Abstract
Objectives:
Previous studies have revealed that both short and long sleep durations are linked to obesity, hyperglycemia and hypertension. We evaluate the relationship between sleep duration and the metabolic syndrome using representative national survey data from the Korean population.
Methods:
We analyzed data from the 2001 Korean National Health and Nutrition Survey. The average amount of sleep per night was categorized as: ⩽5, 6, 7, 8 and ⩾9 h. Those reporting 7 h per night served as a reference group. In this cross-sectional study, the data of 4222 participants were finally analyzed.
Results:
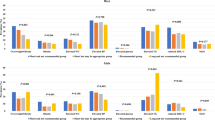
A majority of the components of the metabolic syndrome demonstrated U-shaped patterns based on sleep duration. Although the prevalences of abdominal obesity and hypertension were highest in subjects who slept ⩽5 h per night, those of hyperglycemia and high triglyceridemia were highest in subjects who slept ⩾9 h per night. Prevalence of the metabolic syndrome also exhibited U-shape pattern based on sleep duration. More components of the metabolic syndrome were highly associated with sleep duration in subjects under the age of 60 compared to those over the age of 60. Subjects who slept ⩽5 h per night demonstrated the highest risk for the metabolic syndrome (OR 1.74, 95% CI 1.33–2.26, P<0.001). Subjects who slept ⩾9 h per night exhibited increased risk for the metabolic syndrome even after adjustment of other risk variables (OR 1.69, 95% CI 1.17–2.45, P=0.006).
Conclusions:
Both short and long sleep durations are related to increased risk of the metabolic syndrome and its components in the Korean population, although adjustment for risk factors attenuates their relationship. Subjects reporting sleep duration of 7 h demonstrated the lowest prevalence of the metabolic syndrome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E . Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol 2005; 99: 2008–2019.
Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC . Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med 2005; 165: 25–30.
Kohatsu ND, Tsai R, Young T, Vangilder R, Burmeister LF, Stromquist AM et al. Sleep duration and body mass index in a rural population. Arch Intern Med 2006; 166: 1701–1705.
Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep 2004; 27: 661–666.
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 2003; 26: 380–384.
Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med 2005; 165: 863–867.
Gonzalez-Ortiz M, Martinez-Abundis E, Balcazar-Munoz BR, Pascoe-Gonzalez S . Effect of sleep deprivation on insulin sensitivity and cortisol concentration in healthy subjects. Diabetes Nutr Metab 2000; 13: 80–83.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006; 47: 833–839.
Tochikubo O, Ikeda A, Miyajima E, Ishii M . Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension 1996; 27: 1318–1324.
Lusardi P, Zoppi A, Preti P, Pesce RM, Piazza E, Fogari R . Effects of insufficient sleep on blood pressure in hypertensive patients: a 24-h study. Am J Hypertens 1999; 12: 63–68.
Bjorvatn B, Sagen IM, Oyane N, Waage S, Fetveit A, Pallesen S et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res 2007; 16: 66–76.
Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK et al. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care 2006; 29: 226–231.
Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens 2006; 24: 1515–1521.
Ministry of Health and Social Welfare. Analysis of Major Disease and Health Behavior in Koreans. Ministry of Health and Social Welfare: Gyeonggi-do, South Korea, 2003.
WHO. International Guide for Monitoring Alcohol Consumption and Related Harm. WHO: Geneva, 2000.
Ministry of Health and Social Welfare. Report on 1998 National Health and Nutrition Survey. Ministry of Health and Social Welfare: Gyeonggi-do, South Korea, 1999.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Grundy SM, Brewer Jr HB, Cleeman JI, Smith Jr SC, Lenfant C . Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433–438.
Health Communications Australia Pty Limit. The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Health Communications Australia Pty Limit: Sydney, Australia,, 2000.
Jean-Louis G, Kripke DF, Ancoli-Israel S . Sleep and quality of well-being. Sleep 2000; 23: 1115–1121.
National Sleep Foundation. National Sleep Foundation Sleep Survey. National Sleep Foundation: Washington, D.C., 2001.
Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I et al. Early life risk factors for obesity in childhood: cohort study. BMJ 2005; 330: 1357.
Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB . Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep 2005; 28: 1289–1296.
Taheri S, Lin L, Austin D, Young T, Mignot E . Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004; 1: e62.
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE et al. A prospective study of sleep duration and mortality risk in women. Sleep 2004; 27: 440–444.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB . Association between reduced sleep and weight gain in women. Am J Epidemiol 2006; 164: 947–954.
Spiegel K, Tasali E, Penev P, Van Cauter E . Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004; 141: 846–850.
Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med 2003; 163: 205–209.
Spiegel K, Leproult R, Van Cauter E . Impact of sleep debt on metabolic and endocrine function. Lancet 1999; 354: 1435–1439.
Kapas L, Hong L, Cady AB, Opp MR, Postlethwaite AE, Seyer JM et al. Somnogenic, pyrogenic, and anorectic activities of tumor necrosis factor-alpha and TNF-alpha fragments. Am J Physiol 1992; 263: R708–R715.
Hotamisligil GS, Shargill NS, Spiegelman BM . Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 1993; 259: 87–91.
Kario K, Schwartz JE, Pickering TG . Changes of nocturnal blood pressure dipping status in hypertensives by nighttime dosing of alpha-adrenergic blocker, doxazosin : results from the HALT study. Hypertension 2000; 35: 787–794.
van den Berg JF, Tulen JH, Neven AK, Hofman A, Miedema HM, Witteman JC et al. Sleep duration and hypertension are not associated in the elderly. Hypertension 2007; 50: 585–589.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Curr Opin Cardiol 2006; 21: 1–6.
Van Cauter E, Spiegel K . Sleep as a mediator of the relationship between socioeconomic status and health: a hypothesis. Ann N Y Acad Sci 1999; 896: 254–261.
Lockley SW, Skene DJ, Arendt J . Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res 1999; 8: 175–183.
Acknowledgements
We thank the members of the Korea Institute for Health and Social Affairs who conducted the national survey. This study was supported by a grant of the Seoul R&BD Program, Republic of Korea (10526).
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Choi, K., Lee, J., Park, H. et al. Relationship between sleep duration and the metabolic syndrome: Korean National Health and Nutrition Survey 2001. Int J Obes 32, 1091–1097 (2008). https://doi.org/10.1038/ijo.2008.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2008.62
Keywords
This article is cited by
-
Sleep characteristic profiles and the correlation with spectrum of metabolic syndrome among older adult: a cross-sectional study
BMC Geriatrics (2022)
-
Association of Sleep Duration with Obesity and Cardiometabolic Risk Factors in Children and Adolescents: A Population-Based Study
Scientific Reports (2019)
-
Associations of sleep durations and sleep-related parameters with metabolic syndrome among older Chinese adults
Endocrine (2019)
-
Association between sleep duration and metabolic syndrome: a cross-sectional study
BMC Public Health (2018)
-
Longer Sleep Duration and Later Sleep Timing are Associated with Increased Cold-Pain Perception During the Day
Sleep and Vigilance (2018)