Abstract
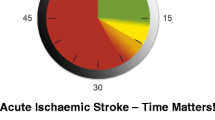
In acute ischemic stroke, time is brain. Current guidelines recommend that the time from arrival at hospital to initiation of administration of tissue plasminogen activator, also known as the door-to-needle (DTN) time, should be 60 min or less. However, DTN times in practice usually exceed this recommended time. The median DTN times from the American Heart Association/American Stroke Association Get With The Guidelines-Stroke program and the multinational Safe Implementation of Treatment in Stroke International Stroke Thrombolysis Register are 75 min and 65 min, respectively. Prehospital factors associated with delays include patient-related factors such as poor recognition of stroke symptoms, poor use of emergency medical services, and complex psychosocial factors. Accurate recognition of stroke symptoms at a dispatcher and paramedic level is associated with shorter onset-to-arrival times. Prenotification of regional stroke centers by paramedics is strongly associated with shorter DTN times. In-hospital delays resulting in prolonged DTN times can be attenuated by having well-defined rapid triage pathways, defined stroke teams, single-call stroke team activation, established code stroke protocols, rapid access to diagnostic imaging, and laboratory services. In this review we summarize factors associated with prolonged DTN times and processes that allow faster onset-to-treatment times. Recent developments in the field are highlighted.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263–6.
Vergouwen MD, Algra A, Pfefferkorn T, et al. Time is brain(stem) in basilar artery occlusion. Stroke. 2012;43(11):3003–6.
Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. New Engl J Med. 1995;333(24):1581–7.
Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012;379(9834):2364–72.
Lees KR, Bluhmki E, von Kummer R, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695–703.
•• Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in-hospital delay to 20 minutes in stroke thrombolysis. Neurology. 2012;79(4):306–13. This article demonstrates the value of using multiple concurrent strategies to reduce DTN times to 20 min.
Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;283(23):3102–9.
Adams Jr HP, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478–534.
Summers D, Leonard A, Wentworth D, et al. Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: a scientific statement from the American Heart Association. Stroke. 2009;40(8):2911–44.
•• Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association's Target: Stroke initiative. Stroke. 2011;42(10):2983–9. The AHA/ASA Target: Stroke initiative is a national quality improvement program designed to facilitate implementation of best practices for rapid, safe delivery of thrombolysis. This article outlines time-based tPA treatment related goals and suggests mechanisms to achieve them.
Smith EE, von Kummer R. Door-to-needle times in acute ischemic stroke: how low can we go? Neurology. 2012;79(4):296–7.
Ahmed N, Wahlgren N, Grond M, et al. Implementation and outcome of thrombolysis with alteplase 3–4.5 h after an acute stroke: an updated analysis from SITS-ISTR. Lancet Neurol. 2010;9(9):866–74.
•• Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123(7):750–8. This article examines the timeliness of tPA administration and factors that result in delay in the largest analysis of its kind of the GWTG-Stroke database. It demonstrates that only a minority of patients are treated within the prescribed 60-min window from arrival at hospital.
Messe SR, Fonarow GC, Smith EE, et al. Use of tissue-type plasminogen activator before and after publication of the European Cooperative Acute Stroke Study III in Get With The Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2012;5(3):321–6.
Nadeau JO, Shi S, Fang J, et al. TPA use for stroke in the Registry of the Canadian Stroke Network. Can J Neurol Sci. 2005;32(4):433–9.
Evenson KR, Foraker RE, Morris DL, Rosamond WD. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke. 2009;4(3):187–99.
Mackintosh JE, Murtagh MJ, Rodgers H, Thomson RG, Ford GA, White M. Why people do, or do not, immediately contact emergency medical services following the onset of acute stroke: qualitative interview study. PloS One. 2012;7(10):e46124.
• Lecouturier J, Murtagh MJ, Thomson RG, et al. Response to symptoms of stroke in the UK: a systematic review. BMC Health Serv Res. 2010;10:157. This article highlights patient factors resulting in OTA delays.
Salisbury HR, Banks BJ, Footitt DR, Winner SJ, Reynolds DJ. Delay in presentation of patients with acute stroke to hospital in Oxford. QJM. 1998;91(9):635–40.
Giles MF, Flossman E, Rothwell PM. Patient behavior immediately after transient ischemic attack according to clinical characteristics, perception of the event, and predicted risk of stroke. Stroke. 2006;37(5):1254–60.
Shah M, Makinde KA, Thomas P. Cognitive and behavioral aspects affecting early referral of acute stroke patients to hospital. J Stroke Cerebrovasc Dis. 2007;16(2):71–6.
Alberts MJ, Perry A, Dawson DV, Bertels C. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke. 1992;23(3):352–6.
Teuschl Y, Brainin M. Stroke education: discrepancies among factors influencing prehospital delay and stroke knowledge. Int J Stroke. 2010;5(3):187–208.
Dombrowski SU, Sniehotta FF, Mackintosh J, et al. Witness response at acute onset of stroke: a qualitative theory-guided study. PloS One. 2012;7(7):e39852.
Deakin CD, Alasaad M, King P, Thompson F. Is ambulance telephone triage using advanced medical priority dispatch protocols able to identify patients with acute stroke correctly? Emerg Med J. 2009;26(6):442–5.
Ramanujam P, Guluma KZ, Castillo EM, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics—San Diego experience. Prehosp Emerg Care. 2008;12(3):307–13.
Krebes S, Ebinger M, Baumann AM, et al. Development and validation of a dispatcher identification algorithm for stroke emergencies. Stroke. 2012;43(3):776–81.
Bray JE, Martin J, Cooper G, Barger B, Bernard S, Bladin C. An interventional study to improve paramedic diagnosis of stroke. Prehosp Emerg Care. 2005;9(3):297–302.
Govindarajan P, Ghilarducci D, McCulloch C, Pierog J, Bloom E, Johnston C. Comparative evaluation of stroke triage algorithms for emergency medical dispatchers (MeDS): prospective cohort study protocol. BMC Neurol. 2011;11:14.
Mosley I, Nicol M, Donnan G, Patrick I, Kerr F, Dewey H. The impact of ambulance practice on acute stroke care. Stroke. 2007;38(10):2765–70.
Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO). Stroke. 2005;36(7):1512–8.
Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000;31(1):71–6.
Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med. 1999;33(4):373–8.
Gladstone DJ, Rodan LH, Sahlas DJ, et al. A citywide prehospital protocol increases access to stroke thrombolysis in Toronto. Stroke. 2009;40(12):3841–4.
Schwamm LH, Pancioli A, Acker 3rd JE, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Circulation. 2005;111(8):1078–91.
•• Tong D, Reeves MJ, Hernandez AF, et al. Times from symptom onset to hospital arrival in the Get With The Guidelines–Stroke program 2002 to 2009: temporal trends and implications. Stroke. 2012;43(7):1912–7. This review of the GWTG-Stroke database outlines factors responsible for delays in onset-to-treatment times and highlights the lack of improvement in OTA times over the study period. Use of EMS, daytime stroke, and higher stroke severity result in shorter OTA times.
• Addo J, Ayis S, Leon J, Rudd AG, McKevitt C, Wolfe CD. Delay in presentation after an acute stroke in a multiethnic population in south London: the South London Stroke Register. J Am Heart Assoc. 2012;1(3):e001685. This article considers the factors related to OTA delays in a multiethnic European population.
Maestroni A, Mandelli C, Manganaro D, et al. Factors influencing delay in presentation for acute stroke in an emergency department in Milan. Italy Emerg Med J. 2008;25(6):340–5.
Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke. 2000;31(11):2585–90.
Wojner AW, Morgenstern L, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Paramedic and emergency department care of stroke: baseline data from a citywide performance improvement study. Am J Crit Care. 2003;12(5):411–7.
Kim SK, Lee SY, Bae HJ, et al. Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. Eur J Neurol. 2009;16(12):1331–5.
• Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5(4):514–22. This is one of several articles demonstrating the strong association between hospital prenotification by EMS and shorter DTN times.
•• McKinney JS, Mylavarapu K, Lane J, Roberts V, Ohman-Strickland P, Merlin MA. Hospital prenotification of stroke patients by emergency medical services improves stroke time targets. J Stroke Cerebrovasc Dis. 2013;22(2):113–8. This is one of several articles demonstrating the strong association between hospital prenotification by EMS and shorter DTN times.
Acker 3rd JE, Pancioli AM, Crocco TJ, et al. Implementation strategies for emergency medical services within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association Expert Panel on Emergency Medical Services Systems and the Stroke Council. Stroke. 2007;38(11):3097–115.
Crocco TJ, Grotta JC, Jauch EC, et al. EMS management of acute stroke–prehospital triage (resource document to NAEMSP position statement). Prehosp Emerg Care. 2007;11(3):313–7.
European Stroke Organisation Executive C, Committee ESOW. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25(5):457–507.
•• Lin CB, Peterson ED, Smith EE, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. J Am Heart Assoc. 2012;1(4):e002345. This is one of several articles demonstrating the strong association between hospital prenotification by EMS and shorter DTN times. In addition, the authors examine the factors related to prenotification by EMS in the large GWTG-Stroke database.
Albers GW, Bates VE, Clark WM, Bell R, Verro P, Hamilton SA. Intravenous tissue-type plasminogen activator for treatment of acute stroke: the Standard Treatment with Alteplase to Reverse Stroke (STARS) study. JAMA. 2000;283(9):1145–50.
Mikulik R, Kadlecova P, Czlonkowska A, et al. Factors influencing in-hospital delay in treatment with intravenous thrombolysis. Stroke. 2012;43(6):1578–83.
Saver JL, Smith EE, Fonarow GC, et al. The "golden hour" and acute brain ischemia: presenting features and lytic therapy in >30,000 patients arriving within 60 minutes of stroke onset. Stroke. 2010;41(7):1431–9.
Kohrmann M, Schellinger PD, Breuer L, et al. Avoiding in hospital delays and eliminating the three-hour effect in thrombolysis for stroke. Int J Stroke. 2011;6(6):493–7.
Belvis R, Cocho D, Marti-Fabregas J, et al. Benefits of a prehospital stroke code system. Feasibility and efficacy in the first year of clinical practice in Barcelona, Spain. Cerebrovasc Dis. 2005;19(2):96–101.
Hill MD, Buchan AM. Canadian Alteplase for Stroke Effectiveness Study I, Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ. 2005;172(10):1307–12.
de la Ossa NP, Sanchez-Ojanguren J, Palomeras E, et al. Influence of the stroke code activation source on the outcome of acute ischemic stroke patients. Neurology. 2008;70(15):1238–43.
Nazir FS, Petre I, Dewey HM. Introduction of an acute stroke team: an effective approach to hasten assessment and management of stroke in the emergency department. J Clin Neurosci. 2009;16(1):21–5.
Hamidon BB, Dewey HM. Impact of acute stroke team emergency calls on in-hospital delays in acute stroke care. J Clin Neurosci. 2007;14(9):831–4.
Tai YJ, Weir L, Hand P, Davis S, Yan B. Does a 'code stroke' rapid access protocol decrease door-to-needle time for thrombolysis? Intern Med J. 2012;42(12):1316–24.
Mehdiratta M, Woolfenden AR, Chapman KM, et al. Reduction in IV t-PA door to needle times using an Acute Stroke Triage Pathway. Can J Neurol Sci. 2006;33(2):214–6.
• Nolte CH, Malzahn U, Kuhnle Y, Ploner CJ, Muller-Nordhorn J, Mockel M. Improvement of door-to-imaging time in acute stroke patients by implementation of an all-points alarm. J Stroke Cerebrovasc Dis. 2013;22(2):149–53. This article demonstrates the utility of a single-call activation system in acute stroke.
•• Jauch EC, Saver JL, Adams Jr HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. This article provides comprehensive guidelines for management of AIS.
Sattin JA, Olson SE, Liu L, Raman R, Lyden PD. An expedited code stroke protocol is feasible and safe. Stroke. 2006;37(12):2935–9.
Green TL, Mansoor A, Newcommon N, Stephenson C, Stewart E, Hill MD. Reliability of point-of-care testing of INR in acute stroke. Can J Neurol Sci. 2008;35(3):348–51.
Rizos T, Jenetzky E, Herweh C, et al. Point-of-care reversal treatment in phenprocoumon-related intracerebral hemorrhage. Ann Neurol. 2010;67(6):788–93.
• Walter S, Kostopoulos P, Haass A, et al. Point-of-care laboratory halves door-to-therapy-decision time in acute stroke. Ann Neurol. 2011;69(3):581–6. Use of point-of-care INR testing when indicated can result in substantial reduction in DTN times as demonstrated in this article..
•• Kelly AG, Hellkamp AS, Olson D, Smith EE, Schwamm LH. Predictors of rapid brain imaging in acute stroke: analysis of the Get With the Guidelines-Stroke program. Stroke. 2012;43(5):1279–84. This is the largest study examining factors resulting in short DTI times in the national GWTG-Stroke database.
Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of time from hospital arrival to initial brain-imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke. 2008;39(12):3262–7.
•• Ford AL, Williams JA, Spencer M, et al. Reducing door-to-needle times using Toyota's lean manufacturing principles and value stream analysis. Stroke. 2012;43(12):3395–8. This single-center study demonstrates the usefulness of Toyota's lean manufacturing principles and value stream analysis in identifying institutional inefficiencies in the acute stroke treatment pathway.
Strbian D, Soinne L, Sairanen T, et al. Ultraearly thrombolysis in acute ischemic stroke is associated with better outcome and lower mortality. Stroke. 2010;41(4):712–6.
Wolfe F, Michaud K. The Hawthorne effect, sponsored trials, and the overestimation of treatment effectiveness. J Rheumatol. 2010;37(11):2216–20.
Qureshi AI, Suri MF, Nasar A, et al. Thrombolysis for ischemic stroke in the United States: data from National Hospital Discharge Survey 1999–2001. Neurosurgery. 2005;57(4):647–54. discussion 647–54.
Kleindorfer D, Lindsell CJ, Brass L, Koroshetz W, Broderick JP. National US estimates of recombinant tissue plasminogen activator use: ICD-9 codes substantially underestimate. Stroke. 2008;39(3):924–8.
Kostopoulos P, Walter S, Haass A, et al. Mobile stroke unit for diagnosis-based triage of persons with suspected stroke. Neurology. 2012;78(23):1849–52.
Liman TG, Winter B, Waldschmidt C, et al. Telestroke ambulances in prehospital stroke management: concept and pilot feasibility study. Stroke. 2012;43(8):2086–90.
•• Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol. 2012;11(5):397–404. This article, as well as [75••], represents a radical rethinking of how to achieve a significant reduction in DTN times by bringing tPA treatment by ambulance to the patient in the field, eliminating the time required for transportation to the emergency department.
•• Weber JE, Ebinger M, Rozanski M, et al. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurol. 2013;80(2):163–8. The authors demonstrate the efficacy and safety of point-of-emergency thrombolysis in the field, prior to transport to the emergency department.
Conflicts of Interest
Jamsheed A. Desai declares no conflicts of interest.
Eric E. Smith declares no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiovascular Disease and Stroke
Rights and permissions
About this article
Cite this article
Desai, J.A., Smith, E.E. Prenotification and Other Factors Involved in Rapid tPA Administration. Curr Atheroscler Rep 15, 337 (2013). https://doi.org/10.1007/s11883-013-0337-5
Published:
DOI: https://doi.org/10.1007/s11883-013-0337-5