Abstract
Objective:
To test the efficacy of single family room (SFR) neonatal intensive care unit (NICU) designs, questions regarding patient medical progress and relative patient safety were explored. Addressing these questions would be of value to hospital staff, administrators and designers alike.
Study Design:
This prospective study documented, by means of Institution Review Board-approved protocols, the progress of patients in two contrasting NICU designs. Noise levels, illumination and air quality measurements were included to define the two NICU physical environments.
Result:
Infants in the SFR unit had fewer apneic events, reduced nosocomial sepsis and mortality, as well as earlier transitions to enteral nutrition. More mothers sustained stage III lactation, and more infants were discharged breastfeeding in the SFR.
Conclusion:
This study showed the SFR to be more conducive to family-centered care, and to enhance infant medical progress and breastfeeding success over that of an open ward.
Similar content being viewed by others
Introduction
The past three decades have seen premature births increase to 12.8% of all live births in the United States.1 As medical advances increase the survival of these preterm infants, the need for neonatal intensive care units (NICUs) increases concomitantly. This growth is occurring within a health-care environment that is increasingly competitive and consumer driven. As development-based, family-centered care shifts the focus from the preterm infant alone to the parent–child dyad, the design of NICU environments is responding by trending away from multi-patient, open-bay wards (OPEN) to single family room (SFR) floor plans.2, 3 As anticipated by White,4 private rooms favor patients and their parents by affording greater privacy, environmental control and space customization to the infant's individual medical and developmental needs. However, the isolation of neonates in separate private rooms prompts concerns about the relative safety of the SFR compared with the open-ward design. Consequently, health-care staff have met the challenge of this transition with mixed enthusiasm, varying with experience and employment position.5, 6 Furthermore, hospital budgets can be taxed by the need to commit greater space and financial resources to the construction of an SFR facility.
Documentation of the efficacy of SFR design in enhancing actual patient progress has been virtually absent from the literature and would contribute to cost-benefit analyses, integral in the decision to transition away from an open-ward facility.7, 8 In 2008, the Cabell Huntington Hospital in Huntington, West Virginia, completed the construction of a 1302 m2 SFR, level III NICU to replace an older, open-bay ward with only 382 m2 floor space, affording only 3.35 m2 per patient. Individual SFR rooms averaged 16 m2 of dedicated patient space per room.6 Transition to the new SFR facility, which more than tripled the size of the old unit, was made with no new staff hires. Thus, the new construction project provided an opportunity for a prospective comparison of patient progress in the two contrasting facility designs with the same staff delivering care in both units.
Methods
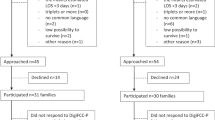
Recognizing the wide range of acuity presenting to a level III NICU, it was deemed important to subgroup, or ‘triage,’ study subjects by prognosis. Infants admitted to each NICU environment were assessed by the research neonatologist and assigned the Physician's Estimate of Mortality Risk (PEMR)9 codes as initial indices of illness severity. Using this scale, acuity increases with the PEMR value, with PEMR 4 being the most severely ill child included in the study. This ‘triage’ protocol was less complicated to administer than the Neonatal Therapeutic Intervention Survey Score adopted by Wielenga et al.10 and correlated positively with length of stay (LOS). Inclusion of infants in the study was suspended for 90 days before and after relocation to avoid the time intervals around and during the move to the new SFR facility, and to ensure that no infant had spent time in both units. This protocol generated original databases of 133 subjects in the OPEN unit and 107 in the SFR.
To minimize variability in the statistical comparison groups, subjects from the original study populations were pair matched according to PEMR, gender and gestational age. Pair matching study infants generated comparable demographic subgroups from each facility design with 81 subjects in each. As the majority of NICU admissions fall within PEMR groups 2 and 3, these two groups were combined for analysis. PEMR 4s were considered separately to determine whether severely ill infants progressed better in either of the two study facilities. Data for each PEMR subgroup were compiled and averaged, and means were compared between the two NICU units for statistical significance using the Mann–Whitney rank-sum nonparametric analysis.
Owing to the prevalence of ‘out-borns’ and transfers in the PEMR 1 group, as well as ‘imminent’ deaths in the PEMR 5 category, these groups were excluded from the final analysis in both facilities. Although deceased infants were excluded, mortality rates over the course of the study were monitored in both facilities and separated by prognosis into ‘expected’ (PEMR 5) and ‘unexpected’ (PEMRs 1 to 4) categories for comparison. Causes of death were recorded, as were nosocomial sepsis events with their causative pathogens and antibiotic sensitivities. Blood infections were considered nosocomial if they occurred after 7 days of hospitalization and were confirmed by laboratory culture. Mortality and nosocomial events were determined for the entire, unmatched study populations to ensure a larger statistical subject pool.
Selected growth and developmental parameters were monitored in each facility to determine differences in patient medical progress between the two designs. Discharge weights, lengths and head circumferences were compared with those taken at the time of admission as indices of overall growth in body mass and stature during hospitalization. Similarly, respiratory and nutritional parameters were monitored as indices of developmental progress. Respiratory data collected for comparison from the two units included conventional mechanical ventilation times, continuous positive airway pressure days, total apnea events, apnea events per day and days requiring caffeine administration. Apnea events and caffeine use were compared in more apnea-prone infants with gestational ages ⩽36 weeks. Nutritional parameters recorded as indices of gastrointestinal maturation included days on total parenteral nutrition (TPN) and intervals (days) to enteral nutrition. TPN data were collected from infants in both units with LOSs ⩾14 days to eliminate bias from ‘short-stay’ subjects who did not require supplemental intravenous nutrition.
A companion study of breastfeeding success was conducted from pair-matched study populations. Inclusion in this study group was predicated on having sustained breast milk production for 14 days postpartum (stage III lactation).11 Numbers of mothers sustaining this stage of mature lactogenesis were compared across facility designs. Infants in the two facilities were compared according to total NICU days on maternal breast milk (MBM), the ratios of MBM days per days of hospitalization (LOS) and the mother–child dyads discharged breastfeeding.
Sound, light and air quality measurements were conducted in both facilities by a consultant from Performance HVAC (Heating, Ventilation, Air Conditioning) Systems (Bramwell, WV, USA). Using a Quest Soundprobe DL-2 (Quest Technologies, Oconomowoc, WI, USA), A-weighted, slow-response sound measurements were made within a closed OmniBed (General Electric Company, www.gehealthcare.com) in bays or rooms located near the unit entrances and nursing stations, as well as at the intermediate and remote sites of both facilities. To track ambient noise, measurements were timed to include peak activity (shift change and visitation) and ‘quiet’ intervals.
Light intensity measurements used an Extech Model 401036 data logging light meter (Extech Instrument Corporation, Waltham, MA, USA), and were made at the bed level in early afternoon on sunny days to determine the maximum brightness and the capacity to darken the facilities during peak natural lighting.
Interior air quality measurements used a Fluke 983 particle counter (Fluke Corporation, Everett, WA, USA) and a TSI 982 indoor air quality meter (TSI, Shoreview, MN, USA). Particulate counts (2 to 10 μm) per 0.1 ft3, air temperature, relative humidity, carbon monoxide levels, carbon dioxide levels and volatile organic compounds were recorded to quantify the physical aspects of the two NICU environments.
Results
NICU physical environments
Table 1 summarizes the air quality, sound and light parameters measured in the two NICU facilities. Air temperature and relative humidity were uniform across all test sites within each facility. Relative humidity levels, recorded in both units with air handling equipment in heating mode, were improved in the SFR unit. As carbon monoxide and volatile organic compound levels were virtually absent in both facilities, they were not tabulated. Particle counts did reflect air quality differences between the two units. Particulates showed a gradient within the OPEN unit, which peaked near the entry/nursing station and declined dramatically with more remote locations. Counts were more uniform across measurement sites in the SFR and approximated the lowest levels seen in the OPEN unit.
Excluding task lighting for medical procedures, light sources differed markedly from primarily artificial fluorescents in the OPEN unit to primarily natural light in the SFR. In the OPEN facility, lighting was not readily adjustable to patient needs, and individualization was improvised using blanket shields over the isolettes as required. However, general illumination intensities at unshielded bed levels were similar in both facilities, and day/night cycling was commonly practiced in both units.
Ambient sound levels were dramatically different in the two facilities. Peak noise criterion levels in the OPEN unit correlated with staff activity and visitation, being louder near the entry/nursing station during shift change/visitation and moving to remote sites during ‘quiet’ times. Considering a midrange human voice frequency of 2000 Hz, loudness equivalence (Leq) levels were as much as 20 dBA higher in the open-bay facility and corresponded with high staff activity sites, suggesting that much of the ambient noise was conversational. In the SFR, sound levels were notably lower, were more uniform across time and measurement sites and were independent of peak staff activity.
Comparative patient progress
With the combined PEMRs 2 and 3 (Table 2), mean LOSs were reduced by ∼2 days (11%) in the SFR facility, but the difference was not statistically significant. Respiratory and gastrointestinal maturation showed significantly better progress in the SFR environment, whereas traditional growth parameters, such as weight and length gains, trended toward being better in the OPEN unit, but differences were not statistically significant.
With infants hospitalized ⩾2 weeks, TPN days showed a statistically significant 30% reduction in the SFR. OPEN unit neonates spent significantly more of their hospital stay on TPN, 32 versus 17% in the SFR group. Infants in the SFR were transitioned to enteral nutrition significantly earlier, with the intervals from admission shortened by 45% for MBM and by 11% for formula starts.
The PEMR 2 and 3 neonates trended toward reduced mechanical ventilation support with less time spent on conventional mechanical ventilation. Continuous positive airway pressure times were similar in both groups, but fewer SFR infants required this level of respiratory assistance. Apnea-prone infants (gestational age ⩽36 weeks) from this PEMR group showed a highly significant 57% reduction in total apnea events, which persisted after normalization for differences in LOS and correction for conventional mechanical ventilation times. Caffeine days only showed a slight, insignificant reduction in SFR infants from this gestational age group.
The study subject group that comprised PEMR 4s showed a higher incidence of lower-birth-weight babies in the SFR facility, with the mean admission weight being 376 g below that of the OPEN unit (Table 3). In addition, pair matching reduced the number of infants in this PEMR category to six, making statistical comparisons of the differences between the two facilities unremarkable. However, there were some important trends in patient progress with this group that merit mention. Even with a greater incidence of low-birth-weight infants, mean LOSs were shortened by 2 days (3%) in the SFR facility. Interestingly, this lower-birth-weight SFR group showed comparable weight, length and head circumference gains per day relative to the OPEN cohort. Nutritionally, the SFR group showed comparable times on TPN, with a shortened interval to enteral feeding related to earlier formula starts. Yet, more maternal/infant dyads were on MBM in the private rooms. With regard to respiratory progress, the total days of caffeine administration were comparable between the two facilities, but apnea events, conventional mechanical ventilation and continuous positive airway pressure times were reduced in the SFR.
Sustained lactation
Lactation and breastfeeding success were notably improved in the private-room environment (Table 4). Considering only those mothers who sustained lactation for 14 days postpartum, the SFR unit showed more mothers achieving this benchmark and 20% more infants were discharged breastfeeding. Not only were the total days on MBM significantly better in the SFR but the mean ratio of MBM days/LOS also showed infants in the SFR to have spent 90% of their hospital stay on breast milk compared with only 66% in the OPEN unit.
Mortality and nosocomial sepsis events
Although PEMR 5s (imminent death) were not included in patient progress data analyses, all mortality events were recorded for comparison. Mortality incidences in the two facilities over the study time intervals showed 11 events in the OPEN unit and 9 in the SFR. In the OPEN facility, 3 of the 11 mortality events were unexpected with causes of death of necrotizing enterocolitis, severe intraventricular hemorrhage and nosocomial sepsis. The SFR showed only one unexpected event from necrotizing enterocolitis. Nosocomial sepsis incidence (Table 5) in the SFR was reduced to nearly half the rate seen in the OPEN unit. Except for one methicillin-resistant Staphylococcus aureus infection in the open ward, all nosocomial pathogens were sensitive to first-tier antibiotics.
Discussion
The ability to adapt the hospital environment to individual developmental needs of neonates without compromising patient safety has long been a goal of neonatal intensive care, and, when practiced, can enhance the medical progress of critically ill infants.12 Yet, neonatal intensive care has been among the last health-care specialties to move away from multi-patient wards to private rooms. Concerns related to cost, workload and patient safety have contributed to this hesitancy. With the relative scarcity of private-room NICUs, little research has been conducted to determine whether neonatal progress improved sufficiently in this environment to justify new construction costs.
NICU physical environments
It has been shown that light and noise reduction in a typical open-ward facility leads to reduced ventilator times and LOSs.13 Recommended standards for newborn intensive care units regarding ambient noise, light, temperature and humidity are available as guidelines and for comparison with study parameter measurements.14, 15 Air quality, sound and lighting from the two contrasting NICU designs revealed noteworthy differences. Generally speaking, the SFR was found to be a quieter, more hygienic facility with controllable natural lighting. Interestingly, staff activity seemed to be implicated in environmental quality of the open ward, and its impact was apparent with noise, airborne particulates and CO2 levels. Much of the activity typically associated with health-care delivery in an OPEN unit is unavoidable, but can be minimized in a private room environment by isolating individual infants from activity associated with the care of other neonates around them.
Exposure of preterm infants to excessive sound has been implicated in sleep pattern disruption with potential negative impact on nervous system development, and is more pronounced in areas where staff congregate.16 Excessive ‘unpredictable’ ambient sound may exacerbate neonatal attention difficulty, and can mask maternal voice frequencies resulting in delayed recognition.17 Ambient noise in the OPEN unit exceeded the recommended standard Leq of 45 dBA where staff activity was greatest. During work hours, the remote patient care areas were louder and high noise criterion levels shifted to areas around the entry/nursing station at shift change and visitation times. As the Leq of a midrange human voice frequency (2000 Hz) showed the same variation pattern, it seemed that human conversation was a major contributor to excess noise. Individual rooms of the SFR were considerably quieter, testing ∼12 dBA below the Leq 45 dBA standard, and did not show variation with staff activity.
Not only did human activity contribute to noise levels in the open ward but it also seemed to impact air quality as well. Gradients of particulates and CO2 were highest around the entry/nursing station of the OPEN unit and decreased with remote locations. The same measurements in the rooms of the SFR were appreciably lower and without gradient variation.
Light intensities were comparable in both facilities and controllable for day/night cycling well within the recommended range of 1 to 600 lux. However, light sources differed dramatically. Overhead fluorescent lighting was the primary source in the open ward at all times, and individual patient adjustments were made with blanket covers over isolettes. Natural light, controllable with darkening window blinds, was the primary source during daylight hours in the SFR, with artificial lighting used only for medical procedures or as ambient evening lighting. Light cycling has been shown to facilitate development of circadian sleep patterns,18, 19 to enhance earlier tolerance of enteral feeding, to decrease ventilator support and to improve movement and muscle tone.20
Comparative patient progress
Four traditional indices of neonatal patient progress, weight, length and head circumference gains during hospitalization and overall LOSs, were monitored in this study and were not significantly different with either PEMR subgroup. Anecdotal evidence from researchers suggested that these indices were all multivariate and not dependent on infant medical progress alone. In the OPEN unit, with sporadic availability of parents, procedures requiring parental consents and predischarge education were sometimes delayed when parents could not be accessed in a timely manner. Delays such as these, occurring around the time of discharge, would coincide with the more rapid growth phase of a stable infant's hospital stay20 and would bias their weight and length gains artificially higher. In addition, the earlier physiological stabilization of an infant in the SFR would lead to earlier discharge with less time in the NICU to accrue body mass and length, biasing their weights and lengths downward. These unanticipated LOS anomalies would be more influential statistically with shorter hospital stays, as seen with PEMRs 2 and 3, and may explain, in part, the lack of significant differences seen with these variables.
Although shortening the LOS in the SFR by 2 days was not statistically significant, it would be economically consequential. In a mid-sized, level III NICU admitting 700 patients per year at an average cost of $2500 per day, shortening LOS yields an annual saving of approximately $1.75 million per patient day. Furthermore, reducing TPN time and shortening time on respiratory support alone could contribute to significant economic savings.
With the moderately ill PEMR group, the SFR cohort transitioned from TPN to enteral nutrition more quickly, showed significantly less apnea with trends toward reduced times on respiratory assistance and earlier discharge. As these variables reflect the extents of developmental maturation and physiological stability, the SFR environment was more conducive to neonatal medical progress than was that of the OPEN facility. If safe swallowing and oral feeding were prerequisite for discharge, accelerating an infant's progression to this stage of maturation would shorten LOS. The neural coordination of sucking, swallowing and breathing, such that swallowing occurs without apnea and at the safer, end-inspiratory phase of breathing, is dependent on brainstem maturation.21, 22 Although true cause–effect relationships cannot be confirmed by this study, it can be speculated that the less chaotic environment of the SFR facilitated neurological maturation in these preterm infants. As formula starts were not appreciably different between the two units, earlier transition to enteral feeding was primarily due to significantly earlier MBM starts in the SFR. Earlier MBM starts likely reflect the increased maternal presence and earlier tolerance of enteral MBM feedings with infants in private rooms.
The enhanced progress of moderately ill PEMR patient categories in the SFR prompts the question of its efficacy with more acutely ill infants. The more seriously ill PEMR 4 subgroup, unfortunately, included too few subjects for valid statistical conclusions compounded by a preponderance of low-birth-weight infants. Regardless, some relevant trends could be identified. Even with birth weights averaging 376 g below those seen in the OPEN facility, infants in the SFR showed weight and length gains similar to their OPEN cohort, and were discharged an average of 2 days earlier. Half of the infants in the SFR received MBM enteral feeds compared with only one in the OPEN unit. It seemed that the SFR environment enhanced the medical progress of both moderately and seriously ill preterm infants, but further studies with larger numbers of seriously ill infants are required to confirm the trends seen within this category of patient acuity.
Sustained lactation and breastfeeding
A number of environmental factors can impact postpartum milk production. Comfortable, tranquil environments that encourage maternal–infant interaction and facilitate elective kangaroo care can have mutual benefits for mothers and infants. Mothers experience increased milk production and ‘let down,’ while infants exhibit better sleep patterns with more stable heart rates, less apnea and better temperature regulation.11, 23 Mother–infant dyads for this phase of the study were required, for inclusion, to have progressed beyond the stage II postpartum increase in milk production, and to have been in active stage III lactation. Sustainment of this stage of lactation would be more susceptible to environmental influences and more likely to differ in the two NICU facilities. Lactation and ultimate breastfeeding success is multivariate and dependent on interactions between both members of the mother–infant dyad. Hypothetically, the privacy and comfort aspects of the SFR environment should facilitate elective kangaroo care and keep mothers in close proximity to their newborns for longer periods of time. Similarly, infants should be less stressed in the more controlled environments of private rooms. Both of these attributes of the SFR should enhance lactation and improve the success of breast pumping and, ultimately, that of breastfeeding. Results showed this to have been the case. More mothers sustained stage III lactation in the SFR, with their infants averaging significantly more of their hospital stay on MBM. Subsequently, more mother–infant dyads were discharged breastfeeding from the SFR.
Patient safety
Preterm infants are intrinsically susceptible to infection because of their immunological deficiencies and immature skin and gastrointestinal mucosal barriers.24 Moreover, most pediatric nosocomials are secondary bloodstream infections associated with intravascular devices,25 and can be exacerbated by overcrowding. Patient overcrowding can lead to decreased hand washing frequency or efficiency as staff hurry from one patient to another. Delayed enteric nutrition may also contribute by increasing the time on TPN, concomitantly increasing the extrinsic risks of nosocomial sepsis. Shortening TPN time, as seen in the SFR, may have had a role in reducing the bloodstream infection incidence seen in this study. In addition, the isolation of patients in private rooms, each with readily accessible hand washing stations, should reduce the likelihood of rushed transitions from one infant to another without adequate hand washing between patients. Finally, reduced apnea would lead to less nursing intervention and reduced risk of cross-contamination.
Interestingly, the isolation of patients in private rooms has not been perceived by NICU staff as totally beneficial. Reduced line of sight in an SFR facility, with more reliance on electronics for patient monitoring and coworker communication, represent major departures from the traditional norms of neonatal intensive care in open-bay wards. Consequently, concerns about patient safety in SFR facilities among staff, particularly those experienced with open-ward practice, would be expected and have been documented.6 Considering the reductions in ‘unexpected’ mortality, apnea and nosocomial sepsis seen with the SFR in this study, no evidence was found to suggest that private rooms were less safe than the open-bay floor plan. Instead, infants in the PEMR 2 and 3 group, representing the majority of typical NICU admissions, showed more rapid medical progress in the SFR than did their OPEN cohort.
Conclusion
The SFR design provided a quieter, more controllable environment for sick neonates, and their medical progress was improved over that of the open-bay unit without increased safety risks. The efficacy of private-room NICUs in enhancing patient progress is multivariate and difficult to quantify with absolute certainty as to cause–effect relationships. Considering the improved nutritional, respiratory and breastfeeding progress seen in the SFR, one common denominator emerges as a major advantage of the SFR over the OPEN design. That advantage lies in providing more opportunities for parents and infants to remain in close contact throughout their hospital stay. Having parents, particularly mothers, close by the bedside not only minimized discharge delays by facilitating the mechanics of procedural consents and neonatal care education but also facilitated elective kangaroo care, providing for earlier physiological stabilization of preterm infants and enhanced MBM production.
References
Lackritz E . Chief, Maternal and Infant Health Branch, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention U.S. Senate Sub-committee Report. 2004.
Conner JM, Nelson EC . Neonatal intensive care: satisfaction measured from a parent's perspective. Pediatrics 1999; 103 (1): 336–349.
Floyd AMD . Challenging designs of neonatal intensive care units. Crit Care Nurse 2005; 25 (5): 59–66.
White RD . Individual rooms in the NICU—an evolving concept. J Perinatol 2003; 23 (Suppl 1): S22–S24.
Stevens DC, Helseth CC, Khan MA, Munson DP, Smith TJ . Neonatal intensive care nursery staff perceive enhanced workplace quality with the single-family room design. J Perinatol 2010; 30 (5): 352–358.
Domanico R, Davis DK, Coleman F, Davis Jr BO . Documenting the NICU design dilemma: parent and staff perceptions of open ward versus single family room units. J Perinatol 2010; 30 (5): 343–351.
Oelrich T . Single Room NICU: Fad or Future. AIA Academy of Architecture for Health Conference: Denver, CO, 2003.
Rosenblum D . Single Family Room Care: Before and After Data. The Physical and Developmental Environment of the High-Risk Infant Conference: Clearwater, FL, 2005.
Gray JE, Richardson DK, McCormick MC, Workman-Daniels K, Goldman DA . Neonatal Therapeutic Intervention Scoring System: a therapy-based severity-of-illness index. Pediatrics 1992; 90 (4): 561–567.
Wielenga JM, Smit BJ, Unk LKA . How satisfied are parents supported by nurses with the NIDCAP model of care for their preterm infant. J Nurs Care Qual 2006; 21 (1): 41–48.
Lawerence R . Breastfeeding: A Guide for the Medical Professional, 6th edn. Elsevier/Saunders: Philadelphia, PA, 2005.
Als H, Lawhon G, Duffy FH, McAnulty GB, Gibes-Grossmal R, Blickman JG . Individualized developmental care for the very low birth-weight preterm infant. JAMA 1994; 272 (11): 853–858.
Altimer LB, Eichel M, Warner B, Tedeschi L, Brown B . Developmental care: changing the NICU physically and behaviorally to promote patient outcomes and contain costs. Neonatal Intensive Care 2005; 18 (4): 12–16.
White RD . Recommended standards for newborn ICU design. J Perinatol 2006; 26: S2–S18.
White RD . Recommended standards for the newborn ICU. J Perinatol 2007; 27: S4–S19.
Kruegar C, Wall S, Parker L, Nealis R . Elevated sound levels within a busy NICU. Neonatal Netw 2005; 24 (6): 33–37.
Gray L, Philbin MK . Effects of the neonatal intensive care unit on auditory attention and distraction. Clin Perinatol 2004; 31: 243–260.
Graven SN . Early neurosensory visual development of the fetus and newborn. Clini Perinatol 2004; 31: 199–216.
Rivkees SA . Emergence and influences of circadian rhythmicity in infants. Clin Perinatol 2004; 31: 217–228.
Miller CL, White R, Whitman TL, O’Callaghan MF, Maxwell SE . The effects of cycled versus noncycled lighting on growth and development in preterm infants. Infant Behav Dev 1995; 18: 87–95.
Gewolb DC, Vice FL . Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Dev Med Child Neurol 2006; 48 (7): 589–594.
Barlow SM . Oral and respiratory control for preterm feeding. Curr Opin Otolaryngol Head Neck Surg 2009; 17: 179–186.
Ferber SG, Makhoul IR . The effect of skin-to-skin contact (kangaroo care) shortly after birth on the neurobehavioral responses of the term newborn: a randomized, controlled trial. Pediatrics 2004; 113 (4): 858–865.
Saiman L . Risk factors for hospital-acquired infections in the neonatal intensive care unit. Semin Perinatol 2002; 26 (5): 315–321.
Adams-Chapman I, Stoll BJ . Prevention of nosocomial infections in the neonatal intensive care unit. Curr Opin Pediatr 2002; 14: 157–164.
Acknowledgements
We acknowledge the administration and NICU staff at the Cabell Huntington Hospital and Jeff Tyner, AIA at Perkins+Will for their support through the provision of resources and personnel essential for the completion of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Domanico, R., Davis, D., Coleman, F. et al. Documenting the NICU design dilemma: comparative patient progress in open-ward and single family room units. J Perinatol 31, 281–288 (2011). https://doi.org/10.1038/jp.2010.120
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.120
Keywords
This article is cited by
-
A unit’s experience with hybrid NICU design: description of care model and implications for patients, families, and professionals
Journal of Perinatology (2023)
-
Lärmbelastung einer neonatologischen Intensivstation
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie (2023)
-
Effects of single family room architecture on parent–infant closeness and family centered care in neonatal environments—a single-center pre–post study
Journal of Perinatology (2021)
-
The Effect of Single-Room Care Versus Open-Bay Care on the Incidence of Bacterial Nosocomial Infections in Pre-Term Neonates: A Retrospective Cohort Study
Infectious Diseases and Therapy (2021)
-
Qualitative analysis of latent safety threats uncovered by in situ simulation-based operations testing before moving into a single-family-room neonatal intensive care unit
Journal of Perinatology (2020)