Abstract
Purpose of Review
In this report, we review the need for point-of-care (POC) or near real-time testing for antiretrovirals, progress in the field, evidence for guiding implementation of these tests globally, and future directions in objective antiretroviral therapy (ART) or pre-exposure prophylaxis (PrEP) adherence monitoring.
Recent Findings
Two cornerstones to end the HIV/AIDS pandemic are ART, which provides individual clinical benefits and eliminates forward transmission, and PrEP, which prevents HIV acquisition with high effectiveness. Maximizing the individual and public health benefits of these powerful biomedical tools requires high and sustained antiretroviral adherence. Routine monitoring of medication adherence in individuals receiving ART and PrEP may be an important component in interpreting outcomes and supporting optimal adherence. Existing practices and subjective metrics for adherence monitoring are often inaccurate or unreliable and, therefore, are generally ineffective for improving adherence. Laboratory measures of antiretroviral concentrations using liquid chromatography tandem mass spectrometry have been utilized in research settings to assess medication adherence, although these are too costly and resource-intensive for routine use.
Summary
Newer, less costly technologies such as antibody-based methods can provide objective drug-level measurement and may allow for POC or near-patient adherence monitoring in clinical settings. When coupled with timely and targeted counseling, POC drug-level measures can support adherence clinic-based interventions to ART or PrEP in near real time.

Similar content being viewed by others
References
Joint United Nations Programme on HIV/AIDS (UNAIDS). Global Report 2019: Report on the global AIDS epidemic. Geneva; 2019.
Walmsley SL, Antela A, Clumeck N, Duiculescu D, Eberhard A, Gutieŕrez F, et al. Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection. N Engl J Med. 2013;369(19):1807–18.
Joint United Nations Programme on HIV/AIDS (UNAIDS). Understanding Fast-Track Targets: Accelerating Action to End the AIDS Epidemic by 2030. 2015 Available from: https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf
US Department of Health and Human Services (DHHS). What is ‘Ending the HIV Epidemic: A Plan for America’? [Internet]. HIV.gov. [cited 2019 Nov 7]. Available from: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview
Joint United Nations Programme on HIV/AIDS (UNAIDS). 90-90-90 An ambitious treatment target to help end the AIDS epidemic [Internet]. Geneva; 2014. Available from: http://unaids.org/sites/default/files/media_asset/90-90-90_en.pdf
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–9.
Brault MA, Spiegelman D, Hargreaves J, Nash D, Vermund SH. Treatment as prevention: concepts and challenges for reducing HIV incidence. J Acquir Immune Defic Syndr. 2019;82:S104–12.
Molina JM, Charreau I, Chidiac C, Pialoux G, Cua E, Delaugerre C, et al. Post-exposure prophylaxis with doxycycline to prevent sexually transmitted infections in men who have sex with men: an open-label randomised substudy of the ANRS IPERGAY trial. Lancet Infect Dis. 2018;18(3):308–17.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
World Health Organization (WHO). Policy brief: WHO expands recommendation on oral pre-exposure prophylaxis of HIV infection (PrEP) [Internet]. Geneva; 2015. Available from: http://apps.who.int/iris/bitstream/handle/10665/197906/WHO_HIV_2015.48_eng.pdf;jsessionid=FD090759CBB747974F6F77E7F020202D?sequence=1
Smith DK, Handel V, Wolitski M, Richard J, Stryker JE, Hall HI, et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition — United States, 2015. Morb Mortal Wkly Rep. 2015;64(46):1291–5.
Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;12(4):151.
Arnsten JH, Demas PA, Farzadegan H, Grant RW, Gourevitch MN, Chang C-J, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: comparison of self-report and electronic monitoring. Clin Infect Dis. 2001;33(8):1417–23.
Haberer JE, Musinguzi N, Boum Y, Siedner MJ, Mocello AR, Hunt PW, et al. Duration of antiretroviral therapy adherence interruption is associated with risk of virologic rebound as determined by real-time adherence monitoring in rural Uganda. J Acquir Immune Defic Syndr. 2015;70(4):386–92.
Bell KM, Haberer JE. Actionable adherence monitoring: technological methods to monitor and support adherence to antiretroviral therapy. Curr HIV/AIDS Rep. 2018;15(5):388–96.
Chaiyachati KH, Ogbuoji O, Price M, Suthar AB, Negussie EK, Bärnighausen T. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS. 2014;28(Suppl 2).
Fox MP, Rosen S. Retention of adult patients on antiretroviral therapy in low- and middle-income countries: systematic review and meta-analysis 2008-2013. J Acquir Immune Defic Syndr. 2015;69(1):98–108.
Stirratt MJ, Dunbar-Jacob J, Crane HM, Simoni JM, Czajkowski S, Hilliard ME, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470–82.
Pearson CR, Simoni JM, Hoff P, Kurth AE, Martin DP. Assessing antiretroviral adherence via electronic drug monitoring and self-report: an examination of key methodological issues. AIDS Behav. 2007;11(2):161–73.
Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45.
Castillo-Mancilla JR, Haberer JE. Adherence measurements in HIV: new advancements in pharmacologic methods and real-time monitoring. Curr HIV/AIDS Rep. 2018;15(1):49–59.
Orrell C, Cohen K, Leisegang R, Bangsberg DR, Wood R, Maartens G. Comparison of six methods to estimate adherence in an ART-naïve cohort in a resource-poor setting: which best predicts virological and resistance outcomes? AIDS Res Ther. 2017;14(1):20.
Walshe L, Saple DG, Mehta SH, Shah B, Bollinger RC, Gupta A. Physician estimate of antiretroviral adherence in India: poor correlation with patient self-report and viral load. AIDS Patient Care STDs. 2010;24(3):189–95.
Haberer JE, Robbins GK, Ybarra M, Monk A, Ragland K, Weiser SD, et al. Real-time electronic adherence monitoring is feasible, comparable to unannounced pill counts, and acceptable. AIDS Behav. 2012;16(2):375–82.
Agot K, Taylor D, Corneli AL, Wang M, Ambia J, Kashuba ADM, et al. Accuracy of self-report and pill-count measures of adherence in the FEM-PrEP clinical trial: implications for future HIV-prevention trials. AIDS Behav. 2015;19(5):743–51.
Saberi P, Chakravarty D, Ming K, Legnitto D, Gandhi M, Johnson MO, et al. Moving antiretroviral adherence assessments to the modern era: correlations among three novel measures of adherence. AIDS Behav. 2019;24(1):284–90.
Genn L, Chapman J, Okatch H, Abell N, Marukutira T, Tshume O, et al. Pharmacy refill data are poor predictors of virologic treatment outcomes in adolescents with HIV in Botswana. AIDS Behav. 2019;23(8):2130–7.
Acri T, TenHave TR, Chapman JC, Bogner HR, Gross R. Lack of association between retrospectively collected pharmacy refill data and electronic drug monitoring of antiretroviral adherence. AIDS Behav. 2010;14(4):748–54.
Grossberg R, Gross R. Use of pharmacy refill data as a measure of antiretroviral adherence. Curr HIV/AIDS Rep. 2007;4(4):187–91.
McMahon JH, Jordan MR, Kelley K, Bertagnolio S, Hong SY, Wanke CA, et al. Pharmacy adherence measures to assess adherence to antiretroviral therapy: review of the literature and implications for treatment monitoring. Clin Infect Dis. 2011;52(4):493–506.
Luma HN, Mbatchou Ngahane BH, Mapoure YN, Mengjo NB, Temfack E, Joko HA, et al. Cross-sectional assessment of three commonly used measures of adherence to combination antiviral therapy in a resource limited setting. Int J STD AIDS. 2015;28(1):69–76.
Kunutsor S, Walley J, Katabira E, Muchuro S, Balidawa H, Namagala E, et al. Clinic attendance for medication refills and medication adherence amongst an antiretroviral treatment cohort in Uganda: a prospective study. AIDS Res Treat. 2010;2010:872396.
Bastard M, Pinoges L, Balkan S, Szumilin E, Ferreyra C, Pujades-Rodriguez M. Timeliness of clinic attendance is a good predictor of virological response and resistance to antiretroviral drugs in HIV-infected patients. PLoS One. 2012;7(11):7.
Garrison LE, Haberer JE. Technological methods to measure adherence to antiretroviral therapy and preexposure prophylaxis. Curr Opin HIV AIDS. 2017;12(5):467–74.
World Health Organization (WHO), US President’s Emergency Plan for AIDS Relief (PEPFAR), Joint United Nations Programme on HIV/AIDS (UNAIDS). Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. Geneva; 2007.
Grimsrud A, Kaplan R, Bekker L-G, Myer L. Outcomes of a nurse-managed service for stable HIV-positive patients in a large South African public sector antiretroviral therapy programme. Tropical Med Int Health. 2014;19(9):1029–39.
Sanne I, Orrell C, Fox MP, Conradie F, Ive P, Zeinecker J, et al. Nurse versus doctor management of HIV-infected patients receiving antiretroviral therapy (CIPRA-SA): a randomised non-inferiority trial. Lancet. 2010;376(9734):33–40.
Sherr K, Pfeiffer J, Mussa A, Vio F, Gimbel S, Micek M, et al. The role of nonphysician clinicians in the rapid expansion of HIV care in Mozambique. J Acquir Immune Defic Syndr. 2009 Nov;52(Suppl 1):S20–3.
Brooks KM, Anderson PL. Pharmacologic-based methods of adherence assessment in HIV prevention. Clin Pharmacol Ther. 2018 Dec 1;104(6):1056–9.
Hendrix CW, Andrade A, Bumpus NN, Kashuba AD, Marzinke MA, Moore A, et al. Dose frequency ranging pharmacokinetic study of tenofovir-emtricitabine after directly observed dosing in healthy volunteers to establish adherence benchmarks (HPTN 066). AIDS Res Hum Retrovir. 2016 Jan;32(1):32–43.
Koenig H, Mounzer K, Daughtridge G, Sloan C, Lalley-Chareczko L, Moorthy G, et al. Urine assay for tenofovir to monitor adherence in real time to tenofovir disoproxil fumarate/emtricitabine as pre-exposure prophylaxis. HIV Med. 2017 Jul;18(6):412–8.
Drain PK, Kubiak RW, Siriprakaisil O, Klinbuayaem V, Quame-Amaglo J, Sukrakanchana P-O, et al. Urine Tenofovir concentrations correlate with plasma and relates to TDF adherence: a randomized directly-observed pharmacokinetic trial (TARGET study). Clin Infect Dis. 2019;69(9):1647.
Haaland RE, Martin A, Livermont T, Fountain J, Dinh C, Holder A, et al. Brief report: urine emtricitabine and tenofovir concentrations provide markers of recent antiretroviral drug exposure among HIV-negative men who have sex with men. J Acquir Immune Defic Syndr. 2019 Nov 1;82(3):252–6.
Fonsart J, Saragosti S, Taouk M, Peytavin G, Bushman L, Charreau I, et al. Single-dose pharmacokinetics and pharmacodynamics of oral tenofovir and emtricitabine in blood, saliva and rectal tissue: a sub-study of the ANRS IPERGAY trial. J Antimicrob Chemother. 2017;72(2):478–85.
Castillo-Mancilla JR, Bushman LR, Meditz A, Seifert SM, Zheng J-H, Guida LA, et al. Emtricitabine-triphosphate in dried blood spots (DBS) as a marker of recent dosing. In: Conference on Retroviruses and Opportunistic Infections. Seattle; 2015.
Seifert SM, Chen X, Meditz AL, Castillo-Mancilla JR, Gardner EM, Predhomme JA, et al. Intracellular tenofovir and emtricitabine anabolites in genital, rectal, and blood compartments from first dose to steady state. AIDS Res Hum Retrovir. 2016 Nov 1;32(10–11):981–91.
Podsadecki TJ, Vrijens BC, Tousset EP, Rode RA, Hanna GJ. “White coat compliance” limits the reliability of therapeutic drug monitoring in HIV-1-infected patients. HIV Clin Trials. 2008;9(4):238–46.
Donnell D, Baeten JM, Bumpus NN, Brantley J, Bangsberg DR, Haberer JE, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J Acquir Immune Defic Syndr. 2014 Jul 1;66(3):340–8.
Fonner VA, Dalglish SL, Kennedy CE, Baggaley R, O’Reilly KR, Koechlin FM, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS. 2016 Jul 31;30(12):1973–83.
Phillips TK, Sinxadi P, Abrams EJ, Zerbe A, Orrell C, Hu N-C, et al. A comparison of plasma efavirenz and tenofovir, dried blood spot tenofovir-diphosphate, and self-reported adherence to predict virologic suppression among South African women. J Acquir Immune Defic Syndr. 2019 Jul 1;81(3):311–8.
de Lastours V, Fonsart J, Burlacu R, Gourmel B, Molina J-M. Concentrations of tenofovir and emtricitabine in saliva: implications for preexposure prophylaxis of oral HIV acquisition. Antimicrob Agents Chemother. 2011 Oct;55(10):4905–7.
Krause J, Subklew-Sehume F, Kenyon C, Colebunders R. Acceptability of HIV self-testing: a systematic literature review. BMC Public Health. 2013 Dec 8;13(1):735.
Kowalczyk Mullins TL, Braverman PK, Dorn LD, Kollar LM, Kahn JA. Adolescent preferences for human immunodeficiency virus testing methods and impact of rapid tests on receipt of results. J Adolesc Health. 2010 Feb;46(2):162–8.
Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Damron KS, et al. Protocol for accuracy of point of care (POC) or in-office urine drug testing (immunoassay) in chronic pain patients: a prospective analysis of immunoassay and liquid chromatography tandem mass spectometry (LC/MS/MS). Pain Physician. 2010;13(1).
Yager J, Castillo-Mancilla JR, Ibrahim ME, Brooks KM, McHugh C, MaWhinney S, et al. Tenofovir-diphosphate in dried blood spots following escalating TAF/FTC dosing. In: Conference on Retroviruses and Opportunistic Infections. Seattle; 2019.
Zheng J-H, Rower C, McAllister K, Castillo-Mancilla J, Klein B, Meditz A, et al. Application of an intracellular assay for determination of tenofovir-diphosphate and emtricitabine-triphosphate from erythrocytes using dried blood spots. J Pharm Biomed Anal. 2016 Apr 15;122:16–20.
Liu AY, Yang Q, Huang Y, Bacchetti P, Anderson PL, Jin C, et al. Strong relationship between oral dose and tenofovir hair levels in a randomized trial: hair as a potential adherence measure for pre-exposure prophylaxis (PrEP). PLoS One. 2014 Jan 8;9(1):e83736.
Adams JL, Sykes C, Menezes P, Prince HMA, Patterson KB, Fransen K, et al. Tenofovir diphosphate and emtricitabine triphosphate concentrations in blood cells compared with isolated peripheral blood mononuclear cells: a new measure of antiretroviral adherence? J Acquir Immune Defic Syndr. 2013 Mar 1;62(3):260–6.
Castillo-Mancilla JR, Zheng J-H, Rower JE, Meditz A, Gardner EM, Predhomme J, et al. Tenofovir, emtricitabine, and tenofovir diphosphate in dried blood spots for determining recent and cumulative drug exposure. AIDS Res Hum Retrovir. 2013 Feb;29(2):384–90.
Anderson PL, Liu AY, Castillo-Mancilla JR, Gardner EM, Seifert SM, McHugh C, et al. Intracellular tenofovir-diphosphate and emtricitabine-triphosphate in dried blood spots following directly observed therapy. Antimicrob Agents Chemother. 2018;1(1):62.
Kearney BP, Flaherty JF, Shah J. Tenofovir disoproxil fumarate: clinical pharmacology and pharmacokinetics. Clin Pharmacokinet. 2004;43(9):595–612.
Koss CA, Bacchetti P, Hillier SL, Livant E, Horng H, Mgodi N, et al. Differences in cumulative exposure and adherence to tenofovir in the VOICE, iPrEx OLE, and PrEP demo studies as determined via hair concentrations. AIDS Res Hum Retrovir. 2017 Aug;33(8):778–83.
Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9.
Castillo-Mancilla JR, Morrow M, Coyle RP, Coleman SS, Gardner EM, Zheng J-H, et al. Tenofovir diphosphate in dried blood spots is strongly associated with viral suppression in individuals with human immunodeficiency virus infections. Clin Infect Dis. 2019 Apr 8;68(8):1335–42.
Morrow M, MaWhinney S, Coyle RP, Coleman SS, Gardner EM, Zheng J-H, et al. Predictive value of tenofovir diphosphate in dried blood spots for future viremia in persons living with HIV. J Infect Dis. 2019.
Koren G, Bellaish E, Maman K. Hair analysis for drug-facilitated crime: the critical role of hair growth rate. J Forensic Sci. 2019;64(5):1574–5.
Gandhi M, Glidden DV, Liu A, Anderson PL, Horng H, Defechereux P, et al. Strong correlation between concentrations of tenofovir (TFV) emtricitabine (FTC) in hair and TFV diphosphate and FTC triphosphate in dried blood spots in the iPrEx open label extension: implications for pre-exposure prophylaxis adherence monitoring. J Infect Dis. 2015 Nov 1;212(9):1402–6.
Gandhi M, Murnane PM, Bacchetti P, Elion R, Kolber MA, Cohen SE, et al. Hair levels of preexposure prophylaxis drugs measure adherence and are associated with renal decline among men/transwomen. AIDS. 2017 Oct 23;31(16):2245–51.
Thaden JT, Gandhi M, Okochi H, Hurt CB, McKellar MS. Seroconversion on preexposure prophylaxis: a case report with segmental hair analysis for timed adherence determination. AIDS. 2018;32(9):F1–4.
Gilliland WM, Prince HMA, Poliseno A, Kashuba ADM, Rosen EP. Infrared matrix-assisted laser desorption electrospray ionization mass spectrometry imaging of human hair to characterize longitudinal profiles of the antiretroviral maraviroc for adherence monitoring. Anal Chem. 2019;91(16):10816–22.
Cohen SE, Sachdev D, Lee SA, Scheer S, Bacon O, Chen MJ, et al. Acquisition of tenofovir-susceptible, emtricitabine-resistant HIV despite high adherence to daily pre-exposure prophylaxis: a case report. Lancet HIV. 2019;6(1):e43–50.
Gandhi M, Ameli N, Bacchetti P, Anastos K, Gange SJ, Minkoff H, et al. Atazanavir concentration in hair is the strongest predictor of outcomes on antiretroviral therapy. Clin Infect Dis. 2011 May;52(10):1267–75.
Tüdos AJ, Besselink GAJ, Schasfoort RBM. Trends in miniaturized total analysis systems for point-of-care testing in clinical chemistry. Lab Chip. 2001 Dec 1;1(2):83–95.
Pratt GW, Fan A, Melakeberhan B, Klapperich CM. A competitive lateral flow assay for the detection of tenofovir. Anal Chim Acta. 2018 Aug 9;1017:34–40.
Gandhi M, Bacchetti P, Rodrigues WC, Spinelli M, Koss CA, Drain PK, et al. Development and validation of an immunoassay for tenofovir in urine as a real-time metric of antiretroviral adherence. EClinicalMedicine. 2018;34(2):255–60.
Gandhi M, Wang G, King R, Rodrigues WC, Vincent M, Glidden DV, et al. Development and validation of the first point-of-care assay to objectively monitor adherence to HIV treatment and prevention in real-time in routine settings. AIDS. 2019;34(2):255–60.
Daughtridge G, Hebel S, Larabee L, Patani H, Cohen A, Fischl M, et al. Development and clinical use case of a urine tenofovir adherence test. In: HIV Diagnostics Conference. Atlanta; 2019.
Gandhi M, Bacchetti P, Spinelli MA, Okochi H, Baeten JM, Siriprakaisil O, et al. Brief report: validation of a urine tenofovir immunoassay for adherence monitoring to PrEP and ART and establishing the cutoff for a point-of-care test. J Acquir Immune Defic Syndr. 2019 May 1;81(1):72–7.
US Centers for Disease Control and Prevention (CDC). Screening in clinical settings | Screening for HIV [Internet]. 2019 [cited 2019 Dec 1]. Available from: https://www.cdc.gov/hiv/clinicians/screening/clinical-settings.html
World Health Organization (WHO). Consolidated guidelines on HIV testing services 2015 [Internet]. 2015 [cited 2019 Dec 1]. Available from: http://apps.who.int/iris/bitstream/10665/179870/1/9789241508926_eng.pdf?ua=1&ua=1
World Health Organization (WHO). WHO recommends HIV self-testing: Policy brief [Internet]. World Health Organization (WHO). Geneva: World Health Organization; 2016 [cited 2019 Jul 23]. Available from: https://www.who.int/hiv/pub/vct/who-recommends-hiv-self-testing/en/
ClinicalTrials.gov. Identifier NCT04341779, Simplifying treatment and monitoring for HIV. Bethesda: National Library of Medicine (US); 2020.
Bardon AR, Simoni JM, Layman LM, Stekler JD, Drain PK. Utility and acceptability of a point-of-care urine tenofovir test for adherence to HIV pre-exposure prophylaxis and antiretroviral therapy: a qualitative assessment among U.S. clients and providers. 2019;Manuscript.
Wu G, Zaman MH. Low-cost tools for diagnosing and monitoring HIV infection in low-resource settings. Bull World Health Organ. 2012 Dec;90(12):914–20.
Johnson CC, Kennedy C, Fonner V, Siegfried N, Figueroa C, Dalal S, et al. Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc. 2017;20(1).
Vojnov L, Markby J, Boeke C, Harris L, Ford N, Peter T. POC CD4 testing improves linkage to HIV care and timeliness of ART initiation in a public health approach: a systematic review and meta-analysis. Roques P, editor. PLoS One. 2016 May 13;11(5):e0155256.
Rice B, Boulle A, Schwarcz S, Shroufi A, Rutherford G, Hargreaves J. The continuing value of CD4 cell count monitoring for differential HIV care and surveillance. J Med Internet Res. 2019;1(3):21.
World Health Organization (WHO). Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy [Internet]. Geneva; 2017 [cited 2020 Jan 12]. Available from: https://www.who.int/hiv/pub/guidelines/advanced-HIV-disease/en/
Drain PK, Dorward J, Bender A, Lillis L, Marinucci F, Sacks J, et al. Point-of-care HIV viral load testing: an essential tool for a sustainable global HIV/AIDS response. Clin Microbiol Rev. 2019;19:32(3).
Agutu CA, Ngetsa CJ, Price MA, Rinke de Wit TF, Omosa-Manyonyi G, Sanders EJ, et al. Systematic review of the performance and clinical utility of point of care HIV-1 RNA testing for diagnosis and care. PLoS One. 2019;14(6).
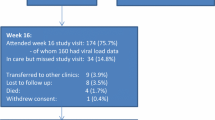
Drain PK, Dorward J, Violette LR, Quame-Amaglo J, Thomas KK, Samsunder N, et al. Point-of-care HIV viral load testing combined with task shifting to improve treatment outcomes: an open-label non-inferiority randomized controlled trial to Simplify HIV TREAtment and Monitoring (STREAM Study). Lancet HIV. 2020;In Press.
Nicholas S, Poulet E, Wolters L, Wapling J, Rakesh A, Amoros I, et al. Point-of-care viral load monitoring: outcomes from a decentralized HIV programme in Malawi. J Int AIDS Soc. 2019;22(8).
Estill J, Egger M, Blaser N, Vizcaya LS, Garone D, Wood R, et al. Cost-effectiveness of point-of-care viral load monitoring of antiretroviral therapy in resource-limited settings: mathematical modelling study. AIDS. 2013 Jun 1;27(9):1483–92.
de Necker M, de Beer JC, Stander MP, Connell CD, Mwai D. Economic and public health impact of decentralized HIV viral load testing: a modelling study in Kenya. PLoS One. 2019;1(2):14.
Simeon K, Sharma M, Dorward J, Naidoo J, Dlamini N, Moodley P, et al. Comparative cost analysis of point-of-care versus laboratory-based testing to initiate and monitor HIV treatment in South Africa. PLoS One. 2019;14(10).
Koester KA, Liu A, Eden C, Amico KR, McMahan V, Goicochea P, et al. Acceptability of drug detection monitoring among participants in an open-label pre-exposure prophylaxis study. AIDS Care. 2015 Oct 3;27(10):1199–204.
Montgomery ET, Mensch B, Musara P, Hartmann M, Woeber K, Etima J, et al. Misreporting of product adherence in the MTN-003/VOICE trial for HIV prevention in Africa: participants’ explanations for dishonesty. AIDS Behav. 2017;21(2):481–91.
Landovitz RJ, Beymer M, Kofron R, Amico KR, Psaros C, Bushman L, et al. Plasma tenofovir levels to support adherence to TDF/FTC preexposure prophylaxis for HIV prevention in MSM in Los Angeles, California. J Acquir Immune Defic Syndr [Internet]. 2017 [cited 2019 May 17];76(5):501–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28902074.
Celum C, Mgodi N, Bekker L-G, Hosek S, Donnell D, Anderson PL, et al. PrEP adherence and effect of drug level feedback among young African women in HPTN 082. In: International AIDS Society. Mexico City; 2019.
ClinicalTrials.gov. Identifier NCT03935464, Point-of-care Urine Monitoring of Adherence (PUMA): testing a real-time urine assay of tenofovir in PrEP (PUMA) [Internet]. Bethesda: National Library of Medicine (US); 2019. Available from: https://clinicaltrials.gov/ct2/show/NCT03935464
ClinicalTrials.gov. Identifer NCT04038060, The PrEP (Pre-exposure Prophylaxis) SMART study [Internet]. Bethesda: National Library of Medicine (US); 2019. Available from: https://clinicaltrials.gov/ct2/show/study/NCT04038060
Spreen WR, Margolis DA, Pottage JC. Long-acting injectable antiretrovirals for HIV treatment and prevention. Curr Opin HIV AIDS. 2013;8(6):565–71.
Devereaux ZJ, Reynolds CA, Fischer JL, Foley CD, DeLeeuw JL, Wager-Miller J, et al. Matrix-assisted ionization on a portable mass spectrometer: analysis directly from biological and synthetic materials. Anal Chem. 2016;88(22):10831–6.
Da Silva LC, Pereira I, De Carvalho TC, Allochio Filho JF, Romão W, Vaz BG. Paper spray ionization and portable mass spectrometers: a review. Anal Methods. 2019;11(8):999–1013.
Li L, Chen TC, Ren Y, Hendricks PI, Cooks RG, Ouyang Z. Mini 12, miniature mass spectrometer for clinical and other applications - Introduction and characterization. Anal Chem. 2014;86(6):2909–16.
Gao L, Sugiarto A, Harper JD, Cooks RG, Ouyang Z. Design and characterization of a multisource hand-held tandem mass spectrometer. Anal Chem. 2008 Oct 1;80(19):7198–205.
Jannetto PJ, Fitzgerald RL. Effective use of mass spectrometry in the clinical laboratory. Clin Chem. 2016 Jan 1;62(1):92–8.
Patel TS, Kaakeh R, Nagel JL, Newton DW, Stevenson JG. Cost analysis of implementing matrix- assisted laser desorption ionization-time of flight mass spectrometry plus real-time antimicrobial stewardship intervention for bloodstream infections. J Clin Microbiol. 2017;55(1):60–7.
Heaney LM, Jones DJ, Suzuki T. Mass spectrometry in medicine: a technology for the future? Futur Sci OA. 2017;3(3).
Pu F, Pandey S, Bushman LR, Anderson PL, Ouyang Z, Cooks RG. Direct quantitation of tenofovir diphosphate in human blood with mass spectrometry for adherence monitoring. Anal Bioanal Chem. 2020;
Ataullakhanov FI, Vitvitsky VM. What determines the intracellular ATP concentration. Biosci Rep. 2002;22(5–6):501–11.
Seok Y, Jang H, Oh J, Joung HA, Kim MG. A handheld lateral flow strip for rapid DNA extraction from staphylococcus aureus cell spiked in various samples. Biomed Phys Eng Express. 2019 Apr;17:5(3).
VanDine RW, Mahesh Babu U, Sambursky RP. US8614101B2 - in situ lysis of cells in lateral flow immunoassays [Internet]. US; 2009 [cited 2019 Dec 10]. Available from: https://patents.google.com/patent/US8614101B2/en
Castillo-Mancilla J, Seifert S, Campbell K, Coleman S, McAllister K, Zheng JH, et al. Emtricitabine-triphosphate in dried blood spots as a marker of recent dosing. Antimicrob Agents Chemother. 2016 Nov 1;60(11):6692–7.
Olanrewaju AO, Posner JD. An enzymatic assay to measure long-term adherence to pre-exposure prophylaxis and antiretroviral therapy. bioRxiv Bioeng.
Olanrewaju A, Sullivan B, Bender A, Zhang J, Lo T, Bardon A, et al. Development of an enzymatic assay for quantitative measurement of adherence to antiretroviral therapy and pre-exposure prophylaxis. In: The 14th International Conference on HIV Treatment and Prevention Adherence. Miami; 2019.
Ruane PJ, DeJesus E, Berger D, Markowitz M, Bredeek UF, Callebaut C, et al. Antiviral activity, safety, and pharmacokinetics/pharmacodynamics of tenofovir alafenamide as 10-day monotherapy in HIV-1-positive adults. J Acquir Immune Defic Syndr. 2013;63(4):449–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any data from studies with human or animal subjects that was performed by any of the authors and has not already been published elsewhere.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on The Science of Prevention
Rights and permissions
About this article
Cite this article
Drain, P.K., Bardon, A.R., Simoni, J.M. et al. Point-of-care and Near Real-time Testing for Antiretroviral Adherence Monitoring to HIV Treatment and Prevention. Curr HIV/AIDS Rep 17, 487–498 (2020). https://doi.org/10.1007/s11904-020-00512-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-020-00512-3