Abstract
Background
Fibromyalgia syndrome (FMS) is a disease of unknown pathogenesis characterized by chronic musculoskeletal pain. FMS has been also associated with altered endocrinological responses, but findings are inconsistent.
Purpose
The aim of the present study was to investigate free salivary cortisol levels in FMS patients compared with healthy controls with a particular focus on the cortisol awakening response (CAR). The saliva samples were collected in a controlled hospital-hotel setting, in which the participants’ compliance was high and a number of potential confounders were analyzed.
Method
Twenty-nine chronic female FMS patients and 29 age-matched healthy female controls were recruited. Salivary cortisol samples were investigated eight times: in the afternoon when participants arrived at the hospital, after stress provocation (to be reported separately), in the evening, before they went to sleep, upon awakening, 30 and 60 min later, and during the afternoon of the second day. Questionnaires measuring pain levels, sleeping problems, perceived stress, and personality were administered to the participants. Other psychophysiological measurements were used to assess sleep quality and heart rate.
Results
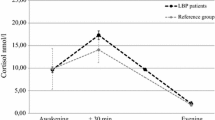
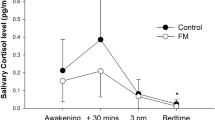
Patients with FMS had significantly lower cortisol levels during the day, most pronounced in the morning (CAR). The potential confounders analyzed did not influence the results. As expected, FMS patients reported more pain, stress, sleeping problems, anxiety, and depression.
Conclusion
The results lend support to the hypothesis of a dysfunction in the hypothalamus–pituitary–adrenal axis in FMS patients, with generally lower cortisol values, most pronounced upon awakening (CAR).




Similar content being viewed by others
References
Wolfe F, Smythe HA, Yunus MB, Bennet RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160–72.
Wolfe F, Ross K, Anderson J, Russell I, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28.
Wolfe F, Anderson J, Harkness D, Bennet R, Caro X, Goldenberg D, et al. Prospective, longitudinal, multicenter study of service utilization and costs in fibromyalgia. Arthritis Rheum. 1997;40:1560–70.
Krag N, Norregaard J, Larsen J, Danneskiold-Samsoe BA. Blinded controlled evaluation of anxiety and depressive symptoms in patients with fibromyalgia, as measured by standardized psychometric interview scales. Acta Psychiatr Scand. 1994;89:370–5.
Catley D, Kaell AT, Kirschbaum C, Stone AA. A naturalistic evaluation of cortisol secretion in persons with fibromyalgia and rheumatoid arthritis. Arthritis Care Res. 2000;13:51–61.
Crofford LJ, Pillemer SR, Kalogeras KT, Cash JM, Michelson D, Kling MA, et al. Hypothalamic–pituitary–adrenal axis perturbations in patients with fibromyalgia. Arthritis Rheum. 1994;37:1583–92.
Lentjes EG, Griep EN, Boersma JW, Romijn FP, de Kloet ER. Glucocorticoid receptors, fibromyalgia and low back pain. Psychoneuroendocrinology. 1997;22:603–14.
Klerman EB, Goldenberg DL, Brown EN, Maliszewski AM, Adler GK. Circadian rhythms of women with fibromyalgia. J Clin Endocrinol Metab. 2001;86:1034–9.
Crofford LJ, Young EA, Engleberg NC, Korszun A, Brucksch CB, McClure LA, et al. Basal circadian and pulsatile ACTH and cortisol secretion in patients with fibromyalgia and/or chronic fatigue syndrome. Brain Behav Immun. 2004;18:314–25.
Wingenfeld K, Wagner D, Schmidt I, Meinlschmidt G, Hellhammer DH, Heim C. The low-dose dexamethasone suppression test in fibromyalgia. J Psychosom Res. 2007;62:85–91.
Maes M, Lin A, Bonaccorso S, van Hunsel F, van Gastel A, Delmeire L, et al. Increased 24-hour urinary cortisol excretion in patients with post-traumatic stress disorder and patients with major depression, but not in patients with fibromyalgia. Acta Psychiatr Scand. 1998;98:328–35.
Adler GK, Kinsley BT, Hurwitz S, Mossey CJ, Goldenberg DL. Reduced hypothalamic–pituitary and sympathoadrenal responses to hypoglycemia in women with fibromyalgia syndrome. Am J Med. 1999;106:534–43.
McLean SA, Williams DA, Harris RE, Kop WJ, Groner KH, Ambrose K, et al. Momentary relationship between cortisol secretion and symptoms in patients with fibromyalgia. Arthritis Rheum. 2005;52:3660–9.
Macedo J, Hesse J, Turner J, Meyer J, Hellhammer D, Muller C. Glucocorticoid sensitivity in fibromyalgia patients: decreased expression of corticosteroid receptors and glucocorticoid-induced leucine zipper. Psychoneuroendocrinology. 2008;33:799–809.
Wingenfeld K, Heim C, Schmidt I, Wagner D, Meinlschmidt G, Hellhammer D. HPA axis reactivity and lymphocyte glucocorticoid sensitivity in fibromyalgia syndrome and chronic pelvic pain. Psychosom Med. 2008;70:65–72.
Griep E, Boersma J, de Kloet E. Altered reactivity of the hypothalamic-pituitary-adrenal axis in the primary fibromyalgia syndrome. J Rheumatol. 1993;20:469–74.
Griep EN, Boersma JW, Lentjes EG, Prins AP, van der Korst JK, de Kloet ER. Function of the hypothalamic–pituitary–adrenal axis in patients with fibromyalgia and low back pain. J Rheumatol. 1998;25:1374–81.
Loevinger B, Muller D, Alonso C, Coe C. Metabolic syndrome in women with chronic pain. Metabolism. 2007;56:87–93.
McCain GA, Tilbe KS. Diurnal hormone variation in fibromyalgia syndrome: a comparison with rheumatoid arthritis. J Rheumatol. 1989;16 Suppl 19:154–7.
van Denderen J, Boersma J, Zeinstra P, Hollander A, van Neerbos B. Physiological effects of exhaustive physical exercise in primary fibromyalgia syndrome (PFS): is PFS a disorder of neuroendocrine reactivity? Scand J Rheumatol. 1992;21:35–7.
Calis M, Gokce C, Ates F, Ulker S, Izgi HB, Demir H, et al. Investigation of the hypothalamo-pituitary-adrenal axis (HPA) by 1 microg ACTH test and metyrapone test in patients with primary fibromyalgia syndrome. J Endocrinol Invest. 2004;27:42–6.
Gur A, Cevik R, Sarac AJ, Colpan L, Em S. Hypothalamic-pituitary-gonadal axis and cortisol in young women with primary fibromyalgia: the potential roles of depression, fatigue, and sleep disturbance in the occurrence of hypocortisolism. Ann Rheum Dis. 2004;63:1504–6.
Gur A, Cevik R, Nas K, Colpan L, Sarac S. Cortisol and hypothalamic-pituitary-gonadal axis hormones in follicular-phase women with fibromyalgia and chronic fatigue syndrome and effect of depressive symptoms on the these hormones. Arthritis Res Ther. 2004;6:R232–8.
Chrousos GP, Gold PW. The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. JAMA. 1992;267:1244–52.
Sternberg EM. Hypoimmune fatigue syndromes: diseases of the stress response? J Rheumatol. 1993;20:418–21.
Crofford LJ, Demitrack MA. Evidence that abnormalities of central neurohormonal systems are key to understanding fibromyalgia and chronic fatigue syndrome. Rheum Dis Clin N Am. 1996;22:267–84.
Clauw DJ, Chrousos GP. Chronic pain and fatigue syndromes: overlapping clinical and neuroendocrine features and potential pathogenic mechanisms. Neuroimmunomodulation. 1997;4:134–53.
Fries E, Hesse J, Hellhammer J, Hellhammer DH. A new view on hypocortisolism. Psychoneuroendocrinology. 2005;30:1010–16.
Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25:1–35.
Weissbecker I, Floyd A, Dedert E, Salmon P, Sephton S. Childhood trauma and diurnal cortisol disruption in fibromyalgia syndrome. Psychoneuroendocrinology. 2006;31:312–24.
Pruessner J, Wolf O, Hellhammer D, Buske-Kirschbaum A, von Auer K, Jobst S, et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997;61:2539–49.
Williams E, Magid K, Steptoe A. The impact of time of waking and concurrent subjective stress on the cortisol response to awakening. Psychoneuroendocrinology. 2005;30:139–48.
Wilhelm I, Born J, Kudielka BM, Schlotz W, Wüst S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007;32:358–66.
Kudielka BM, Hellhammer DH, Wüst S. Why do we respond so differently? Reviewing determinants of human salivary cortisol responses to challenge. Psychoneuroendocrinology. 2009;34:2–18.
Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic–pituitary–adrenocortical axis in humans. Psychol Bull. 2007;133:25–45.
Kudielka BM, Bellingrath S, Hellhammer DH. Cortisol in burnout and vital exhaustion: an overview. G Ital Med Lav Ergon [Appl Psychol Work Rehabil Med]. 2006;28:34–42.
Boscarino JA. Posttraumatic stress disorder, exposure to combat, and lower plasma cortisol among Vietnam veterans: findings and clinical implications. J Consult Clin Psychol. 1996;64:191–201.
Wüst S, Wolf J, Hellhammer D, Federenko I, Schommer N, Kirschbaum C. The cortisol awakening response—normal values and confounds. Noise Health. 2000;7:77–85.
Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress. 2004;7:29–37.
Federenko I, Wüst S, Hellhammer DH, Dechoux R, Kumsta R, Kirschbaum C. Free cortisol awakening responses are influenced by awakening time. Psychoneuroendocrinology. 2004;29:174–84.
Borg G, Borg E. A new generation of scaling methods: level anchored ration scaling. Psychologia. 2001;28:15–45.
Eriksen H, Ihlebæk C, Ursin H. A scoring system for Subjective Health Complaints (SHC). Scand J Public Health. 1999;27:63–72.
Schalling D, Edman G. Personality and vulnerability to psychopathology: the development of the Karolinska Scales of Personality (KSP). Stockholm: Karolinska Institutet; 1987.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Eysenck H, Eysenck S. The manual for the Eysenck Personality Questionnaire. London: Hodder & Stoughton; 1975.
Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. 1st ed. Westchester: American Academy of Sleep Medicine; 2007.
Pruessner J, Kirschbaum C, Meinlschmid G, Hellhammer D. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–31.
Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 1999;61:197–204.
Roberts AD, Wessely S, Chalder T, Papadopoulos A, Cleare AJ. Salivary cortisol response to awakening in chronic fatigue syndrome. Br J Psychiatry. 2004;184:136–41.
Rohleder N, Joksimovic L, Wolf JM, Kirschbaum C. Hypocortisolism and increased glucocorticoid sensitivity of proinflammatory cytokine production in Bosnian war refugees with posttraumatic stress disorder. Biol Psychiatry. 2004;55:745–51.
Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry. 2004;56:651–6.
Wolf OT, Fujiwara E, Luwinski G, Kirschbaum C, Markowitsch HJ. No morning cortisol response in patients with severe global amnesia. Psychoneuroendocrinology. 2005;30:101–5.
Hellhammer J, Fries E, Schweisthal OW, Schlotz W, Stone AA, Hagemann D. Several daily measurements are necessary to reliably assess the cortisol rise after awakening: State- and trait components. Psychoneuroendocrinology. 2007;32:80–6.
Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol. 2009;80:265–78.
Van Houdenhove B, Van Den Eede F, Luyten P. Does hypothalamic-pituitary-adrenal axis hypofunction in chronic fatigue syndrome reflect a ‘crash’ in the stress system? Med hypothesis. 2009;72:701–5.
McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9.
Glass JM, Lyden AK, Petzke F, Stein P, Whalen G, Ambrose K, et al. The effect of brief exercise cessation on pain, fatigue, and mood symptom development in healthy, fit individuals. J Psychosom Res. 2004;57:391–8.
Shaver JL, Lentz M, Landis CA, Heitkemper MM, Buchwald DS, Woods NF. Sleep, psychological distress, and stress arousal in women with fibromyalgia. Res Nurs Health. 1997;20:247–57.
Ekstedt M, Åkerstedt T, Söderström M. Microarousals during sleep are associated with increased levels of lipids, cortisol, and blood pressure. Psychosom Med. 2004;66:925–31.
Vgontzas AN, Bixler EO, Lin HM, Prolo P, Mastorakos G, Vela-Bueno A, et al. Chronic insomnia is associated with nyctohemeral activation of thehypothalamic–pituitary–adrenal axis: clinical implications. J Clin Endocrinol Metab. 2001;86:3787–94.
Shaver J, Johnston S, Lentz M, Landis C. Stress exposure, psychological distress, and physiological stress activation in midlife women with insomnia. Psychosom Med. 2002;64:793–802.
Backhaus J, Junghanns K, Hohagen F. Sleep disturbances are correlated with decreased morning awakening salivary cortisol. Psychoneuroendocrinology. 2004;29:1184–91.
Vgontzas A, Mastorakos G, Bixler E, Kales A, Gold P, Chrousos GP. Sleep deprivation effects on the activity of the hypothalamic-pituitary-adrenal and growth axes: potential clinical implications. Clin Endocrinol (Oxf). 1999;51:205–15.
Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20:865–70.
Pasquali R, Vicennati V. The abdominal obesity phenotype and insulin resistance are associated with abnormalities of the hypothalamic-pituitaryadrenal axis in humans. Horm Metab Res. 2000;32:521–5.
Wallerius S, Rosmond R, Ljung T, Holm G, Bjorntorp P. Rise in morning saliva cortisol is associated with abdominal obesity in men: a preliminary report. J Endocrinol Invest. 2003;26:616–19.
Steptoe A, Kunz-Ebrecht SR, Brydon L, Wardle J. Central adiposity and cortisol responses to waking in middle-aged men and women. Int J Obes. 2004;28:1168–73.
Alen M, Pakarinen A, Häikkinen K, Komi P. Responses of serum androgenic-anabolic and catabolic hormones to prolonged strength training. Int J Sports Med. 1988;9:229–33.
Tabata I, Atomi Y, Mutoh Y, Miyashita M. Effect of physical training on responses of serum adrenocorticotropic hormone during prolonged exhausting exercise. Eur J Appl Physiol. 1990;61:188–92.
O’Connor P, Morgan W, Raglin J, Barksdale C, Kalin N. Mood state and salivary cortisol levels following overtraining in female swimmers. Psychoneuroendocrinology. 1989;14(4):303–10.
Filaire E, Duché P, Lac G, Robert A. Saliva cortisol, physical exercise and training: influences of swimming and handball on cortisol concentrations in women. Eur J Appl Physiol. 1996;74:274–8.
Bouget M, Rouveix M, Michaux O, Pequignot J, Filaire E. Relationships among training stress, mood and dehydroepiandrosterone sulphate/cortisol ratio in female cyclists. J Sports Sci. 2006;24(12):1297–302.
Kudielka BM, Broderick JE, Kirschbaum C. Compliance with saliva sampling protocols: electronic monitoring reveals invalid cortisol daytime profiles in noncompliant subjects. Psychosom Med. 2003;65:313–19.
Kudielka B, Kirschbaum C. Awakening cortisol responses are influenced by health status and awaking time but not by menstrual phase. Psychoneuroendocrinology. 2003;28:35–47.
Acknowledgments
This research was supported by grants to Professor Ulf Lundberg from the Swedish Research Council and the Swedish Council for Working Life and Social Research.
Thanks to Associate Professor Petra Lindfors for her suggestions regarding the statistical analysis and for her comments on the preliminary manuscript, Mrs. Ann-Christine Sjöbeck for performing the cortisol assays, Mr. Jens Nilsson for performing the sleep analysis, and to Mr. Håvard Wuttudal Lorås for assisting during data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Riva, R., Mork, P.J., Westgaard, R.H. et al. Fibromyalgia Syndrome is Associated with Hypocortisolism. Int.J. Behav. Med. 17, 223–233 (2010). https://doi.org/10.1007/s12529-010-9097-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-010-9097-6