Key Points
-
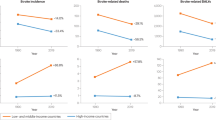
Although global stroke incidence and mortality declined from 1990 to 2013, the stroke burden, in terms of absolute numbers of people affected by stroke, continues to increase rapidly throughout the world
-
The ever-increasing burden of stroke suggests that current primary prevention strategies for stroke and cardiovascular disease (CVD) are not sufficiently effective
-
To improve primary stroke prevention strategies, we need to shift the emphasis from a high-risk approach to a more comprehensive approach targeting people at all levels of CVD risk
-
To be cost-effective, primary stroke prevention strategies must be integrated with prevention strategies for other major noncommunicable diseases that share common risk factors with stroke, including CVD, vascular dementia and diabetes
-
Resources for the development and implementation of culturally appropriate and population-specific primary stroke prevention strategies could be taken from revenue resulting from taxation on tobacco, salt, sugar and alcohol
-
Given the already immense and fast-increasing burden of stroke and other major NCDs, which threatens global sustainability, failure to act on primary prevention of these diseases is unacceptable
Abstract
The increasing global stroke burden strongly suggests that currently implemented primary stroke prevention strategies are not sufficiently effective, and new primary prevention strategies with larger effect sizes are needed. Here, we review the latest stroke epidemiology literature, with an emphasis on the recently published Global Burden of Disease 2013 Study estimates; highlight the problems with current primary stroke and cardiovascular disease (CVD) prevention strategies; and outline new developments in primary stroke and CVD prevention. We also suggest key priorities for the future, including comprehensive prevention strategies that target people at all levels of CVD risk; implementation of an integrated approach to promote healthy behaviours and reduce health disparities; capitalizing on information technology to advance prevention approaches and techniques; and incorporation of culturally appropriate education about healthy lifestyles into standard education curricula early in life. Given the already immense and fast-increasing burden of stroke and other major noncommunicable diseases (NCDs), which threatens worldwide sustainability, governments of all countries should develop and implement an emergency action plan addressing the primary prevention of NCDs, possibly including taxation strategies to tackle unhealthy behaviours that increase the risk of stroke and other NCDs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Feigin, V. L. et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 383, 245–254 (2014).
Roth, G. A. et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N. Engl. J. Med. 372, 1333–1341 (2015).
Feigin, V. L. et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the GBD 2013 study. Neuroepidemiology 45, 161–176 (2015).
Murray, C. J. & Lopez, A. D. Measuring the global burden of disease. N. Engl. J. Med. 369, 448–457 (2013).
Mensah, G. A., Norrving, B. & Feigin, V. L. The global burden of stroke. Neuroepidemiology 45, 143–145 (2015).
Roth, G. A. et al. Methods for estimating the global burden of cerebrovascular diseases. Neuroepidemiology 45, 146–151 (2015).
Truelsen, T. et al. Causes of death data in the Global Burden of Disease estimates for ischemic and hemorrhagic stroke. Neuroepidemiology 45, 152–160 (2015).
Krishnamurthi, R. V. et al. Stroke prevalence, mortality and disability-adjusted life years in children and youth aged 0–19 years: data from the Global and Regional Burden of Stroke 2013. Neuroepidemiology 45, 177–189 (2015).
Krishnamurthi, R. V. et al. Stroke prevalence, mortality and disability-adjusted life years in adults aged 20–64 years in 1990–2013: data from the Global Burden of Disease 2013 study. Neuroepidemiology 45, 190–202 (2015).
Barker-Collo, S. et al. Sex differences in stroke incidence, prevalence, mortality and disability-adjusted life years: results from the Global Burden of Disease Study 2013. Neuroepidemiology 45, 203–214 (2015).
Feigin, V. L., Mensah, G. A., Norrving, B., Murray, C. J. & Roth, G. A. Atlas of the global burden of stroke (1990–2013): the GBD 2013 study. Neuroepidemiology 45, 230–236 (2015).
Norrving, B. et al. Stroke prevention worldwide — what could make it work. Neuroepidemiology 45, 215–220 (2015).
Roth, G. A. et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 132, 1667–1678 (2015).
Maher, D., Waswa, L., Baisley, K., Karabarinde, A. & Unwin, N. Epidemiology of hypertension in low-income countries: a cross-sectional population-based survey in rural Uganda. J. Hypertens. 29, 1061–1068 (2011).
Ibrahim, M. M. & Damasceno, A. Hypertension in developing countries. Lancet 380, 611–619 (2012).
Kumara, W. A. N., Perera, T., Dissanayake, M., Ranasinghe, P. & Constantine, G. R. Prevalence and risk factors for resistant hypertension among hypertensive patients from a developing country. BMC Res. Notes 6, 373 (2013).
Mehndiratta, M. M. Stroke in Asia: geographical variations and temporal trends. J. Neurol. Neurosurg. Psychiatry 85, 1308–1312 (2014).
Bernick, C. et al. Silent MRI infarcts and the risk of future stroke: the cardiovascular health study. Neurology 57, 1222–1229 (2001).
Lee, S., Shafe, A. C. & Cowie, M. R. UK stroke incidence, mortality and cardiovascular risk management 1999–2008: time-trend analysis from the General Practice Research Database. BMJ Open 1, e000269 (2011).
Soljak, M. et al. Does higher quality primary health care reduce stroke admissions? A national cross-sectional study. Br. J. Gen. Pract. 61, e801–e807 (2011).
Kissela, B. M. et al. Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology 79, 1781–1787 (2012).
George, M. G., Tong, X., Kuklina, E. V. & Labarthe, D. R. Trends in stroke hospitalizations and associated risk factors among children and young adults, 1995–2008. Ann. Neurol. 70, 713–721 (2011).
Feigin, V. L. et al. New strategy to reduce the global burden of stroke. Stroke 46, 1740–1747 (2015).
United Nations General Assembly. Resolution adopted by the General Assembly: 66/2. Political declaration of the high-level meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. World Health Organization http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf (2012).
Lyle, C. A., Bernard, T. J. & Goldenberg, N. A. Childhood arterial ischemic stroke: a review of etiologies, antithrombotic treatments, prognostic factors, and priorities for future research. Semin. Thromb. Hemost. 37, 786–793 (2011).
Murray, C. J. et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet 386, 2145–2191 (2015).
Feigin, V. L. et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. http://dx.doi.org/10.1016/S1474-4422(16)30073-4 (2016).
O'Donnell, M. J. et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case–control study. Lancet 376, 112–123 (2010).
Go, A. S. et al. Heart Disease and Stroke Statistics — 2014 update: a report from the American Heart Association. Circulation 129, e28–e292 (2014).
Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2224–2260 (2012).
Spring, B. et al. Better population health through behavior change in adults: a call to action. Circulation 128, 2169–2176 (2013).
Rose, G. Strategy of prevention: lessons from cardiovascular disease. Br. Med. J. (Clin. Res. Ed.) 282, 1847–1851 (1981).
Goldstein, L. B. et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42, 517–584 (2011).
Tikk, K. et al. Primary preventive potential for stroke by avoidance of major lifestyle risk factors: the European Prospective Investigation into Cancer and Nutrition–Heidelberg cohort. Stroke 45, 2041–2046 (2014).
SPRINT Research Group et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116 (2015).
Ettehad, D. et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387, 957–967 (2016).
Ruff, C. T. et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 383, 955–962 (2014).
Martinez, C. et al. Increasing incidence of non-valvular atrial fibrillation in the UK from 2001 to 2013. Heart 101, 1748–1754 (2015).
Miyasaka, Y. et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 114, 119–125 (2006).
Stefansdottir, H., Aspelund, T., Gudnason, V. & Arnar, D. O. Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. Europace 13, 1110–1117 (2011).
WorldHealth Organization. Prevention of cardiovascular disease: guidelines for assessment and management of cardiovascular risk. http://apps.who.int/iris/bitstream/10665/43685/1/9789241547178_eng.pdf (2007).
WorldHealth Organization. Preventing chronic diseases: a vital investment http://www.who.int/chp/chronic_disease_report/en/ (2005).
Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 14, 32–38 (1985).
Pearson, T. A. et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation 106, 388–391 (2002).
Puska, P. Successful prevention of non-communicable diseases: 25 year experiences with North Karelia project in Finland. Public Health Med. 4, 5–7 (2002).
Miura, K. Epidemiology and prevention of hypertension in Japanese: how could Japan get longevity? EPMA J. 2, 59–64 (2011).
Record, N. B. et al. Community-wide cardiovascular disease prevention programs and health outcomes in a rural county, 1970–2010. JAMA 313, 147–155 (2015).
Emberson, J., Whincup, P., Morris, R., Walker, M. & Ebrahim, S. Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur. Heart J. 25, 484–491 (2004).
Mehta, S. et al. Under-utilisation of preventive medication in patients with cardiovascular disease is greatest in younger age groups (PREDICT-CVD 15). J. Prim. Health Care 3, 93–101 (2011).
Goldstein, L. B. et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 113, e873–e923 (2006).
[No authors listed.] Life After Stroke: New Zealand Guideline for Management of Stroke (Stroke Foundation of New Zealand Inc., 2003).
Cox, J. L., Carr, B., Vallis, T. M., Szpilfogel, C. & O'Neill, B. J. A novel approach to cardiovascular health by optimizing risk management (ANCHOR): a primary prevention initiative examining the impact of health risk factor assessment and management on cardiac wellness. Can. J. Cardiol. 27, 809–817 (2011).
Zannad, F. et al. Prevention of cardiovascular disease guided by total risk estimations — challenges and opportunities for practical implementation: highlights of a CardioVascular Clinical Trialists (CVCT) Workshop of the ESC Working Group on CardioVascular Pharmacology and Drug Therapy. Eur. J. Prev. Cardiol. 19, 1454–1464 (2012).
Ebrahim, S. et al. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst. Rev. 1, CD001561 (2011).
Mc Namara, K. P. et al. Engaging community pharmacists in the primary prevention of cardiovascular disease: protocol for the Pharmacist Assessment of Adherence, Risk and Treatment in Cardiovascular Disease (PAART CVD) pilot study. BMC Health Serv. Res. 10, 264 (2010).
Selak, V. et al. IMProving Adherence using Combination Therapy (IMPACT): design and protocol of a randomised controlled trial in primary care. Contemp. Clin. Trials 32, 909–915 (2011).
Gorelick, P. B. Primary prevention of stroke: impact of healthy lifestyle. Circulation 118, 904–906 (2008).
Jackson, R. et al. Alcohol and ischaemic heart disease: probably no free lunch. Lancet 366, 1911–1912 (2005).
Powers, B. J. et al. The effectiveness of personalized coronary heart disease and stroke risk communication. Am. Heart J. 161, 673–680 (2011).
Sheridan, S. L. et al. The effect of giving global coronary risk information to adults: a systematic review. Arch. Intern. Med. 170, 230–239 (2010).
Guarneri, M., Mercado, N. & Suhar, C. Integrative approaches for cardiovascular disease. Nutr. Clin. Pract. 24, 701–708 (2009).
National Vascular Disease Prevention Alliance. Guidelines for the management of absolute cardiovascular disease risk. Heart Foundation https://heartfoundation.org.au/images/uploads/publications/Absolute-CVD-Risk-Full-Guidelines.pdf (2012).
Goff, D. C. Jr et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 63, 2935–2959 (2014).
Brindle, P. et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ 327, 1267–1270 (2003).
Dalton, A. R., Soljak, M., Samarasundera, E., Millett, C. & Majeed, A. Prevalence of cardiovascular disease risk amongst the population eligible for the NHS Health Check Programme. Eur. J. Prev. Cardiol. 20, 142–150 (2013).
Jansen, J. et al. General practitioners' use of absolute risk versus individual risk factors in cardiovascular disease prevention: an experimental study. BMJ Open 4, e004812 (2014).
World Health Organization. Cardiovascular diseases (CVDs): fact sheet. World Health Organization http://www.who.int/mediacentre/factsheets/fs317/en/ (2016).
Zullig, L. L. et al. Patient-reported medication adherence barriers among patients with cardiovascular risk factors. J. Manag. Care Spec. Pharm. 21, 479–485 (2015).
McKenzie, S. J., McLaughlin, D., Clark, J. & Doi, S. A. The burden of non-adherence to cardiovascular medications among the aging population in Australia: a meta-analysis. Drugs Aging 32, 217–225 (2015).
Wong, M. C. et al. The association between multimorbidity and poor adherence with cardiovascular medications. Int. J. Cardiol. 177, 477–482 (2014).
McLaren, L., McIntyre, L. & Kirkpatrick, S. Rose's population strategy of prevention need not increase social inequalities in health. Int. J. Epidemiol. 39, 372–377 (2010).
[No authors listed.] The 2015/16 health targets. Ministry of Health http://www.health.govt.nz/new-zealand-health-system/health-targets (2015).
Krogsbøll, L. T., Jørgensen, K. J., Grønhøj Larsen, C. & Gøtzsche, P. C. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ 345, e7191 (2012).
Jørgensen, T. et al. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 348, g3617 (2014).
Sacco, R. L., Frieden, T. R., Blakeman, D. E., Jauch, E. C. & Mohl, S. What the million hearts initiative means for stroke: a presidential advisory from the American Heart Association/American Stroke Association. Stroke 43, 924–928 (2012).
Frieden, T. R. & Berwick, D. M. The 'Million Hearts' initiative — preventing heart attacks and strokes. N. Engl. J. Med. 365, e27 (2011).
Sanghavi, D. M. & Conway, P. H. Paying for prevention: a novel test of medicare value-based payment for cardiovascular risk reduction. JAMA 314, 123–124 (2015).
Asch, D. A. et al. Effect of financial incentives to physicians, patients, or both on lipid levels: a randomized clinical trial. JAMA 314, 1926–1935 (2015).
Probst-Hensch, N., Tanner, M., Kessler, C., Burri, C. & Kunzli, N. Prevention — a cost-effective way to fight the non-communicable disease epidemic: an academic perspective of the United Nations High-level NCD Meeting. Swiss Med. Wkly 141, w13266 (2011).
Asaria, P., Chisholm, D., Mathers, C., Ezzati, M. & Beaglehole, R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 370, 2044–2053 (2007).
Khatib, R. et al. Availability and affordability of cardiovascular disease medicines and their effect on use in high-income, middle-income, and low-income countries: an analysis of the PURE study data. Lancet 387, 61–69 (2016).
Notara, V., Panagiotakos, D. B. & Pitsavos, C. E. Secondary prevention of acute coronary syndrome. Socio-economic and lifestyle determinants: a literature review. Cent. Eur. J. Public Health 22, 175–182 (2014).
Boden-Albala, B. & Quarles, L. W. Education strategies for stroke prevention. Stroke 44 (6 Suppl. 1), S48–S51 (2013).
Yusuf, S., Wood, D., Ralston, J. & Reddy, K. S. The World Heart Federation's vision for worldwide cardiovascular disease prevention. Lancet 386, 399–402 (2015).
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. http://www.who.int/nmh/events/ncd_action_plan/en/ (2015).
Cooney, M. T., Dudina, A., D'Agostino, R. & Graham, I. M. Cardiovascular risk-estimation systems in primary prevention: do they differ? Do they make a difference? Can we see the future? Circulation 122, 300–310 (2010).
Mancia, G. et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 31, 1281–1357 (2013).
Hill, S. et al. Absolute risk representation in cardiovascular disease prevention: comprehension and preferences of health care consumers and general practitioners involved in a focus group study. BMC Public Health 10, 108 (2010).
Fagerlin, A., Zikmund-Fisher, B. J. & Ubel, P. A. Helping patients decide: ten steps to better risk communication. J. Natl Cancer Inst. 103, 1436–1443 (2011).
Maniar, S. et al. in PanVascular Medicine 2nd edn (ed. Lanzer, P.) 1695–1718 (Springer, 2015).
Wald, D. S. & Raiman, L. Medication adherence in cardiovascular disease: how to address one of the challenges of preventive medicine. Prim. Care Cardiovasc. J. 6, 60–62 (2013).
Bowry, A. D., Shrank, W. H., Lee, J. L., Stedman, M. & Choudhry, N. K. A systematic review of adherence to cardiovascular medications in resource-limited settings. J. Gen. Intern. Med. 26, 1479–1491 (2011).
Webster, R. & Rodgers, A. Polypill: progress and challenges to global use — update on the trials and policy implementation. Curr. Cardiol. Rep. 17, 121 (2015).
Gaziano, T. A., Opie, L. H. & Weinstein, M. C. Cardiovascular disease prevention with a multidrug regimen in the developing world: a cost-effectiveness analysis. Lancet 368, 679–686 (2006).
[No authors listed]. Community–clinical linkages to improve hypertension identification, management, and control. Association of State and Territorial Health Officials http://www.astho.org/Prevention/Community-Clinical-Linkages-Issue-Brief/ (2015).
Foltz, J. L., Belay, B. & Blackburn, G. L. Improving the weight of the nation by engaging the medical setting in obesity prevention and control. J. Law Med. Ethics 41, 19–26 (2013).
[No authors listed]. Chronic disease prevention and health promotion domains. Centers for Disease Control and Prevention http://www.cdc.gov/chronicdisease/about/foa/docs/four-domains-nov2012.pdf (2012).
[No authors listed]. Cardiovascular disease prevention and control: interventions engaging community health workers. The Community Guide http://www.thecommunityguide.org/cvd/CHW.html (2015).
Feigin, V. L. Stroke in developing countries: can the epidemic be stopped and outcomes improved? Lancet Neurol. 6, 94–97 (2007).
Chandra, V. et al. in Neurological Disorders (eds Jamison, D. T. et al.) 627–643 (Oxford Univ. Press & World Bank, 2006).
Zhao, X. et al. Using a low-sodium, high-potassium salt substitute to reduce blood pressure among Tibetans with high blood pressure: a patient-blinded randomized controlled trial. PLoS ONE 9, e110131 (2014).
Luo, B., Wan, L., Liang, L. & Li, T. The effects of educational campaigns and smoking bans in public places on smokers' intention to quit smoking: findings from 17 cities in China. BioMed Res. Int. 2015, 853418 (2015).
Selmer, R. M. et al. Cost and health consequences of reducing the population intake of salt. J. Epidemiol. Commun. Health 54, 697–702 (2000).
Johnson, R. K. et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 120, 1011–1020 (2009).
Martineau, F., Tyner, E., Lorenc, T., Petticrew, M. & Lock, K. Population-level interventions to reduce alcohol-related harm: an overview of systematic reviews. Prev. Med. 57, 278–296 (2013).
Wilson, N. Salt tax could reduce population's salt intake. BMJ 329, 918 (2004).
Hopkins, D. P. et al. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am. J. Prev. Med. 20, 16–66 (2001).
Goodchild, M., Perucic, A. M. & Nargis, N. Modelling the impact of raising tobacco taxes on public health and finance. Bull. World Health Organ. 94, 250–257 (2016).
World Health Organization. WHO report on the global tobacco epidemic, 2015: raising taxes on tobacco. World Health Organization http://apps.who.int/iris/bitstream/10665/178574/1/9789240694606_eng.pdf (2015).
Ruff, R. R. & Zhen, C. Estimating the effects of a calorie-based sugar-sweetened beverage tax on weight and obesity in New York City adults using dynamic loss models. Ann. Epidemiol. 25, 350–357 (2015).
Briggs, A. D. et al. Overall and income specific effect on prevalence of overweight and obesity of 20% sugar sweetened drink tax in UK: econometric and comparative risk assessment modelling study. BMJ 347, f6189 (2013).
WHO technical staff. Reducing consumption of sugar-sweetened beverages to reduce the risk of unhealthy weight gain in adults. World Health Organization http://www.who.int/elena/bbc/ssbs_adult_weight/en/ (2014).
Meier, P. S. et al. Estimated effects of different alcohol taxation and price policies on health inequalities: a mathematical modelling study. PLoS Med. 13, e1001963 (2016).
Delcher, C., Maldonado-Molina, M. M. & Wagenaar, A. C. Effects of alcohol taxes on alcohol-related disease mortality in New York State from 1969 to 2006. Addict. Behav. 37, 783–789 (2012).
Wagenaar, A. C., Tobler, A. L. & Komro, K. A. Effects of alcohol tax and price policies on morbidity and mortality: a systematic review. Am. J. Public Health 100, 2270–2278 (2010).
Chaloupka, F. J., Grossman, M. & Saffer, H. The effects of price on alcohol consumption and alcohol-related problems. Alcohol Res. Health 26, 22–34 (2002).
Elder, R. W. et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am. J. Prev. Med. 38, 217–229 (2010).
Doran, C. M., Byrnes, J. M., Higashi, H. & Truong, K. Revenue implications to the Vietnamese government of using taxes to curb cigarette smoking. Addict. Behav. 35, 1089–1093 (2010).
Andreyeva, T., Chaloupka, F. J. & Brownell, K. D. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Prev. Med. 52, 413–416 (2011).
Doran, C. M., Byrnes, J. M., Cobiac, L. J., Vandenberg, B. & Vos, T. Estimated impacts of alternative Australian alcohol taxation structures on consumption, public health and government revenues. Med. J. Aust. 199, 619–622 (2013).
Feigin, V. L., Krishnamurthi, R., Barber, P. A. & Arroll, B. Stroke prevention in New Zealand: can we do better? Int. J. Stroke 9, 61–63 (2013).
Murray, C. J. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2197–2223 (2012).
Lozano, R. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2095–2128 (2012).
Cappuccio, F. Epidemiologic transition, migration and cardiovascular disease. Int. J. Epidemiol. 33, 387–388 (2004).
Licskai, C., Sands, T. W. & Ferrone, M. Development and pilot testing of a mobile health solution for asthma self-management: asthma action plan smartphone application pilot study. Can. Respir. J. 20, 301–306 (2013).
Brouillette, R. M. et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PLoS ONE 8, e65925 (2013).
Buller, D. B., Borland, R., Bettinghaus, E. P., Shane, J. H. & Zimmerman, D. E. Randomized trial of a smartphone mobile application compared to text messaging to support smoking cessation. Telemed. J. E Health 20, 206–214 (2014).
Ly, K. H., Carlbring, P. & Andersson, G. Behavioral activation-based guided self-help treatment administered through a smartphone application: study protocol for a randomized controlled trial. Trials 13, 62 (2012).
Carter, M. C., Burley, V. J., Nykjaer, C. & Cade, J. E. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J. Med. Internet Res. 15, e32 (2013).
[No authors listed.] Surveillance Strategy: a strategy for improving the Centers for Disease Control and Prevention's activities in public health surveillance. Centers for Disease Control and Prevention http://www.cdc.gov/ophss/docs/cdc-surveillance-strategy-final.pdf (2014).
Spring, B. et al. Multiple behavior changes in diet and activity: a randomized controlled trial using mobile technology. Arch. Intern. Med. 172, 789–796 (2012).
Recio- Rodríguez, J. I. et al. Effectiveness of a smartphone application for improving healthy lifestyles, a randomized clinical trial (EVIDENT II): study protocol. BMC Public Health 14, 254 (2014).
Bond, D. S. et al. B-MOBILE — a smartphone-based intervention to reduce sedentary time in overweight/obese individuals: a within-subjects experimental trial. PLoS ONE 9, e0100821 (2014).
Glynn, L. G. et al. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomised controlled trial. Br. J. Gen. Pract. 64, e384–e391 (2014).
Martin, C. K. et al. Efficacy of SmartLossSM, a smartphone-based weight loss intervention: results from a randomized controlled trial. Obesity 23, 935–942 (2015).
Stephens, J. D., Yager, A. M. & Allen, J. Smartphone technology and text messaging for weight loss in young adults: a randomized controlled trial. J. Cardiovasc. Nurs. http://dx.doi.org/10.1097/JCN.0000000000000307 (2015).
Eyles, H. et al. Using mobile technology to support lower-salt food choices for people with cardiovascular disease: protocol for the SaltSwitch randomized controlled trial. BMC Public Health 14, 950 (2014).
Piette, J. D. et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed. J. E Health 18, 613–620 (2012).
Block, G. et al. Diabetes prevention and weight loss with a fully automated behavioral intervention by e-mail, web, and mobile phone: a randomized controlled trial among persons with prediabetes. J. Med. Internet Res. 17, e240 (2015).
Rodgers, A. et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob. Control 14, 255–261 (2005).
Free, C. et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 378, 49–55 (2011).
Chow, C. K. et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA 314, 1255–1263 (2015).
Proudfoot, J. et al. Impact of a mobile phone and web program on symptom and functional outcomes for people with mild-to-moderate depression, anxiety and stress: a randomised controlled trial. BMC Psychiatry 13, 312 (2013).
World Health Organization. mHealth: new horizons for health through mobile technologies. http://apps.who.int/iris/bitstream/10665/44607/1/9789241564250_eng.pdf (2011).
Burke, L. E. et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 132, 1157–1213 (2015).
Nasser, F. B. & Trevena, L. There's an app for that: a guide for healthcare practitioners and researchers on smartphone technology. Online J. Public Health Inform. 7, e218 (2015).
Morgan, J. The power of the App: can mobile-technology save lives? Lancet Neurol. 15, 668 (2015).
World Health Organization. Global status report on noncommunicable diseases 2010 http://www.who.int/nmh/publications/ncd_report_full_en.pdf (2011).
Fustinoni, O. & Biller, J. Ethnicity and stroke: beware of the fallacies. Stroke 31, 1013–1015 (2000).
Sacco, R. L. et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am. J. Epidemiol. 147, 259–268 (1998).
Stewart, J. A., Dundas, R., Howard, R. S., Rudd, A. G. & Wolfe, C. D. Ethnic differences in incidence of stroke: prospective study with stroke register. BMJ 318, 967–971 (1999).
van Rossum, C. T., van de Mheen, H., Breteler, M. M., Grobbee, D. E. & Mackenbach, J. P. Socioeconomic differences in stroke among Dutch elderly women: the Rotterdam Study. Stroke 30, 357–362 (1999).
Feigin, V. L. et al. 30-year trends in stroke rates and outcome in Auckland, New Zealand (1981–2012): a multi-ethnic population-based series of studies. PLoS ONE 10, e0134609 (2015).
Mullen Conley, K. et al. Kids Identifying and Defeating Stroke (KIDS): development and implementation of a multiethnic health education intervention to increase stroke awareness among middle school students and their parents. Health Promot. Pract. 11, 95–103 (2010).
World Health Organization. Adherence to long-term therapies: evidence for action. World Health Organization http://www.who.int/chp/knowledge/publications/adherence_introduction.pdf (2003).
Davis, P. C. Jr & Rankin, L. L. Guidelines for making existing health education programs more culturally appropriate. Am. J. Health Educ. 37, 250–252 (2006).
Peñalvo, J. L. et al. The Program SI! intervention for enhancing a healthy lifestyle in preschoolers: first results from a cluster randomized trial. BMC Public Health 13, 1208 (2013).
Wen, X., Kong, K. L., Eiden, R. D., Sharma, N. N. & Xie, C. Sociodemographic differences and infant dietary patterns. Pediatrics 134, e1387–e1398 (2014).
Foltz, J. L. et al. Population-level intervention strategies and examples for obesity prevention in children. Annu. Rev. Nutr. 32, 391–415 (2012).
Hickey, A. et al. Stroke awareness in the general population: knowledge of stroke risk factors and warning signs in older adults. BMC Geriatr. 9, 35 (2009).
Jones, S. P., Jenkinson, A. J., Leathley, M. J. & Watkins, C. L. Stroke knowledge and awareness: an integrative review of the evidence. Age Ageing 39, 11–22 (2010).
Ellis, C., Wolff, J. & Wyse, A. Stroke awareness among low literacy Latinos living in the South Carolina low country. J. Immigr. Minor. Health 11, 499–504 (2009).
Ryan, T. Stroke awareness among British ethnic minorities. Br. J. Commun. Nurs. 15, 381–384 (2010).
Ellis, C. & Egede, L. E. Racial/ethnic differences in stroke awareness among veterans. Ethn. Dis. 18, 198–203 (2008).
Alkadry, M. G. & Tower, L. E. The effect of rurality and gender on stroke awareness of adults in West Virginia. J. Health Hum. Serv. Admin. 33, 63–93 (2010).
Hodgson, C. Community outreach for stroke education. Stroke 39, 2189–2190 (2008).
Sullivan, K. A. & Katajamaki, A. Stroke education: promising effects on the health beliefs of those at risk. Top. Stroke Rehabil. 16, 377–387 (2009).
Tadros, A. et al. Emergency medical services-based community stroke education: pilot results from a novel approach. Stroke 40, 2134–2142 (2009).
Kim, Y. S. et al. Stroke awareness decreases prehospital delay after acute ischemic stroke in Korea. BMC Neurol. 11, 2 (2011).
Bray, J. E., Mosley, I., Bailey, M., Barger, B. & Bladin, C. Stroke public awareness campaigns have increased ambulance dispatches for stroke in Melbourne, Australia. Stroke 42, 2154–2157 (2011).
Rothwell, P. M. Lack of research funding for stroke. Int. J. Stroke 2, 73 (2007).
[No authors listed.] Final report of the Stroke Progress Review Group – January 2012. NIH National Institute of Neurological Disorders and Stroke http://www.ninds.nih.gov/about_ninds/groups/stroke_prg/01-2012-stroke-prg-report.htm (2012).
Yusuf, S. et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N. Engl. J. Med. 371, 818–827 (2014).
[No authors listed.] Be he@lthy, be mobile. ITU http://www.itu.int/en/ITU-D/ICT-Applications/eHEALTH/Pages/Be_Healthy.aspx (2014).
Collins, F. S. & Varmus, H. A new initiative on precision medicine. N. Engl. J. Med. 372, 793–795 (2015).
[No authors listed.] Cardiovascular disease prevention and control. Translating evidence into practice. World Health Organization http://apps.who.int/iris/bitstream/10665/43235/1/9241593253_eng.pdf (2005).
Acknowledgements
V.L.F. was partly funded by the Health Council of New Zealand, the Brain Research New Zealand Centre of Research Excellence, the “Ageing Well” Programme of the National Science Challenge, and the Ministry of Business, Innovation and Employment of New Zealand. G.A.R. has grant funding from the US National Institute on Ageing and Medtronic Philanthropy. We would like to thank Barbara Bowman at the Centers for Disease Control and Prevention for her valuable comments on early version of the manuscript. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; NIH; Centers for Disease Control and Prevention; or the U.S. Department of Health and Human Services.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content and reviewed and/or edited the manuscript before submission. V.L.F. wrote the article.
Corresponding author
Ethics declarations
Competing interests
V.L.F. declares that Stroke Riskometer app is copyrighted by the Auckland University of Technology, and funds resulting from the sale of the professional version of this app will be used for further research and education for stroke prevention. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Feigin, V., Norrving, B., George, M. et al. Prevention of stroke: a strategic global imperative. Nat Rev Neurol 12, 501–512 (2016). https://doi.org/10.1038/nrneurol.2016.107
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.107
This article is cited by
-
Comparison of performances of SIREN or MFSRS in stroke risk prediction in an African environment
BMC Public Health (2024)
-
Trends in all-cause mortality and leading causes of death from 2009 to 2019 among older adults in China
BMC Geriatrics (2023)
-
CircDLGAP4 overexpression relieves oxygen-glucose deprivation-induced neuronal injury by elevating NEGR1 through sponging miR-503-3p
Journal of Molecular Histology (2022)
-
Personalized Spiking Neural Network Models of Clinical and Environmental Factors to Predict Stroke
Cognitive Computation (2022)
-
Can quantifying morphology and TMEM119 expression distinguish between microglia and infiltrating macrophages after ischemic stroke and reperfusion in male and female mice?
Journal of Neuroinflammation (2021)