Abstract
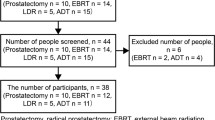
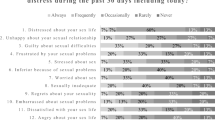
In an effort to address reports from men that their sex life is worse after treatment for rectal cancer, this qualitative study was designed to better understand their experience with sexual dysfunction following rectal cancer treatment, thus providing information on the adaptation of a psycho-educational sexual health intervention for male rectal cancer survivors and simultaneously investigating barriers and promoters that would influence their participation in a psycho-educational sexual health intervention. Thirteen male rectal cancer survivors who were treated at Memorial Sloan-Kettering Cancer Center (MSKCC) for rectal cancer participated (median time post-treatment was 6.4 years). Six survivors participated in individual semi-structured phone interviews, and seven others took part in focus groups. We performed standard procedures of qualitative thematic text analysis, which involved independent review of interview and focus group transcripts by several analysts followed by consensus meetings to identify key themes. Participants reported bowel dysfunction (N = 13, or 100 %) and erectile dysfunction (N = 12, or 92 %) as chief complaints. The participants thought a psychoeducational sexual health intervention post-surgery would be helpful because it would provide educational information regarding the etiology of their problems and treatments to improve their sexual health (N = 8, or 62 %). Most participants' primary concern immediately after treatment was surviving their disease; improving sexual functioning seemed to become more important over time. Barriers to potentially participating in a psycho-educational sexual health intervention included geographical distance from MSKCC (N = 3, or 3/13) and the risk of embarrassment when discussing sexual issues (N = 5, or 5/13). Men reported that a psycho-educational sexual health intervention would be helpful to improve their sexual functioning post-treatment. Discussion of bowel issues and logistical concerns gave information on the psycho-educational sexual health intervention.
Similar content being viewed by others
References
American Cancer Society Facts and Figures (2013) Cancers of the colon and rectum key statistics. Atlanta, GA, American Cancer Society
Ho VP, Lee Y, Stein SL, Temple LK (2011) Sexual function after treatment for rectal cancer: a review. Dis Colon Rectum 54:113–125
Potosky AL, Davis WW, Hoffman RM et al (2004) Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: the prostate cancer outcomes study. J Natl Cancer Inst 96:1358–1367
Hendren SK, O'Connor BI, Liu M et al (2005) Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg 242:212–223
Mannaerts G, Schijven MP, Hendrikx A, Martijn H, Rutten HJ, Wiggers T (2001) Urologic and sexual morbidity following multimodality treatment for locally advanced primary and locally recurrent rectal cancer. Eur J Surg Oncol 27:265–272
Moriya Y (2006) Function preservation in rectal cancer surgery. Int J Clin Oncol 11:339–343
Heriot AG, Tekkis PP, Fazio VW, Neary P, Lavery IC (2005) Adjuvant radiotherapy is associated with increased sexual dysfunction in male patients undergoing resection for rectal cancer: a predictive model. Ann Surg 242:502–510, discussion 10–1
Marijnen CA, van de Velde CJ, Putter H, van den Brink M, Maas CP, Martijn H, Rutten HJ, Wiggers T, Kranenbarg EK, Leer JW, Stiggelbout AM (2005) Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 23:1847–1858
Andersen BL, Cyranowski JM, Espindle D (1999) Men's sexual self-schema. J Pers Soc Psychol 76:645–661
Nelson CJ, Deveci S, Stasi J, Scardino PT, Mulhall JP (2010) Sexual bother following radical prostatectomy. J Sex Med 7:129–135
Nelson CJ, Mulhall JP, Roth AJ (2010) The association between erectile dysfunction and depressive symptoms in men treated for prostate cancer. J Sex Med 8:560-566
Canada AL, Neese LE, Sui D, Schover LR (2006) Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer 104:2689-2700
Schover LR, Fouladi RT, Warneke CL et al (2002) The use of treatments for erectile dysfunction among survivors of prostate carcinoma. Cancer 95:2397–2407
Sundaram CP, Thomas W, Pryor LE, Sidi AA, Billups K, Pryor JL (1997) Long-term follow-up of patients receiving injection therapy for erectile dysfunction. Urology 49:932–935
Guest G, Bunce A, Johnson L (2006) How many interviews are enough?: an experiment with data saturation and variability. Field Methods 18:59–82
Bernard HR (ed) (1994) Research methods in anthropology: qualitative and quantitative approaches. Sage Publications, Thousand Oaks
Creswell JW (ed) (1998) Qualitative inquiry and research design: choosing among five traditions. Sage Publications, Thousand Oaks
Green J, Thorogood N (eds) (2004) Qualitative methods for health research. Sage Publications, London
Patton MQ (ed) (2002) Qualitative evaluation and research methods. Sage Publications, Thousand Oaks
Miles MB, Huberman AM (eds) (1994) Qualitative data analysis, 2nd edn. Sage, Thousand Oaks
Patton MQ (1999) Enhancing the quality and credibility of qualitative analysis. Health Serv Res 34:1189–1208
Warren CAB, Karner TX (2005) Discovering qualitative methods: field research, interviews, and analysis. Roxbury Publishing Company, Los Angeles
Guba EG (1978) Toward a methodology of naturalistic inquiry in educational evaluation. Los Angeles: University of California, Graduate School of Education, Center for the Study of Evaluation
Hubbard G, Kidd L, Kearney N (2010) Disrupted lives and threats to identity: the experiences of people with colorectal cancer within the first year following diagnosis. Health (London) 14:131–146
List MA, Stracks J, Colangelo L et al (2000) How do head and neck cancer patients prioritize treatment outcomes before initiating treatment? J Clin Oncol 18:877–884
Arndt V, Merx H, Stegmaier C, Ziegler H, Brenner H (2004) Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: a population-based study. J Clin Oncol 22:4829–4836
Temple LK, Bacik J, Savatta SG et al (2005) The development of a validated instrument to evaluate bowel function after sphincter-preserving surgery for rectal cancer. Dis Colon Rectum 48:1353–1365
Araujo AB, Durante R, Feldman HA, Goldstein I, McKinlay JB (1998) The relationship between depressive symptoms and male erectile dysfunction: cross-sectional results from the Massachusetts Male Aging Study. Psychosom Med 60:458–465
Shabsigh R, Klein LT, Seidman S, Kaplan SA, Lehrhoff BJ, Ritter JS (1998) Increased incidence of depressive symptoms in men with erectile dysfunction. Urology 52:848–852
Shiri R, Koskimaki J, Tammela TL, Hakkinen J, Auvinen A, Hakama M (2007) Bidirectional relationship between depression and erectile dysfunction. J Urol 177:669–673
Smith DP, Supramaniam R, King MT, Ward J, Berry M, Armstrong BK (2007) Age, health, and education determine supportive care needs of men younger than 70 years with prostate cancer. J Clin Oncol 25:2560–2566
Steginga SK, Occhipinti S, Dunn J, Gardiner RA, Heathcote P, Yaxley J (2001) The supportive care needs of men with prostate cancer (2000). Psychooncology 10:66–75
O'Brien R, Rose P, Campbell C, et al (2010) "I wish I'd told them": a qualitative study examining the unmet psychosexual needs of prostate cancer patients during follow-up after treatment. Patient Educ Couns 84:200-207
Giesler RB, Given B, Given CW et al (2005) Improving the quality of life of patients with prostate carcinoma: a randomized trial testing the efficacy of a nurse-driven intervention. Cancer 104:752–762
Lepore SJ, Helgeson VS, Eton DT, Schulz R (2003) Improving quality of life in men with prostate cancer: a randomized controlled trial of group education interventions. Health Psychol 22:443–452
Penson DF, Latini DM, Lubeck DP, Wallace K, Henning JM, Lue T (2003) Is quality of life different for men with erectile dysfunction and prostate cancer compared to men with erectile dysfunction due to other causes? Results from the ExCEED data base. J Urol 169:1458–1461
Kerr J, Engel J, Schlesinger-Raab A, Sauer H, Holzel D (2003) Doctor-patient communication: results of a four-year prospective study in rectal cancer patients. Dis Colon Rectum 46:1038–1046
Razavi D, Delvaux N, Hopwood P (1997) Improving communication with cancer patients. A challenge for physicians. Ann N Y Acad Sci 809:350–360
Montorsi F, Guazzoni G, Strambi LF et al (1997) Recovery of spontaneous erectile function after nerve-sparing radical retropubic prostatectomy with and without early intracavernous injections of alprostadil: results of a prospective, randomized trial. J Urol 158:1408–1410
Acknowledgment
NIH (site grant number 1 R21 CA137434-01A1).
Conflict of interest
The authors have no conflicts to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ball, M., Nelson, C.J., Shuk, E. et al. Men’s Experience with Sexual Dysfunction Post-rectal Cancer Treatment: A Qualitative Study. J Canc Educ 28, 494–502 (2013). https://doi.org/10.1007/s13187-013-0492-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-013-0492-y