Abstract
Background
Cerebral edema and raised intracranial pressure are common problems in neurological intensive care. Osmotherapy, typically using mannitol or hypertonic saline (HTS), has become one of the first-line interventions. However, the literature on the use of these agents is heterogeneous and lacking in class I studies. The authors hypothesized that clinical practice would reflect this heterogeneity with respect to choice of agent, dosing strategy, and methods for monitoring therapy.
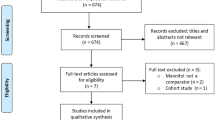
Methods
An on-line survey was administered by e-mail to members of the Neurocritical Care Society. Multiple-choice questions regarding use of mannitol and HTS were employed to gain insight into clinician practices.
Results
A total of 295 responses were received, 79.7% of which were from physicians. The majority (89.9%) reported using osmotherapy as needed for intracranial hypertension, though a minority reported initiating treatment prophylactically. Practitioners were fairly evenly split between those who preferred HTS (54.9%) and those who preferred mannitol (45.1%), with some respondents reserving HTS for patients with refractory intracranial hypertension. Respondents who preferred HTS were more likely to endorse prophylactic administration. Preferred dosing regimens for both agents varied considerably, as did monitoring parameters.
Conclusions
Treatment of cerebral edema using osmotically active substances varies considerably between practitioners. This variation could hamper efforts to design and implement multicenter trials in neurocritical care.

Similar content being viewed by others
References
Bhardwaj A. Osmotherapy in neurocritical care. Curr Neurol Neurosci Rep. 2007;7:513–21.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. II. Hyperosmolar therapy. J Neurotrauma. 2007;24(Suppl 1):S14–20.
Harold P, Adams J, Zoppo Gd, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke. Stroke. 2007;38:1655–711.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update. Stroke. 2007;38:2001–23.
Wise BL, Chater N. The value of hypertonic mannitol solution in decreasing brain mass and lowering cerebrospinal fluid pressure. J Neurosurg. 1962;19:1038–43.
Paczynski RP. Osmotherapy. Basic concepts and controversies. Crit Care Clin. 1997;13:105–29.
Francony G, Fauvage B, Falcon D, et al. Equimolar doses of mannitol and hypertonic saline in the treatment of increased intracranial pressure. Crit Care Med. 2008;36:795–800.
Lee SC, Chen JF, Lee ST. Continuous regional cerebral blood flow monitoring in the neurosurgical intensive care unit. J Clin Neurosci. 2005;12:520–3.
Hartmann A, Dettmers C, Schott H, Beyenburg S. Cerebral blood flow and rheologic alterations by hyperosmolar therapy in patients with brain edema. Acta Neurochir Suppl. (Wien). 1990;51:168–9.
Diringer MN, Zazulia AR. Osmotic therapy: fact and fiction. Neurocrit Care. 2004;1:219–33.
Rangel-Castillo L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 2008;26:521–41.
Kalita J, Misra UK, Ranjan P, Pradhan PK, Das BK. Effect of mannitol on regional cerebral blood flow in patients with intracerebral hemorrhage. J Neurol Sci. 2004;224:19–22.
Oddo M, Levine JM, Frangos S, et al. Effect of mannitol and hypertonic saline on cerebral oxygenation in patients with severe traumatic brain injury and refractory intracranial hypertension. J Neurol Neurosurg Psychiatry. 2009;80:916–20.
Sakowitz OW, Stover JF, Sarrafzadeh AS, Unterberg AW, Kiening KL. Effects of mannitol bolus administration on intracranial pressure, cerebral extracellular metabolites, and tissue oxygenation in severely head-injured patients. J Trauma. 2007;62:292–8.
Gasco J, Sendra J, Lim J, Ng I. Linear correlation between stable intracranial pressure decrease and regional cerebral oxygenation improvement following mannitol administration in severe acute head injury patients. Acta Neurochir Suppl. 2005;95:73–7.
Hartl R, Bardt TF, Kiening KL, Sarrafzadeh AS, Schneider GH, Unterberg AW. Mannitol decreases ICP but does not improve brain-tissue pO2 in severely head-injured patients with intracranial hypertension. Acta Neurochir Suppl. 1997;70:40–2.
Alvarez B, Ferrer-Sueta G, Radi R. Slowing of peroxynitrite decomposition in the presence of mannitol and ethanol. Free Radic Biol Med. 1998;24:1331–7.
Korenkov AI, Pahnke J, Frei K, et al. Treatment with nimodipine or mannitol reduces programmed cell death and infarct size following focal cerebral ischemia. Neurosurg Rev. 2000;23:145–50.
Wade CE, Grady JJ, Kramer GC, Younes RN, Gehlsen K, Holcroft JW. Individual patient cohort analysis of the efficacy of hypertonic saline/dextran in patients with traumatic brain injury and hypotension. J Trauma. 1997;42:S61–5.
Cooper DJ, Myles PS, McDermott FT, et al. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: a randomized controlled trial. JAMA. 2004;291:1350–7.
Ogden AT, Mayer SA, Sander Connolly E Jr. Hyperosmolar agents in neurosurgical practice: the evolving role of hypertonic saline. Neurosurgery. 2005;57:207–15.
Schwarz S, Georgiadis D, Aschoff A, Schwab S. Effects of hypertonic (10%) saline in patients with raised intracranial pressure after stroke. Stroke. 2002;33:136–40.
Schwarz S, Schwab S, Bertram M, Aschoff A, Hacke W. Effects of hypertonic saline hydroxyethyl starch solution and mannitol in patients with increased intracranial pressure after stroke. Stroke. 1998;29:1550–5.
Vialet R, Albanese J, Thomachot L, et al. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 ml/kg 7.5% saline is more effective than 2 ml/kg 20% mannitol. Crit Care Med. 2003;31:1683–7.
Ziai WC, Toung TJ, Bhardwaj A. Hypertonic saline: first-line therapy for cerebral edema? J Neurol Sci. 2007;261:157–66.
Mattox KL, Maningas PA, Moore EE, et al. Prehospital hypertonic saline/dextran infusion for post-traumatic hypotension. The U.S.A. Multicenter Trial. Ann Surg. 1991;213:482–91.
Shackford SR, Norton CH, Todd MM. Renal, cerebral, and pulmonary effects of hypertonic resuscitation in a porcine model of hemorrhagic shock. Surgery. 1988;104:553–60.
Rizoli SB, Rhind SG, Shek PN, et al. The immunomodulatory effects of hypertonic saline resuscitation in patients sustaining traumatic hemorrhagic shock: a randomized, controlled, double-blinded trial. Ann Surg. 2006;243:47–57.
Poli-de-Figueiredo LF, Cruz RJ Jr, Sannomiya P, Rocha ESM. Mechanisms of action of hypertonic saline resuscitation in severe sepsis and septic shock. Endocr Metab Immune Disord Drug Targets. 2006;6:201–6.
Sadick NS. Sclerotherapy of varicose and telangiectatic leg veins. Minimal sclerosant concentration of hypertonic saline and its relationship to vessel diameter. J Dermatol Surg Oncol. 1991;17:65–70.
Himmelseher S. Hypertonic saline solutions for treatment of intracranial hypertension. Curr Opin Anaesthesiol. 2007;20:414–26.
Froelich M, Ni Q, Wess C, Ougorets I, Hartl R. Continuous hypertonic saline therapy and the occurrence of complications in neurocritically ill patients. Crit Care Med. 2009;37:1433–41.
Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care. 2006;21:163–72.
Sankar T, Assina R, Karis JP, Theodore N, Preul MC. Neurosurgical implications of mannitol accumulation within a meningioma and its peritumoral region demonstrated by magnetic resonance spectroscopy: case report. J Neurosurg. 2008;108:1010–3.
Palma L, Bruni G, Fiaschi AI, Mariottini A. Passage of mannitol into the brain around gliomas: a potential cause of rebound phenomenon. A study on 21 patients. J Neurosurg Sci. 2006;50:63–6.
Maioriello AV, Chaljub G, Nauta HJ, Lacroix M. Chemical shift imaging of mannitol in acute cerebral ischemia Case report. J Neurosurg. 2002;97:687–91.
Qureshi AI, Suarez JI, Bhardwaj A. Malignant cerebral edema in patients with hypertensive intracerebral hemorrhage associated with hypertonic saline infusion: a rebound phenomenon? J Neurosurg Anesthesiol. 1998;10:188–92.
Soustiel JF, Mahamid E, Chistyakov A, Shik V, Benenson R, Zaaroor M. Comparison of moderate hyperventilation and mannitol for control of intracranial pressure control in patients with severe traumatic brain injury—a study of cerebral blood flow and metabolism. Acta Neurochir. (Wien). 2006;148:845–51. discussion 51.
Rozet I, Tontisirin N, Muangman S, et al. Effect of equiosmolar solutions of mannitol versus hypertonic saline on intraoperative brain relaxation and electrolyte balance. Anesthesiology. 2007;107:697–704.
Harutjunyan L, Holz C, Rieger A, Menzel M, Grond S, Soukup J. Efficiency of 7.2% hypertonic saline hydroxyethyl starch 200/0.5 versus mannitol 15% in the treatment of increased intracranial pressure in neurosurgical patients—a randomized clinical trial [ISRCTN62699180]. Crit Care. 2005;9:R530–40.
Battison C, Andrews PJ, Graham C, Petty T. Randomized, controlled trial on the effect of a 20% mannitol solution and a 7.5% saline/6% dextran solution on increased intracranial pressure after brain injury. Crit Care Med. 2005;33:196–202. discussion 57–8.
Cruz J, Minoja G, Okuchi K, Facco E. Successful use of the new high-dose mannitol treatment in patients with Glasgow Coma Scale scores of 3 and bilateral abnormal pupillary widening: a randomized trial. J Neurosurg. 2004;100:376–83.
Cruz J, Minoja G, Okuchi K. Major clinical and physiological benefits of early high doses of mannitol for intraparenchymal temporal lobe hemorrhages with abnormal pupillary widening: a randomized trial. Neurosurgery. 2002;51:628–37. discussion 37–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hays, A.N., Lazaridis, C., Neyens, R. et al. Osmotherapy: Use Among Neurointensivists. Neurocrit Care 14, 222–228 (2011). https://doi.org/10.1007/s12028-010-9477-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9477-4