Abstract
Study design: Cohort study with 6-years follow-up.
Objective: To describe the utilization of health services by persons with spinal cord injury (SCI) and compare it with that of the general population.
Setting: Alberta, Canada.
Methods: All persons who sustained an SCI in Alberta between April 1992 and March 1994 were followed from date of injury to 6 years postinjury. Cases were matched (1:5) with controls randomly selected from the general population and matched for age, gender, and region of residence. Administrative data from centralized health care databases were compiled to provide a complete picture of health care use, including hospitalizations, physician contacts, long-term care admissions, home care services, and the occurrence of secondary complications.
Results: In all, 233 individuals with SCI and 1165 matched controls were followed for 6 years. Compared with the control group, persons with SCI were rehospitalized 2.6 times more often, spent 3.3 more days in hospital, were 2.7 times more likely to have a physician contact, and required 30 times more hours of home care services. Of those with SCI, 47.6% were treated for a urinary tract infection, 33.8% for pneumonia, 27.5% for depression, and 19.7% for decubitus ulcer.
Conclusion: SCI places a heavy burden on the health care system. Persons with SCI have greater rates of contact with the health system compared with the general population. Secondary complications continue to affect persons with SCI long after the acute trauma.
Similar content being viewed by others
Introduction
In the months and years following acute trauma, persons with spinal cord injury (SCI) are at risk for a number of secondary health conditions, which can result in frequent contact with physicians and other health providers and hospitalization.1 In a cross-sectional study of Model SCI System patients, researchers found that 95.6% of patients had at least one medical complication at the time of their routine annual check-up.2 Between 28 and 35% of patients (depending on level of injury) had a urinary tract infection and 22.4% had decubitus ulcers. In a population-based survey of persons with SCI in Quebec, Canada, researchers found that 56% had experienced a urinary tract infection in the previous year, and 28% reported a decubitus ulcer.3 Respiratory, cardiovascular, and psychosocial issues have also been shown to be prevalent in studies of postacute SCI patients.3, 4, 5, 6, 7 Persons with SCI are two times more likely to be rehospitalized than the general population of the United States.4 The proportion of people with SCI who are rehospitalized in a given year has been reported between 27 and 57%.1, 4, 8, 9, 10, 11 The highest rates of readmission to hospital occur in the first 5 years following injury.10, 11 In a study of hospitalizations in the first year postinjury, Davidoff et al8 found the leading reasons for admission were urinary tract infections (17.0%) and deep venous thrombosis (12.8%). Beyond the first postinjury year, Meyers et al9 found that respiratory complications (19%), urinary tract infections (14%), and dermatological conditions (7%) were the primary reasons for hospital admissions.
Ongoing complications and hospital admissions are costly.1, 12, 13, 14 They disrupt work, education, and interpersonal relationships, and may negatively impact quality of life.15 In order to assist health care providers develop effective programs for persons with SCI, it is important to have a clear understanding of the nature and extent of health service utilization. While previous research has provided some information in this regard, many studies suffer from methodological limitations. Most studies are cross-sectional and report on the experiences of individuals who have been injured for varied lengths of time and are therefore at different states of risk.1, 3, 6, 10 Some studies are restricted to a single health care center or service provider, which may limit their generalizability.10, 11 Others have relied on interviews and patient surveys, which may be affected by recall bias.1, 3, 4
The present study addresses some of these limitations using a population-based cohort design to follow persons who sustained a traumatic SCI in Alberta, Canada. Administrative data from centralized databases were compiled to provide a complete picture of health care use following SCI, including hospital admissions, physician contacts, long-term care, and home care services. The primary objectives of this study were: (1) To describe health care utilization by persons with SCI from date of injury to 6-years postinjury; (2) To describe the incidence and pattern of secondary medical complications following injury; and (3) To compare the utilization of health services by persons with SCI with that of the general population.
Methods
Study location
Alberta is located in western Canada and occupies an area of approximately 661 000 square kilometers. In 1993, the population was estimated as 2.7 million, of which 75% lived in urban areas. Alberta has a universal publicly funded health care system that guarantees access to medically necessary hospital and medical services for all residents of the province. Virtually all (>99%) Alberta residents are registered with the system.16
Definition of SCI
SCI was defined as the occurrence of an acute traumatic lesion of neural elements in the spinal canal (spinal cord and cauda equina) resulting in resolving or permanent neurological deficit. Cases were identified by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes for SCI: 806.x (fracture of the vertebral column with SCI) or 952.x (SCI without evidence of spinal bone injury). The use of these two ICD-9-CM codes was based on the ‘Uniform Data Systems Case Definition’ recommended by the US Centers for Disease Control and Prevention.17 This definition has been used extensively in trauma registries and surveillance systems to identify SCI.18, 19, 20
Data sources
Data for this study were gathered from the Alberta Ministry of Health and Wellness, which maintains computerized records of all hospital and medical services in Alberta.16 The reliability and utility of administrative health care data have been established.21, 22, 23 Records from five databases were used to compile information on individual encounters with the Alberta health care system during the 6-year follow-up period. Records were linked deterministically using the unique personal health number that is assigned to every Albertan. The data sources were:
Alberta Health Care Insurance Stakeholder Registry (Stakeholder Registry): This database contains demographic information about Albertans registered with the health care system.
Canadian Institute for Health Information (CIHI) Hospital Inpatient database (Inpatient database): Records of all hospitalizations in Alberta are collected in the Inpatient database. Separation abstracts are completed for each admission by trained medical records nosologists and contain admission and discharge dates, up to 16 ICD-9-CM diagnostic codes, and up to 10 ICD-9-CM procedure codes.
Alberta Health Insurance Plan Payment Data (Physician claims database): This is a database of fee-for-service claims submitted by physicians and other health service providers (eg, optometrists and chiropractors) in Alberta for the provision of medically required services. For the purposes of this research, only physician claims are reported and include medical, surgical, obstetric, anesthesia, and diagnostic services. For claims made in 1992 and 1993, one 3-digit ICD-9-CM diagnostic code was assigned to each contact. Since 1994, up to three 4-digit ICD-9-CM codes were assigned for each encounter.
Long-Term Care Resident Classification (Long-term care): Data are collected for all residents in long-term care institutions during the annual assessment period. Individuals are included if they were classified during the previous year or are resident at the time of assessment. Admission to a long-term care facility and nursing care intensity were used as measures of long-term care.
Home Care Information System (Home care): The database provides information on clients receiving services provided under the home care program including nursing care, meal services, and other support for activities of daily living. Total hours of service and service duration were used as measures of home care utilization.
Inclusion criteria and case identification
A search of the inpatient database identified Albertans who were hospitalized for SCI during the study period. The date of the index hospitalization was considered the date of the SCI. The inclusion criteria for the study were: (1) admission to a hospital in Alberta, between April 1, 1992 and March 31, 1994, with an ICD-9-CM code for SCI, (2) transfer to an acute care center in Edmonton or Calgary, the two major cities in the province, (3) an external cause of injury code (E code) consistent with traumatic SCI, and (4) Alberta residency at the time of injury. In Alberta, all severely injured patients are routinely transferred from smaller, rural hospitals to an acute care center. Therefore, we assumed that all patients with a suspected SCI would be transferred to Edmonton or Calgary for confirmation of diagnosis and treatment. Patients were excluded if they had a subsequent diagnosis of a ‘conversion’ disorder (ICD-9-CM code 300.11) or if there was a record of a hospital or physician claim for SCI within 30 days prior to the index visit.
Control group
For comparison with the general population, each SCI case was matched to five controls randomly selected from the Stakeholder Registry. Controls were matched with SCI cases for age, gender, and region of residence (to control for distance and access to health services). Individuals were not eligible to be controls if they sustained an SCI at any time during the follow-up period or if there was evidence of a prior SCI (ICD-9-CM codes 952.x, 806.x, or 907.2 [late effect of SCI]).
Follow-up period
Data on health care utilization were collected from date of injury for each SCI case to 6 years postinjury. For each individual in the control group, data were collected from the date of injury of their respective cases to 6 years after the date of injury. Deaths and losses to follow-up were confirmed in the Stakeholder Registry. Persons who were lost to follow-up were presumed to have moved from the province.
The initial hospitalization period refers to the episode of care in the hospital system from date of SCI to the first definitive discharge to the community or to a long-term care facility. It includes admissions to rural hospitals prior to transfer to an acute care hospital in Edmonton or Calgary, acute care hospitalization, and inpatient rehabilitation. For patients who received acute and rehabilitation care in the same hospital (∼40%), it was not possible to separate the acute care and inpatient rehabilitation phases.
For subsequent hospital admissions (after initial hospitalization for SCI cases), the reason for admission was determined by the principal diagnosis for each hospitalization. For physician visits, the reason for the contact was determined by the first diagnostic code for each physician claim. Reasons for admissions or contacts were grouped into diagnostic categories following the ICD-9-CM (Appendix A).
A number of secondary complications were selected for examination: urinary tract infection, decubitus ulcer, pneumonia, septicemia, venous thromboembolism, and pulmonary embolism. The presence of a complication was determined by an ICD-9-CM code for the condition in any diagnostic field in the Inpatient database and the Physician claims database (Appendix B). This study also examined depression following SCI. The working definition of depression was an ICD-9-CM code for depressive disorders (311), affective disorders (296.x), adjustment reaction (309.x), or neurotic depression (300.4). A person was determined to have depression if there was at least one diagnosis in the inpatient database or if there were two or more physician contacts for depression over the follow-up period.22, 24
Ethics
This study was approved by the Health Research Ethics Board (Panel B: Health Research) at the University of Alberta, Edmonton, Canada. To maintain the confidentiality of patients, all personal identifiers were removed prior to the release of data from the Alberta Ministry of Health and Wellness.
Analyses
Descriptive statistics for demographic and injury characteristics are presented using frequencies and percentages for categorical data, and medians and interquartile ranges (IQR) for continuous variables. Annual age–gender-specific rates of injury and 95% confidence intervals (95% CI) were constructed using the registrant count at June 30, 1993 from the Stakeholder Registry as population denominators. Place of residence (rural or urban) was determined using the postal code reported for each individual in the Stakeholder Registry. Rural residents were identified by the presence of a zero in the second position of their postal code.25 Differences between groups were tested using the Mann–Whitney U test and χ2, where appropriate (alpha was set at 0.05).
Rates for hospital admissions and physician contacts are reported as admissions or contacts per person year or 100-person years. Poisson regression with generalized estimating equations was used to compare number of hospitalizations and physician contacts between the SCI group and the control group.26, 27 Results are presented as rate ratios (RR) with 95% CI.
Results
Case ascertainment
From the inpatient database, a total of 233 patients met the inclusion criteria for traumatic SCI and were included in the follow-up study. A total of 1165 matched controls were selected from the general population. The mean incidence rate was 43.5 per million population per year (95% CI: 37.9, 49.1). The mean annual incident rate for males was 65.9 per million population (95% CI: 56.1, 75.6) and for females was 21.3 per million (95% CI: 15.7, 26.8). For rural residents, the incidence rate was 70.7 per million per year compared with 31.4 per million per year for those living in urban areas.
Demographics and injury characteristics
Of the 233 individuals who sustained an SCI, 176 (75.5%) were male (Table 1). The median age for the total sample was 34.0 years (IQR 24.0–48.0). Ages ranged from 9 to 95 years. The median age differed between males (32.0 years; IQR 22.5–46.5) and females (41.0 years; IQR 29.0–69.0) (U=3585.5, P=0.001). Due to matching, the age and gender distribution of the control group was the same as the SCI group.
Motor vehicle collisions accounted for the greatest number of SCI (Table 1). A total of 116 (49.8%) individuals were involved in a collision with a motorized vehicle, including drivers, passengers, pedestrians, and bicyclists. Falls were the second most common cause of injury with 61 (26.2%) people affected.
In total, 117 (50.2%) individuals sustained an injury at the cervical level, while 98 (42.1%) sustained an injury at the thoracic, lumbar, sacral, or cauda equina level (Table 1). Overall, 43 (18.5%) of the injuries were classified as complete and 69 (30.0%) were incomplete. For 121 (51.9%) cases the extent of SCI was not specified (Table 1).
In all, 142 (60.9%) individuals sustained another injury in addition to their SCI (Table 1). Overall, 51 (21.9%) people were diagnosed with a traumatic brain injury in addition to their SCI.
Deaths and losses to follow-up
Totally, 20 (8.6%). SCI patients died during their initial hospitalization (Table 1). The median time to death was 10.0 days (IQR 5.0–19.0) ranging from 2 to 134 days. During the 6-year follow-up period, a greater proportion of persons in the SCI group (16 {7.5%}) died than in the control group (45 {3.9%}) (χ2=47.8, P<0.001). For both groups, the individuals who died were significantly older than those who were alive at the end of the follow-up period.
In addition to those who died during the follow-up period, 119 people were lost to follow-up. Among individuals with SCI, 20 (10.2%) were lost to follow-up compared with 99 (8.8%) people from the control group (χ2=0.35, P=0.55). There were no statistically significant differences in age and gender between those lost to follow-up and those followed to the end of the study period in either the SCI or control group.
Discharge status
Following initial hospitalization, most individuals were discharged into the community; however, 10 (4.7%) people were discharged to a long-term care facility. The median age for this group was 69.0 years (IQR 38.0–78.0). During the follow-up period an additional eight people were admitted to a long-term care facility. From the control group, 20 (1.7%) people were admitted to a long-term care facility. The SCI group required a greater level of nursing care in long-term care with 73.3% receiving care at the two highest levels compared with 40.3% from the control group (χ2=8.8, P=0.003).
Initial hospitalization
During initial hospitalization, including acute care and inpatient rehabilitation, the SCI group was hospitalized for a total of 14 200 days (Table 2). The median length of stay (LOS) was 26.0 days (IQR 6.0–98.0) and ranged from 1 to 450 days. For patients with a complete SCI, the median LOS was 139.5 days (IQR 87.5–171.0); for those with incomplete injuries, it was 50.5 days (IQR 15.5–93.0). Where extent of SCI was unspecified, the median LOS was 10.0 days (IQR 4.0–30.0). For 78 patients, it was possible to identify the acute care and inpatient rehabilitation phases of care. For the acute care phase, the median LOS was 24.0 days (IQR 16.0–43.0), while for inpatient rehabilitation it was 72.0 days (IQR 46.0–106.0).
Rehospitalizations
For patients who were discharged alive following initial hospitalization, 122 (57.3%) were rehospitalized at least once during the follow-up period for a total of 365 admissions (Table 2). Over the 6-year follow-up, the median LOS was 4.0 days (IQR 2.0–9.0) per hospitalization and ranged from 1 to 277 days. The number of hospital admissions per person ranged from 1 to 27. In all, 57 (46.7%) people were hospitalized once, 21 (17.2%) were hospitalized twice, 39 (32.0%) were admitted between three and nine times, and five (4.1%) were rehospitalized on 10 or more occasions.
Following initial discharge, individuals with SCI had 2.6 (95% CI: 2.3, 3.0) more hospital visits than the control group (Figure 1). The SCI group was hospitalized for 3.03 days per person year compared with 0.92 days per person year for the control group. The median LOS for the control group was the same as the SCI group (4.0 days; IQR 2.0–8.0).
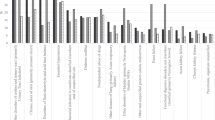
Figure 2 illustrates the distribution of hospital admissions by diagnostic category. For both the SCI and control groups, respiratory diseases, digestive system diseases, and injuries were the most common principal diagnoses associated with hospital admissions. However, for every diagnostic category, the SCI group had more admissions and a greater proportion of people admitted compared with the control group.
Hospitalizations by diagnostic category for SCI patients and their matched controls over 6 years of follow-up (excludes initial hospitalization for the SCI group). Diagnostic category is based on the principal diagnosis for each admission. ‘Other’ includes neoplasms, blood disorders, pregnancy, perinatal, and congenital conditions
Physician contacts
Over the 6-year follow-up period, the SCI group had 17 227 contacts with physicians, including outpatient visits and during hospitalization (Table 3). In the year of injury, the median number of contacts was 22.0 (IQR 12.0–37.0). In the subsequent 5 years, the median number of contacts declined from 8.0 (IQR 2.5–15.5) in the second postinjury year to 4.0 (IQR 0.0–10.0) in the sixth year (χ2=5.0, P=0.03). For the control group, the median number of contacts per year was 3.0 (IQR 1.0–6.0). In every year postinjury, there were more physician contacts by the SCI group than the control group (RR=2.7, 95% CI: 2.6, 2.71).
In the first postinjury year, the SCI group visited family physicians, physical medicine specialists, and internists most frequently (Figure 3). In the subsequent 5 years, family physicians, internists, and psychiatrists were seen most often. Over the 6-year follow-up, the control group also visited family physicians, internists, and psychiatrists most often. The number of visits to specialists and the proportion of people seeing specialists were higher among persons with SCI.
Figure 4 shows number of physician contacts by diagnostic category. For the SCI group, visits to physicians in the first postinjury year appear to be related to the initial injury episode and associated neurological symptoms. In the subsequent 5 years, the main reasons for visits were ill-defined symptoms, injuries, disorders of the genitourinary system, and mental disorders. For the control group, the main reasons for physician visits were ill-defined symptoms, disorders of the respiratory system, musculoskeletal diseases, and mental disorders. For all diagnostic categories the SCI group were more seen more often than the control group.
Secondary complications
During initial hospitalization, 106 (45.5%) patients were treated for a urinary tract infection, decubitus ulcer, pneumonia, or septicemia (Table 4). Of these, 32 (13.7%) individuals were treated for more than one of these complications. Most (93.2%) patients with complete injuries were treated for at least one complication, compared with 47.1% of those with incomplete injuries and 29.8% of those where the extent of SCI was not specified. After discharge from initial hospitalization, 94 (44.1%) people were treated for a urinary tract infection, decubitus ulcer, pneumonia or septicemia either during a subsequent hospitalization or by a physician (Table 4). Of these, 31 (33.3%) had more than one complication.
Over the 6-year follow-up, 111 (47.6%) people with SCI were treated for a urinary tract infection, either during initial hospitalization, a subsequent hospitalization, or by a physician (Figure 5). In all, 79 (33.8%) people were treated for pneumonia, 46 (19.7%) for decubitus ulcer, and 36 (15.5%) for septicemia. For each complication, a higher proportion of individuals from the SCI group were treated for one of these conditions compared with the control group (Figure 5).
Eight (3.4%) people with SCI were treated for venous thromboembolism following their injury (Figure 5). Three people were treated during initial hospitalization and four were treated within the first year of injury. One individual was treated in the fifth year postinjury. Eleven (4.7%) people were treated for pulmonary embolism (Figure 5). Nine were treated during initial hospitalization and two were treated within the first year postinjury. Within the control group, three individuals (0.3%) were treated for venous thromboembolism and three (0.3%) for pulmonary embolism over the 6-year follow-up.
Over the entire follow-up period, 64 (27.5%) individuals with SCI were treated for depression (Figure 5). Totally, 26 people were treated during initial hospitalization and an additional 38 were treated either during a subsequent hospitalization or as an outpatient. Among the control group, 10.8% were treated for depression. Persons with SCI were more likely to be treated by a psychiatrist and more likely to be rehospitalized for a mental disorder than the control group (Figures 2 and 3).
Home care
Following discharge from initial hospitalization, 66 (31.0%) individuals with SCI received a total of 76 588 h of home care services, or 65.0 h per person year. This compares with 73 (6.3%) persons from the control group who received 2.2 h per person year.
Discussion
This study examined the utilization of health services following traumatic SCI over a 6-year period in a Canadian province with universal health care and centralized health care databases. Utilization of health services was compared with that of a control group randomly selected from the general population of the province and matched on age, gender, and region of residence. Information on utilization was comprehensive and included an examination of all hospitalizations, long-term care admissions, fee-for-service physician contacts, and home care services in the province.
Overall, 233 individuals with traumatic SCI were followed from their date of injury to 6 years postinjury. Many spent prolonged periods in hospital and often required readmission. Following initial hospitalization, persons with SCI were hospitalized 2.6 more times than their matched controls. They also had 2.7 more contacts with physicians and required 30 times more hours of home care services. After the first year postinjury, the pattern of health care use in terms of diagnoses was similar to that of the control group. For both groups, the primary reasons for hospitalization related to respiratory and digestive disorders, and family physicians and internists were the physicians most frequently contacted. However, the rates of utilization for each diagnostic category and physician specialty were higher for persons with SCI compared with their matched controls.
These results support previous generic research, which shows that persons with disabilities or chronic diseases use health services more than the general population;28, 29 however, limited research has specifically examined persons with SCI. In a Swedish study, Levi et al30 compared the health profile of persons with chronic SCI with that of the general population. Data for their study were derived from the annual ‘Level-of-Living’ survey conducted by the Swedish Bureau of Statistics. They found that persons with SCI experienced significantly more health problems than the general population and reported a higher prevalence of medical symptoms, greater use of medications, more emergency department visits, and more hospital admissions. They also found a higher prevalence of dysfunctions related to SCI, such as bladder dysfunction and skin problems. However, the prevalence of non-SCI-related conditions, such as diabetes, high blood pressure, and cardiac disease, was the same or less than the general population. This finding differs from the present study, which showed that for secondary complications and for all broad diagnostic categories, the SCI group had more physician contacts and more hospitalizations than the control group. An examination of the top 10 specific diagnoses for both groups revealed that physician contacts for hypertension were the same, however, the SCI group had 1.7 times the number of physician contacts for diabetes (data not shown). Differences in findings may relate to the diverse study population from Sweden whose duration of injury ranged from 1 to 44 years.
Few studies have reported on the utilization of physician services by persons with SCI. In the present study, the SCI group had a median of 52.0 physician contacts over the 6-year follow-up period. Almost all persons (99.1%) saw a family physician at least once during the follow-up period. After family physicians, internists (36.5%), physical medicine specialists (36.0%), and urologists (31.2%) were the physicians seen most often after the first year postinjury. Approximately 12% visited a psychiatrist over the 6-year follow-up. These results confirm those reported by Berkowitz et al.1 In a survey of 758 persons who were at least 3 years postinjury, they found that 86.3% saw a physician at least once a year, with a mean of 18 visits per year. In the year prior to the survey, the most commonly visited physicians were urologists (45%), family physicians (44%), neurologists/neurosurgeons (31%), orthopedic surgeons (30%), and physical medicine specialists (27%). Approximately 10% of those surveyed had visited a psychiatrist in the previous year. Our findings also support those of Meyers et al,9 who conducted a survey of 96 people with high-level SCI who were between 1 and 41 years postinjury. They found that 78% had seen a physician in the previous year. The median number of outpatient visits to a physician or nurse practitioner in the previous year was 4.0. Almost 50% reported one to five contacts, 39% reported six or more, and 8% reported seeing a physician or nurse practitioner at least once per week.
In the current study, the proportion of persons with SCI who were rehospitalized following initial discharge were 22.5, 29.4, 14.9, 16.0, 13.8, and 13.4% in years 1 through 6, respectively. These findings confirm to those reported by Johnson et al4 in a population-based study using self-report survey methodology. They interviewed SCI survivors from Colorado at their first, third, and fifth year postinjury anniversaries and found that 27.0% of their cohort was rehospitalized in the first postinjury year, 20.1% in year 3 and 18.8% in year 5. In a cross-sectional study of Model SCI System, patients who were between 1 and 7 years postinjury, researchers found that 26% of patients had been hospitalized at least once in the previous year.10
Other studies, however, have reported higher rates of rehospitalization. Davidoff et al8 followed patients from a Model SCI System center for 1 year following discharge from initial rehabilitation and found that 39% were readmitted at least once during the year. In a study of male veterans with SCI, Samsa et al11 reported that between 42 and 50% (depending on level and extent of injury) were readmitted to a Veterans Affairs hospital in the US in the first year postinjury. This rate declined to between 30 and 47% in the fifth postinjury year. These higher rates may reflect a more severely injured patient population who continue to use the Model SCI or Veterans Affairs systems for follow-up care.
As has been shown in previous research, persons with SCI are at risk for secondary complications, not only during initial hospitalization but also in the years following discharge.2, 3, 4, 6, 31 Persons with SCI are treated for these conditions at significantly higher rates than their matched controls. While not all persons with SCI will require treatment for a secondary complication, it is a significant minority who will require follow-up care through the health system.
The current research showed that the SCI group received a diagnosis for depression 2.5 times more than the control group. While a confirmation of diagnosis was not possible from this methodology, we are confident with these estimates given that the rate among the control group was 10.8%, which is almost identical (10.2%) to the estimated prevalence of affective disorders in the general population in Alberta.32 Previous research is equivocal as to the occurrence of depression following SCI. Among patients who were assessed during their initial rehabilitation, between 13.7 and 43.8% were reported to have depression.33, 34, 35, 36 In a study that followed patients for 2 years after injury, researchers reported that 26.8% were clinically depressed.37 Among individuals who were between 1 and 44 years postinjury, Levi et al reported that persons with SCI more likely than the general population to report mental symptoms such as anxiety (OR=3.7), sleep disturbance (OR=3.5), and fatigue (OR=2.1). The present study found that 11.2% of patients were treated for depression during initial hospitalization, and an additional 38 (17.8%) were treated following discharge, for an overall rate of 22.1%. For all measures of mental disorders in this study, the SCI group used more services than the control group, suggesting a greater need for mental health care.
It is clear from this research that the need for health services by people with SCI continues long after they complete their initial hospitalization. These services are particularly important to prevent secondary complications. This requires ongoing multifaceted efforts at maintaining contact with persons with SCI after their discharge into the community. Family physicians may be ideally suited to facilitate this ongoing contact. Our study showed that family physicians were visited most often after the first postinjury year and most individuals in our cohort contacted a family physician at least once following their injury. However, family physicians may not be familiar with the lifelong medical needs that are specific to a person with SCI.38 Thus, information packages tailored to family physicians who have patients with SCI is an important service that could be developed by SCI specialists.
Multidisciplinary outreach services also have a role to play in the provision of information and support for many aspects of medical and social care for persons with SCI.39, 40 Because individuals tend to negate the possibility that ‘silent’ complications may be developing, they may be unwilling to take the time and expense to come back for regular evaluations.41 A follow-up system involving reminder cards or phone calls from family physicians, outreach services, and/or peer support groups might encourage persons with SCI to have annual physical examinations. The use of technology can help to increase access to a range of health professionals and services to SCI population and support the delivery of outreach services.42, 43, 44 For example, researchers from an SCI center in Georgia have demonstrated that telehealth interventions can be used successfully to manage skin care and to promote general self-care among people with SCI.42, 43 Further research into what strategies may be best suited for this important group of patients is clearly needed.
Potential limitations of this research need to be discussed. First, data are not available on health care services that were provided outside the province of Alberta. It is not possible to determine the extent to which patients sought out-of-province care or the nature of services. This would result in an underestimate of service utilization for both the SCI and control groups. Second, the data sources do not provide information on neurological outcomes or functional recovery of persons with SCI, nor do they include measures of socioeconomic status, which might be associated with health status. This precluded an analysis of risk factors associated with utilization of health services. Notwithstanding the above concerns, to our knowledge this study represents the most comprehensive and extended picture of health care utilization by individuals with SCI. It is population-based, followed individuals from date of injury to 6 years postinjury, and includes data on all hospitalizations, fee-for-service physician contacts, home care services, and long-term care admissions in a large geographically defined region. The results of this study can be generalized to areas with similar populations.
Conclusion
SCI places a heavy burden on the health care system in the first 6 years following injury. Persons with SCI have higher rates of contact with the health care system compared with the general population, including hospitalizations, long-term care admissions, home care services, and physician contacts. Secondary complications, including urinary tract infections, decubitus ulcer, pneumonia and septicemia, continue to plague persons with SCI long after the acute trauma. In addition, other health care problems appear to be more common in this population. For example, psychological disorders are greater than those of the general population. Persons with SCI continue to be high users of the health care system long after the acute care phase. Ongoing follow-up care that addresses all aspects of physical and psychological well being, not just those directly related to the injury, is essential for individuals with SCI.
References
Berkowitz M, Harvey C, Greene CG, Wilson SE . The Economic Consequences of Traumatic Spinal Cord Injury. Demos Publications: New York (NY) 1992, pp 1–202.
Anson CA, Shepherd C . Incidence of secondary complications in spinal cord injury. Int J Rehabil Res 1996; 19: 55–66.
Noreau L, Proulx P, Gagnon L, Drolet M, Laramee M-T . Secondary impairments after spinal cord injury: a population-based study. Am J Phys Med Rehabil 2000; 79: 526–535.
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG . Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998; 36: 45–50.
Jackson AB, Groomes TE . Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil 1994; 75: 270–275.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ . Long-term medical complications after traumatic spinal cord injury: a regional model system analysis. Arch Phys Med Rehabil 1999; 80: 1402–1410.
Ragnarsson KT, Hall KM, Wilmot CB, Carter RE . Management of pulmonary, cardiovascular, and metabolic conditions after spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GG (eds) Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen Publishers: Gaithersburg (MD) 1995, pp 79–99.
Davidoff G et al. Rehospitalization after initial rehabilitation for acute spinal cord injury: incidence and risk factors. Arch Phys Med Rehabil 1990; 71: 121–124.
Meyers AR, Feltin M, Master RJ, Nicastro D, Cupples LA . Rehospitalization and spinal cord injury: cross-sectional survey of adults living independently. Arch Phys Med Rehabil 1985; 66: 704–708.
Ivie CS, DeVivo MJ . Predicting unplanned hospitalizations in persons with spinal cord injury. Arch Phys Med Rehabil 1994; 75: 1182–1188.
Samsa GP, Landsman PB, Hamilton B . Inpatient hospital utilization among verterans with traumatic spinal cord injury. Arch Phys Med Rehabil 1996; 77: 1037–1043.
Menter RR et al. Impairment, disability, handicap and medical expenses of persons aging with spinal cord injury. Paraplegia 1991; 29: 613–619.
Johnson RL, Brooks CA, Whiteneck GG . Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord 1996; 34: 470–480.
DeVivo MJ, Whiteneck GG, Charles ED . The economic impact of spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GG (eds) Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen Publishers: Gaithersburg (MD) 1995, pp 234–271.
Krause JS . Intercorrelations between secondary conditions and life adjustment in people with spinal cord injury. SCI Psychosoc Process 1998; 11: 3–7.
Alberta Health and Wellness. Accessing Data for Research Purposes: A Researcher's Handbook. Alberta Health and Wellness: Edmonton (AB) 1999, pp 1–28.
Thurman DJ, Sniezek JE, Johnson D, Greenspan A, Smith SM . Guidelines for Surveillance of Central Nervous System Injury. Centers for Disease Control and Prevention: Atlanta 1995, pp 1–106.
Thurman DJ, Burnett CL, Jeppson L, Beaudoin DE, Sniezek JE . Surveillance of spinal cord injuries in Utah, USA. Paraplegia 1994; 32: 665–669.
Surkin J, Colley Gilbert BJ, Harkey HL, Sniezek JE, Currier M . Spinal cord injury in Mississippi: findings and evaluation, 1992–1994. Spine 2000; 25: 716–721.
O’Connor P . Incidence and patterns of spinal cord injury in Australia. Accid Anal Prev 2002; 34: 405–415.
Roos LL, Walld R, Wajda A, Bond R, Hartford K . Record linkage strategies, outpatient procedurs, and administrative data. Med Care 1996; 34: 570–582.
Rawson NSB, Malcolm E, D'Arcy C . Reliability of the recording of schizophrenia and depressive disorder in the Sakatchewan health care datafiles. Soc Psychiatry Psychiatr Epidemiol 1997; 32: 191–199.
Coleman E, Wagner EH, Grothaus LC, Hecht J, Savarino J, Buchner DM . Predicting hospitalization and functional decline in older health plan enrollees: are administrative data as accurate as self-report? J Am Geriat Soc 1998; 46: 419–425.
West SL, Richter A, Melfi CA, McNutt M, Nennstiel ME, Mauskopf JA . Assessing the Saskatchewan database for outcomes research studies of depression and its treatment. J Clin Epidemiol 2000; 53: 823–831.
Statistics Canada. 1996 Census Dictionary, Final edition (Cat. No. 92-351-UIE) Statistics Canada: Ottawa (ON) 1999, pp 220–221.
Liang KY, Zeger S . Longitudinal data analysis using generalized linear models. Biometrika 1986; 73: 12–22.
Zeger S, Liang KY . The analysis of discrete and continuous longitudinal data. Biometrics 1986; 42: 121–130.
Tomiak M, Berthelot J-M, Mustard CA . A profile of health care utilization of the disabled population in Manitoba. Med Care 1998; 36: 1383–1397.
Rice DP, LaPlante MP . Medical expenditures for disability and disabling comorbidity. Am J Public Health 1992; 82: 739–741.
Levi R, Hultling C, Seiger A . The Stockholm spinal cord injury study: 3. Health-related issues of the Swedish annual level-of-living survey in SCI subjects and controls. Paraplegia 1995; 33: 726–730.
Chen D, Apple DF, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury: current experience of the Model Systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Bland RC, Newman SC . Lifetime prevalence of psychiatric disorders in Edmonton. Am J Psychiatry 1988; 77: 24–32.
Howell T, Fullerton DT, Harvey RF, Klein M . Depression in spinal cord injured patients. Paraplegia 1981; 19: 284–288.
Frank RG, Kashani JH, Wonderlich SA, Lising A, Visot LR . Depression and adrenal function in spinal cord injury. Am J Psychiatry 1985; 142: 252–253.
Judd FK, Stone J, Webber JE, Brown DJ, Burrows GD . Depression following spinal cord injury: a prospective in-patient study. Br J Psychiatry 1989; 154: 668–671.
Elliott TR, Frank RG . Depression following spinal cord injury. Arch Phys Med Rehabil 1996; 77: 816–823.
Craig AR, Hancock KM, Dickson HG . A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Paraplegia 1994; 32: 675–679.
Tepperman PS . Primary care after spinal cord injury. Postgrad Med 1989; 86: 211–218.
Cox RJ, Amsters DI, Pershouse KJ . The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin Rehabil 2001; 15: 600–606.
Raghavan P, Raza W, Ahmed Y, Chamberlain M . Outreach services in spinal injury rehabilitation [letter]. Clin Rehabil 2002; 16: 910–911.
Canupp KC, Waites KB, DeVivo MJ, Richards JS . Predicting compliance with annual follow-up evaluations in persons with spinal cord injury. Spinal Cord 1997; 35: 314–319.
Phillips V, Temkin A, Vesmarovich S, Burns R, Idleman L . Using telehealth interventions to prevent pressure ulcers in newly injured spinal cord injury patients post-discharge. Int J Technol Assessment Health Care 1999; 15: 749–766.
Phillips V, Vesmarovich S, Hauber R, Wiggers E, Egner A . Telehealth: reaching out to newly injured spinal cord patients. Public Health Rep 2001; 116(Suppl 1): 94–102.
Edwards L, Krassioukov A, Fehlings MG . Importance of access to research information among individuals with spinal cord injury: results of an evidence-based questionnaire. Spinal Cord 2002; 40: 529–535.
Acknowledgements
This research was supported by a grant from the Institute of Health Economics, Edmonton, Alberta, Canada. The Alberta Paraplegic Foundation and the Alberta Heritage Foundation for Medical Research provided support to Dr Dryden. The Canadian Institute of Health Research supports Dr Rowe's research through the Canadian Research Chairs program. Dr Voaklander is supported via a grant from the British Columbia Ministry of Health. The authors thank the Alberta Centre for Injury Control and Research for their assistance.
Author information
Authors and Affiliations
Additional information
Sources of support: This work was funded by a grant from the Institute of Health Economics, Edmonton, AB, Canada
Rights and permissions
About this article
Cite this article
Dryden, D., Saunders, L., Rowe, B. et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 42, 513–525 (2004). https://doi.org/10.1038/sj.sc.3101629
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101629
Keywords
This article is cited by
-
Use of professional home care in persons with spinal cord injury in Switzerland: a cross-sectional study
BMC Health Services Research (2023)
-
The effect of rurality and distance from care on health outcomes, environmental barriers, and healthcare utilization patterns in persons with traumatic spinal cord injury
Spinal Cord (2023)
-
Multimorbidity in persons with non-traumatic spinal cord injury and its impact on healthcare utilization and health outcomes
Spinal Cord (2023)
-
Relationship between secondary health conditions and life satisfaction in persons with spinal cord injury: study across twenty-one countries
Quality of Life Research (2023)
-
Development of a comprehensive assessment tool to measure the quality of care for individuals with traumatic spinal cord injuries
Spinal Cord Series and Cases (2023)