Abstract
Background
Many pain patients appreciate biofeedback interventions because of the integration of psychological and physiological aspects. Therefore we wanted to investigate in a sample of chronic back pain patients whether biofeedback ingredients lead to improved outcome of psychological interventions.
Method
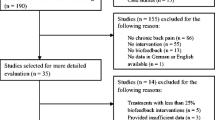
One hundred and twenty-eight chronic back pain patients were randomly assigned to cognitive-behavioural therapy (CBT), cognitive-behavioural therapy including biofeedback tools (CBT-B) or waitlist control (WLC). The sample was recruited from a highly disabled group including many patients with low education status and former back surgeries. Measures on pain, physical functioning, emotional functioning, coping strategies and health care utilisation were taken at pretreatment, posttreatment and 6 months of follow-up.
Results
The results indicated significant improvements on most outcome measures for CBT-B and CBT in comparison to WLC. CBT-B and CBT were equally effective (e.g. ITT effect sizes for pain intensity: CBT-B, 0.66 (95% CI 0.39–0.95); CBT, 0.60 (95% CI 0.33–0.87)).
Conclusion
In conclusion, biofeedback ingredients did not lead to improved outcome of a psychological intervention. Cognitive-behavioural treatment as a “package” of respondent, operant and cognitive interventions was effective for ameliorating pain-related symptoms for chronic back pain patients treated in an outpatient setting. The high treatment acceptability associated with biofeedback ingredients can also be achieved with pure psychological interventions.

Similar content being viewed by others
Notes
Please contact Dr. Julia A. Glombiewski (julia.glombiewski@staff.uni-marburg.de) for further information on treatment manual.
References
Schmidt CO, Raspe H, Pfingsten M, Hasenbring M, Basler HD, Eich W, et al. Back pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine. 2007;32:2005–11.
Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26:1–9.
van Tulder MW, Ostelo R, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane Back Review Group. Spine. 2001;26:270–81.
Nigl AJ. A comparison of binary and analog EMG feedback techniques in the treatment of low back pain. Am J Clin Biofeedback. 1981;4:25–31.
Flor H, Birbaumer N. Comparison of the efficacy of electromyographic biofeedback, cognitive-behavioral therapy, and conservative medical interventions in the treatment of chronic musculoskeletal pain. J Consult Clin Psychol. 1993;61:653–8.
Kroener-Herwig B, Beck A. An exploratory study of biofeedback for chronic low back pain. Br J Th Rehab. 2000;7:134–42.
Newton-John TR, Spence SH, Schotte D. Cognitive-behavioural therapy versus EMG biofeedback in the treatment of chronic low back pain. Behav Res Ther. 1995;33:691–7.
Hemingway MA, Biedermann HJ, Inglis J. Electromyographic recordings of paraspinal muscles: variations related to subcutaneous tissue thickness. Biofeedback Self Regul. 1995;20:39–49.
Keefe FJ, Shapira B. EMG-assisted relaxation training in the management of chronic low back pain. Am J Clin Biofeedback. 1981;4:93–103.
Nouwen A. EMG biofeedback used to reduce standing levels of paraspinal muscle tension in chronic low back pain. Pain. 1983;17:353–60.
Stuckey SJ, Jacobs A, Goldfarb J. EMG biofeedback training, relaxation training, and placebo for the relief of chronic back pain. Percept Mot Skills. 1986;63:1023–36.
Bush C, Ditto B, Feuerstein M. A controlled evaluation of paraspinal EMG biofeedback in the treatment of chronic low back pain. Health Psychol. 1985;4:307–21.
Large RG, Lamb AM. Electromyographic (EMG) feedback in chronic musculoskeletal pain: a controlled trial. Pain. 1983;17:167–77.
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19.
Yates SL, Morley S, Eccleston C, Williams ACD. A scale for rating the quality of psychological trials for pain. Pain. 2005;117:314–25.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates; 1988.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91.
Flor H, Turk DC. Psychophysiology of chronic pain: do chronic pain patients exhibit symptom-specific psychophysiological responses? Psychol Bullet. 1989;105:215–59.
Cram JR, Kasman GS, Holtz J. Introduction to surface electromyography. Gaithersburg: Aspen; 1998.
Nagel B, Gerbershagen HU, Lindena G, Pfingsten M. Entwicklung und empirische Uberprufung des Deutschen Schmerzfragebogens der DGSS. Schmerz. 2002;16:263–70.
Pollard CA. Preliminary validity study of the Pain Disability Index. Percept Mot Skills. 1986;59:974.
Tait RC, Chibnall JT, Krause S. The pain disability index: psychometric properties. Pain. 1990;40:171–82.
Myrtek M. Life satisfaction, illness behaviour, and rehabilitation outcome: results of a one year follow-up study with cardiac patients. Int J Rehabil Res. 1987;10:373–82.
Myrtek M, Fichtler A, Konig K, Brugner G, Muller W. Differences between patients with asymptomatic and symptomatic myocardial infarction: the relevance of psychological factors. Eur Heart J. 1994;15:311–7.
Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psych Rev. 1988;8:77–100.
Hautzinger M. Das Beck-Depressioninventar (BDI) in der Klinik The German version of the Beck Depression Inventory (BDI) in clinical use. Nervenarzt. 1991;62:689–96.
Lauridsen HH, Hartvigsen J, Korsholm L, Grunnet Nilsson N, Manniche C. Choice of external criteria in back pain research: Does it matter? Recommendations based on analysis of responsiveness. Pain. 2007;131:112–20.
Morley S, Williams A, Hussain S. Estimating the clinical effectiveness of cognitive behavioural therapy in the clinic: Evaluation of a CBT informed pain management programme. Pain. 2008;137:670–80.
Geissner E. Dimensionen der Verarbeitung chronischer Schmerzen-Eine Replikationsstudie. Z Klin Psychol Psychopathol Psychother. 1992;40:20–33.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58.
McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long standing chronic pain: a preliminary analysis of treatment outcome in comparison to a waiting phase. Behav Res Ther. 2005;43:1335–46.
van Tulder M, Koes B, Bombardier C. Low back pain. Clin Rheumatol. 2002;16:761–75.
Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–56.
Buchner M, Zahlten Hinguranage A, Schiltenwolf M, Neubauer E. Therapy outcome after multidisciplinary treatment for chronic neck and chronic low back pain: a prospective clinical study in 365 patients. Scand J Rheumatol. 2006;35:363–7.
Conflicts of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was supported by a doctoral thesis scholarship from the University of Marburg.
Rights and permissions
About this article
Cite this article
Glombiewski, J.A., Hartwich-Tersek, J. & Rief, W. Two Psychological Interventions Are Effective in Severely Disabled, Chronic Back Pain Patients: A Randomised Controlled Trial. Int.J. Behav. Med. 17, 97–107 (2010). https://doi.org/10.1007/s12529-009-9070-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-009-9070-4