheral neuropathy (50%)20 and Parkinson's disease (38–62%).21, 22
For individuals with incomplete SCI, the location where the majority of falls occurred was in the home, and the frequency of falls increased throughout the day. The incidence of fractures (18%) exceeded that reported in studies of healthy older adults (510–6%23) suggesting a much greater consequence of falls in this population. This is furthered evidenced by declines in ability to engage in community and productive activities among almost half (45%) of the participants.
Implications
This study suggests that falls are a significant problem among ambulatory persons with SCI, both in terms of frequency and consequence. Given that ambulation is a highly coveted goal after SCI, rehabilitation professionals may not fully address safety issues. This demonstrates the need to incorporate falls history and specific clinical tests and measures into the examination of these individuals to better identify the particular factors that may be associated with falls. Laboratory assessment of balance and gait would provide additional objective data that would allow an even better analysis of the factors contributing to falls among individuals with incomplete SCI. This information could then be used to design interventions to remediate identified deficits and potentially reduce the incidence of falls and subsequent injuries.
Limitations
There are several noteworthy limitations in this study. First, all data are self-report. Data from observance of actual behaviors or from diaries updated on a regular basis may have identified a somewhat different incidence of falls. However, we selected a relatively short timeframe to minimize recall bias. Second, there were a large number of nonresponders. Selective attrition/response could affect the overall estimate of the incidence of falls and would depend on the differences between responders and nonresponders. Third, participants were selected from a specialty hospital rather than a population based cohort. However, the specialty hospital captures 85% of all SCI persons within that state, suggesting that a population-based cohort would have had only modest effects on the results.
Future research
Whereas this study was the first to identify basic epidemiologic information on falls, further research is needed to pinpoint risk and protective factors for falls. Clinical and laboratory examination of balance and gait may also augment information obtained through self-report.
References
Crozier K, Graziani V, Ditunno J, Herbison G . Spinal cord injury: Prognosis for ambulation based on sensory examaintaion in patients who are initially motor complete. Arch Phys Med Rehabil 1991; 72: 119–121.
Winter DA . The Biomechanics and Motor Control of Human Gait. University of Waterloo Press: Warterloo, Canada 1987.
Little JW, Burns SP, James JJ, Stiens SA . Neurologic recovery and neurologic decline after spinal cord injury. Top Spinal Cord Inj Med 2000; 11: 73–89.
Goldstein B . Musculoskeletal conditions after spinal cord injury. Top Spinal Cord Inj Med 2000; 11: 91–108.
Bauman WA, Raza M, Spungen AM, Machac J . Cardiac stress testing with thallium-201 imagining reveals silent ischemia in individuals with paraplegia. Arch Phys Med Rehabil 1994; 75: 946–950.
Krause JS . Factors associated with risk for subsequent injuries after traumatic spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1503–1508.
King MB, Tinetti ME . A multifactorial approach to reducing injurious falls. Clin Geriatr Med 1996; 12: 745–759.
Barancik JI et al. Northeastern ohio trauma study: I. Magnitude of the problem. Am J Public Health 1983; 73: 746–751.
Scott JC . Osteoporosis and hip fractures. Rheum Disease Clin North Am 1990; 16: 717–740.
Tinetti ME, Speechley M, Ginter SF . Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319: 1701–1706.
Shumway-Cook A, Woollacott MH . Motor Control: Theory and Practical Applications. Williams and Wilkins: Baltimore, MD 1995, pp 119–143.
Podsiadlo D, Richardson S . The timed ‘up and go’: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–148.
Berg KO, Wood-Dauphinee SL, Williams JT, Gayton D . Measuring balance in the elderly: Preliminary development of an instrument. Physiother Can 1989; 41: 304–311.
Tinetti ME . Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 1986; 34: 119–126.
Rapport LJ et al. Predictors of falls among right hemisphere stroke patients in the rehabilitation setting. Arch Phys Med Rehabil 1993; 74: 621–626.
Centers for Disease Control and Prevention (CDC). Overview Behavioral Risk Factor Surveillance System (BRFSS) 2002, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, Georgia. Available at:. http://www.cdc.gov/brfss/technical_infodata/surveydata/2002.htm.
SAS [Computer Software]. Statistical Software: Cary, NC 2004.
Prudham D, Evans J . Factors associated with falls in the elderly: a community study. Age Ageing 1981; 10: 141–146.
Campbell AJ, Borrie MJ, Spears GF . Risk factors for falls in a community based prospective study of people 70 years and older. J Gerontol A Biol SCi Med Sci 1989; 44: M112–M117.
Richardson JK, Hurvitz EA . Peripheral neuropathy: a true risk factor for falls. J Gerontol A Biol Sci Med Sci 1995; 50: M211–M215.
Stack E, Ashburn A . Fall events described by people with Parkinson's disease: implications for clinical interviewing and research agenda. Physiother Res Intl 1999; 4: 190–200.
Hirsh MA, Toole T, Maitland CG, Rider RA . The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson's disease. Arch Phys Med Rehabil 2003; 84: 1109–1117.
Gryfe CI, Aimes A, Ashley MJ . A longitudinal study of falls in an elderly population; 1: incidence and morbidity. Age Ageing 1977; 6: 201–210.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Brotherton, S., Krause, J. & Nietert, P. Falls in individuals with incomplete spinal cord injury. Spinal Cord 45, 37–40 (2007). https://doi.org/10.1038/sj.sc.3101909
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101909
Keywords
This article is cited by
-
Zoledronic acid after spinal cord injury mitigates losses in proximal femoral strength independent of ambulation ability
Osteoporosis International (2023)
-
Design and Fabrication of a Passive Pelvic Orthosis for Treadmill Walking Rehabilitation
Journal of Bionic Engineering (2023)
-
Impaired foot placement strategy during walking in people with incomplete spinal cord injury
Journal of NeuroEngineering and Rehabilitation (2022)
-
Meaningful measurements of maneuvers: People with incomplete spinal cord injury ‘step up’ to the challenges of altered stability requirements
Journal of NeuroEngineering and Rehabilitation (2021)
-
Feasibility and tolerance of a robotic postural training to improve standing in a person with ambulatory spinal cord injury
Spinal Cord Series and Cases (2021)