Abstract
Background
Physician leadership development programs typically aim to strengthen physicians’ leadership competencies and improve organizational performance. We conducted a systematic review of medical literature on physician leadership development programs in order to characterize the setting, educational content, teaching methods, and learning outcomes achieved.
Methods
Articles were identified through a search in Ovid MEDLINE from 1950 through November 2013. We included articles that described programs designed to expose physicians to leadership concepts, outlined teaching methods, and reported evaluation outcomes. A thematic analysis was conducted using a structured data entry form with categories for setting/target group, educational content, format, type of evaluation and outcomes.
Results
We identified 45 studies that met eligibility criteria, of which 35 reported on programs exclusively targeting physicians. The majority of programs focused on skills training and technical and conceptual knowledge, while fewer programs focused on personal growth and awareness. Half of the studies used pre/post intervention designs, and four studies used a comparison group. Positive outcomes were reported in all studies, although the majority of studies relied on learner satisfaction scores and self-assessed knowledge or behavioral change. Only six studies documented favorable organizational outcomes, such as improvement in quality indicators for disease management. The leadership programs examined in these studies were characterized by the use of multiple learning methods, including lectures, seminars, group work, and action learning projects in multidisciplinary teams.
Discussion
Physician leadership development programs are associated with increased self-assessed knowledge and expertise; however, few studies have examined outcomes at a system level. Our synthesis of the literature suggests important gaps, including a lack of programs that integrate non-physician and physician professionals, limited use of more interactive learning and feedback to develop greater self-awareness, and an overly narrow focus on individual-level rather than system-level outcomes.
Similar content being viewed by others
INTRODUCTION
High-quality health care increasingly relies on teams, collaboration, and interdisciplinary work, and physician leadership is essential for optimizing health system performance.1 – 3 The Accreditation Council for Graduate Medical Education (ACGME) has established common program requirements that include skills in interpersonal communication, quality improvement, and system-based practice.4 The CanMEDS Physician Competency Framework identifies and describes seven roles for physicians: medical expert, communicator, collaborator, manager, health advocate, scholar, and professional.5 As practice management, performance improvement, and system-based practice have become integral to residency training in the U.S.6 – 8, experts are calling for leadership development to strengthen practicing physicians’ leadership skills and competencies.9 – 15 The lack of a common conceptual framework, however, presents a challenge to the field. While leadership may be understood as motivating and influencing others to bring about change, management involves achieving specific results through planning, organizing, and solving problems.16 Some see leadership and management as separate systems of action, but in practice, the terms are often used interchangeably.17 , 18 Some leadership models focus on competencies required to fill leadership roles in a given organizational setting, such as self-awareness, technical and conceptual knowledge, and skills needed in leadership roles.19 , 20
Although the literature draws a distinction between leader development (building individual competencies) and leadership development (building collective capacity)21, the term "leadership development" often encompasses efforts to develop individual leaders as well as to build capacity for leadership within an organization.22 , 23 Leadership development can promote several key functions in organizations, such as performance improvement, succession planning, and organizational change, and the literature on leadership provides evidence that leadership development helps organizations to achieve their goals.24 , 25 Developing leadership capacity in groups and organizations includes promoting a culture of accountability and alignment.22 , 26 Target groups for leadership development may include individuals with or without formal leadership roles.27 Leadership development programs may be delivered internally, externally, or a combination of both, and recent surveys suggest wide variation in approaches to leadership development among health care organizations.14 , 15
We lack a synthesis in the scientific literature that summarizes recurrent themes and empirical evidence regarding physician leadership development programs. Accordingly, we sought to systematically review published medical literature on physician leadership development in order to characterize the settings, educational content, teaching methods, and learning outcomes achieved. Findings from this study may be useful for designing and evaluating future leadership development programs.
METHODS
Literature Search
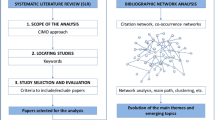
We searched for relevant English-language studies published from 1950 through November 2013 using the Ovid MEDLINE electronic database. We initially identified articles using text keyword searches (e.g. “leadership development”or “physicians”). We then developed a comprehensive search strategy using Medical Subject Headings terms: (Physicians OR Physician executives OR Internship and Residency OR Medical staff) AND (Leadership OR Practice Management) AND (Program evaluation OR Program development OR Curriculum). The search identified 596 unique articles, and four additional articles were identified through other sources, comprising a total of 600 articles (Fig. 1).
Eligibility Criteria
We included any peer-reviewed article that: (a) reported on an educational course, curriculum, or program designed to train physicians in leadership skills or expose physicians to leadership concepts, (b) outlined teaching methods used to achieve this goal, or (c) reported results from the evaluation of the course, curriculum, or program.
Article Review Process
Two members of the research team (J.F. and E.C.) independently reviewed all titles as well as available abstracts. Of the 600 articles, we excluded 527 that were not relevant, such as articles that focused exclusively on medical students or nurses or articles that described programs intended only to build competencies in quality improvement or accounting skills. The full text of the article was consulted as needed. We identified 73 articles that described leadership development courses or programs, and we were successful in retrieving the full text for a total of 71 articles. Two researchers (J.F. and A.B...) reviewed these articles to determine their eligibility; 26 articles did not report evaluation findings and were therefore excluded, resulting in a final sample of 45 studies.
The article screening process was followed by independent abstraction of data by J.F. and A.B. from all 45 articles, using a structured data entry form with categories for setting/target group, teaching/learning method used, educational content, evaluation design, method, and outcome. Differences in categorization at the article screening and data abstraction stages were resolved through negotiated consensus.
Data Analysis
We extracted curricular descriptors using the data entry form and recorded whether a curriculum was a one-time activity or an extended program, and to what extent didactic lectures/seminars, project work, group work, simulation, and multi-source/360-degree feedback tools were used. Leadership development may focus on personal growth, conceptual, or technical knowledge or skills19 , 20, and we recorded which of these aspects were covered by a program. Leadership development curricula may be evaluated using various outcome measures, including outcomes for individuals, groups or teams, organizations, networks, and societies.28 We used Kirkpatrick’s four-level evaluation model as a starting point for program classification.29 This model describes four evaluation levels: reaction (Level 1), knowledge (Level 2), behavioral change (Level 3), and system results (Level 4). In accordance with previous reviews on leadership development in the general leadership literature24 , 25 we differentiated between subjective and objective assessment of outcomes. Thus, seven categories were used to classify evaluation outcomes: reaction (Level 1), knowledge (subjective) (Level 2A), knowledge (objective) (Level 2B), behavior/expertise (subjective) (Level 3A), behavior/expertise (objective) (Level 3B), system results/performance (subjective) (Level 4A), and system results/performance (objective) (Level 4B) (Table 1).
RESULTS
Setting and Target Group
Of the 45 studies that met the eligibility criteria,30 – 74 the majority (n = 34) reported on single residency/fellowship programs or programs for physicians, surgeons, or medical faculty. A minority (n = 11) of programs were multidisciplinary (Table 2). Authors cited the need to foster a nonthreatening participatory and exploratory environment as the primary reason for including physicians only.58 , 71 The desire for interdisciplinary learning, communication, and collaboration were cited as reasons for choosing a multidisciplinary approach.40 , 50 , 56 Among the 45 articles, 39 reported on courses and programs in the U.S. and Canada (Table 3).
A total of 29 articles described programs for physicians (including residents and faculty) without a formal leadership role, and 16 articles described programs for individuals in formal leadership roles (chief residents, physicians with leadership responsibilities, program directors, and faculty in leadership position) (Table 3). The duration of training ranged from a half-day workshop47 to a three-year program.55 Most programs (n = 32) were delivered as an extended course, most often over a period of 12 months; fewer (n = 13) were one-time events (such as a single workshop, conference, or a course).
Educational Aims and Content
The educational programs in more than half of the 45 studies focused on training skills, including exercises on giving feedback, building teams, resolving conflicts, communicating and writing a business plan, or teaching technical and conceptual knowledge (Table 2). Personal growth and self-awareness were explicit aims in nine programs. The curricula addressed a wide range of educational content and displayed great diversity—and, at times, inconsistency—in concepts of leadership and management (see Tables 2 and 3). The most common topics included in the curricula were leadership, teamwork, financial management, self-management, conflict management, quality improvement, communication, and health policy/strategy.
Teaching/Learning Methods
Teaching methods were specified in 43 articles (Table 2), while two articles lacked this information.30 , 42 Of the 43 programs, 36 used didactic lectures/interactive plenary seminars, 32 involved group work (case-based discussions, exercises, group reflections), 16 included project work (action-based learning, project planning), and 12 reported the use of simulation exercises (simulated practice and role play). Multi-source feedback or a 360-degree feedback tool was used in three programs.33 , 54 , 64 Most of the programs used two or more teaching/learning methods in the curricula.
Evaluation Design and Outcomes
About half of the 45 studies used pre/post intervention designs as the basis for evaluating outcomes. Most post-intervention assessments occurred immediately after the program, while five studies assessed participants over a longer time span, of which three programs scored participants at baseline and at six months post-intervention,34 , 37 , 47 and three reported data on participant career development.40 , 42 , 64 Only five studies34 , 42 , 45 , 57 used a comparison group. Quantitative data only (surveys, tests, standardized observations, etc.) were used in the majority of studies, and qualitative data only (free-text comments, oral evaluation, and semi-structured interviews) were used in one study.35 Mixed evaluation methods were used in one-fifth of the studies.
A majority (n = 25) of the articles reported participants’ reaction scores (Level 1), and four-point or five-point Likert scales were commonly used to rate modules, sessions, or the program as a whole (Tables 2 and 3). Self-assessed knowledge outcomes (Level 2A) were reported in 36 of the studies, while objective tests of knowledge (Level 2B) were used alone or in addition to self-assessed measures in seven of the studies. Self-assessed learning outcomes for behavior/expertise (Level 3A) were reported in 10 studies. Two studies reported using objective outcome measures for behavior/expertise (Level 3B), such as using a form to score a third person’s leadership performance44 or using a checklist to score a team’s performance.47
Outcomes at the system (e.g., organizational) level (Level 4A and Level 4B) were reported in six articles. Staff-assessed increased quality of care was measured in one of these studies,37 and participant success in advancing to higher leadership roles was reported in three studies.42 , 54 , 64 Two of the studies documented objective outcomes on quality indicators for management of diseases such as diabetes, asthma, and breast cancer,48 and one study reported increased customer satisfaction.54 One study measured the number of business plans implemented.70
DISCUSSION
We identified 45 peer-reviewed articles that described and reported evaluation outcomes of physician leadership development programs. We found considerable heterogeneity concerning conceptual frameworks, teaching and learning methods, educational content, evaluation design, and outcomes measured. Most programs identified in this study targeted either resident physicians with no formal leadership roles or physicians in mid-level management positions. We found no reports on programs for physicians in top-level leadership positions. Almost two-thirds of the programs focused on skills training and technical and conceptual knowledge, while one-fifth of the programs focused on personal growth and awareness. All 45 studies reported positive outcomes, but few studies reported system-level effects, such as improved performance on quality indicators for disease management or increased customer satisfaction.
As a whole, the reports in the literature indicated that the majority of programs targeted physicians exclusively, with no participation of other professional groups within the health care organization. Although experts have noted that physician-only programs may facilitate open dialogue among participants75, it is possible that such approaches miss opportunities for developing the capacity to collaborate across professional lines, which may be important for team-based leadership.26 , 27 This review suggests that current approaches to physician leadership development focus more on the skills of individual physicians than on enhancing the capacity for collaboration through cultivating greater levels of understanding and communication networks across professional groups.
We also found that although self-awareness within larger groups and organizations is fundamental to leadership capacity, relatively few programs addressed personal growth and self-awareness.19 , 20 , 22 , 25 One-third of the programs addressed self-management, but the methods were limited, and few programs reported using any sort of multi-source feedback tool. Our findings suggest that the leadership programs described in the medical literature focus more on the “know” and “do” elements of leadership than the “be” component, which some argue is fundamental in attaining the capacity to lead.19 , 20 , 25 As teamwork and collaboration are increasingly required in the area of health care, there is a growing need to include self-awareness and emotional intelligence as fundamental competencies within leadership development programs.9 , 10 , 13 , 76
We found that programs largely employed lectures, seminars, and group work rather than the broader set of teaching tools available for leadership development, including developmental relationships (mentors, coaching, peer learning partners), assignments (job moves and rotations, action-based learning projects), feedback processes (performance appraisal, 360° feedback), and self-developmental activities.15 , 20 – 22 , 75 This finding is consistent with the recognition that, thus far, the literature on physician leadership development has been centered on imparting conceptual knowledge to physicians as individuals, for which lectures and seminars may be suitable, and has directed fewer resources to efforts in building self-awareness, for which action-based learning, feedback, and self-development activities may be more appropriate. Importantly, the few studies that documented favorable organizational outcomes, such as improvement in quality indicators for disease management, were characterized by the use of multiple learning methods, including lectures, seminars, and group work, and involved action learning projects in multidisciplinary teams.42 , 48 , 54 The implication of this finding is that greater investment in programs using teamwork and multiple learning methods is likely to have the largest impact in the area of leadership development for physicians. And while these may be more expensive and time-consuming to undertake, real progress will likely require such resources, and lower-level efforts may continue to have a limited effect.
Furthermore, we found that most of the literature evaluated the impact of programs on a narrow set of measures, most commonly participant satisfaction scores and self-assessed knowledge and behavioral change. Only six studies examined more complex outcomes at the system level. Evidence from outside the medical field has indicated that leadership development activities can positively influence organizational performance;24 , 25 however, the evidence base remains modest due to the paucity of studies that have assessed organization-level outcomes. Pilot programs are needed, with robust evaluation, to provide a base of evidence for the most effective means of achieving this critical capacity. We have come a long way in calling for great leadership among physicians, but there is opportunity for further improvement. Although learner satisfaction and individual learning outcomes are important, there is a dearth of research exploring clinical outcomes and organizational effects, as well as a lack of studies exploring the mechanisms by which leadership programs foster learning and change.
Our findings should be interpreted in light of several limitations. First, many of the studies we reviewed exhibited weak study design, modest and selected samples of participants, and a limited scope of outcomes measured. Furthermore, there was substantial heterogeneity among evaluation designs, outcome measures, and conceptual frameworks, precluding a quantitative synthesis of the varied findings. Although these are acknowledged limitations, this recognition also provides an understanding of the current state of evidence and highlights important paths for improvement with regard to studies on physician leadership development. Second, we limited our search to the peer-reviewed literature, excluding data on programs reported in the grey literature. Although this may have resulted in our missing novel programs, we wanted to ensure an adequate understanding of the methodologies employed, and thus focused on peer-reviewed scientific literature. Last, our findings likely suffer from publication bias, in that negative studies that have shown no significant impact of leadership development programs were likely underrepresented in our review. This is a common challenge for reviews of peer-reviewed literature, and is important to acknowledge in interpreting our findings.
In conclusion, the literature indicates that physician leadership development programs are associated with significantly increased self-assessed knowledge and expertise among physician participants; however, few studies have examined the impact on broader outcomes at an organizational or system level. Furthermore, our synthesis of the literature suggests important gaps, including a lack of programs that integrate non-physician and physician professionals, a limited use of more advanced training tools such as interactive learning and feedback in order to develop greater self-awareness, and an overly narrow focus on individual-level rather than system-level outcomes.
REFERENCES
Reinertsen JL. Physicians as leaders in the improvement of health care systems. Ann Intern Med. 1998;128:833–8.
McAlearney AS. Using leadership development programs to improve quality and efficiency in healthcare. J Healthc Manag. 2008;53:319–31.
Lee TH. Turning doctors into leaders. Harv Bus Rev. 2010;88(4):50–8.
The Accreditation Council for Graduate Medical Education. Common Program Requirements. Available at: http://www.acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx. Accessed 12 May 2014.
Frank JR, Danoff D. The CanMEDS initiative: implementing and outcomes-based framework for physician competencies. Med Teach. 2007;29:642–7.
Kolva DE, Barzee KA, Morley CP. Practice management curricula: a systematic literature review. Fam Med. 2009;41:411–9.
Wong BM, Etchells EE, Kuper A, Levinson W, Shojania KG. Teaching quality improvement and patient safety to trainees: a systematic review. Acad Med. 2010;85:1425–39.
Busari JO, Berkenbosh L, Brouns JW. Physicians as managers of health care delivery and the implications for postgraduate medical training: a literature review. Teach Lern Med. 2011;23:186–96.
Stoller JK. Developing physician-leaders: key competencies and available programs. J Health Adm Educ. 2008;25:307–28.
Stoller JK. Developing physician-leaders: a call to action. J Gen Intern Med. 2009;24:876–8.
Stoller JK. Recommendations and remaining questions for health care leadership training programs. Acad Med. 2013;88:12–5.
Blumenthal DM, Bernard K, Bohnen J, Bohmer R. Addressing the leadership gap in medicine: residents’ need for systematic leadership development training. Acad Med. 2012;87:513–22.
Detsky AS. How to be a good academic leader. J Gen Intern Med. 2010;26:88–90.
Anderson MM, Garman AN. Leadership development in healthcare systems: toward an evidence-based approach. Available at: http://nchl.org/Documents/Ctrl_Hyperlink/NCHL_Leadership_Survey_White_Paper_Final_05.14_uid6232014300422.pdf. Accessed 9 Jul 2014.
Physician leadership development programs: best practices in healthcare organizations. Available at: http://nchl.org/Documents/Ctrl_Hyperlink/NCHL_Physician_Leadership_Development_White_Paper_Final_05.14_uid6192014202392.pdf. Accessed 9 Jul 2014.
Yukl GA. Leadership in organizations. Englewood Cliffs, NJ: Prentice Hall; 2010.
Kotter JP. What leaders really do. Harv Bus Rev. 1990;63(3):103–11.
Mintzberg H. The nature of managerial work. New York, NY: Harper and Row; 1973.
Hesselbein F, Shinseki EK. Be, know, do: leadership the Army way. San Francisco, CA: Jossey-Bass; 2004.
Snook S, Nohria N, Khurana R, eds. The handbook for teaching leadership: knowing, doing, and being. London: Sage; 2012.
Day DV. Leadership development: a review in context. Leadersh Q. 2000;11:581–613.
Conger JA, Benjamin B. Building leaders: how successful companies develop the next generation. San Francisco, CA: Jossey-Bass; 1999.
Kets de Vries M, Korotov K. Introduction. In: Kets de Vries M, Korotov K, eds. Leadership development. Northhampton, MA: Edward Elgar Publishing; 2011:xv–xl.
Burke MJ, Day RR. A cumulative study of the effectiveness of managerial training. J Appl Psychol. 1986;71:232–45.
Collins DB, Holton EF III. The effectiveness of managerial leadership development programs: a metaanalysis of studies from 1982 to 2001. Hum Resour Dev Q. 2004;15:217–48.
Gronn P. Distributed leadership as a unit of analysis. Leadersh Q. 2002;13:423–51.
Fulop L, Day GE. From leader to leadership: clinician managers and where to next? Aust Health Rev. 2010;34:344–51.
Hannum KM, Martineau JW, Reinelt C, eds. The handbook of leadership development education. San Francisco, CA: Wiley; 2007.
Kirckpatrick DL. Techniques for evaluating training program. Train Dev J. 1979; 178–92.
Awad SS, Hayley B, Fagan SP, Berger DH, Brunicardi FC. The impact of a novel resident leadership training curriculum. Am J Surg. 2004;188:481–4.
Babitch LA. Teaching practice management skills to pediatric residents. Clin Pediatr (Phila). 2006;45:846–9.
Bayard M, Peeples CR, Holt J, David DJ. An interactive approach to teaching practice management to family practice residents. Fam Med. 2003;35:622–4.
Bearman M, O’Brien R, Anthony A, et al. Learning surgical communication, leadership and teamwork through simulation. J Surg Educ. 2012;69:201–7.
Bergman D, Fransson-Sellgren S, Wahlström R, et al. Healthcare leadership: impact of short-term intensive and long-term less intensive training programmes. Leadersh Health Serv. 2009;22:161–75.
Bircher J. Extending GP, training and the development of leadership skills: the experience of the North Western Deanery pilot. Educ Prim Care. 2013;24:57–60.
Block AA, Singh J, Kanaris AM, McGrath BP. Equipping our front-line managers: a national program for the Professional Development of Registrars. Med J Aust. 2007;186(7 Suppl):S22–4.
Boyle DK, Kochinda C. Enhancing collaborative communication of nurse and physician leadership in two intensive care units. J Nurs Adm. 2004;34:60–70.
Brandon CJ, Mullan PB. Teaching medical management and operations engineering for systems-based practice to radiology residents. Acad Radiol. 2013;20:345–50.
Cooper JB, Singer SJ, Hayes J, et al. Design and evaluation of simulation scenarios for a program introducing patient safety, teamwork, safety leadership, and simulation to healthcare leaders and managers. Sim Healthc. 2011;6:231–8.
Cordes DH, Rea DF, Rea J, Vuturo A. A program of management training for residents. Acad Med. 1989;64:45–6.
Crites GE, Schuster RJ. A preliminary report of an educational intervention in practice management. BMC Med Educ. 2004;4:15.
Dannels SA, Yamagata H, McDade SA, et al. Evaluating a leadership program: a comparative, longitudinal study to assess the impact of the Executive Leadership in Academic Medicine (ELAM) Program for Women. Acad Med. 2008;83:488–95.
Doughty RA, Williams PD, Seashore CN. Chief resident training. Developing leadership skills for future medical leaders. Am J Dis Child. 1991;145:639–42.
Edler A, Adamshick M, Fanning R, Piro N. Leadership lessons from military education for postgraduate medical curricular improvement. Clin Teach. 2010;7:26–31.
Evans DV, Egnew TR. Outdoor-based leadership training and group development of family practice interns. Fam Med. 1997;29:471–6.
Gagliano NJ, Ferris T, Colton D, Dubitzky A, Hefferman J, Torchiana D. A physician leadership development program at an academic medical center. Qual Manag Health Care. 2010;19:231–8.
Gilfoyle E, Gottesman R, Razack S. Development of a leadership skills workshop in paediatric advanced resuscitation. Med Teach. 2007;29:e276–83.
Green PL, Plsek PE. Coaching and leadership for the diffusion of innovation in health care: a different type of multi-organization improvement collaborative. Jt Comm J Qual Improv. 2002;28:55–71.
Gruver W, Spahr RC. Imparting wisdom to evolving leaders. New leadership program at Geisinger focuses on case-based discussions mixed with personal experience. Phys Exec. 2006;32(3):24–9.
Hanna WC, Mulder DS, Fried GM, Elhilali M, Khwaja KA. Training future surgeons for management roles: the resident-surgeon-manager conference. Arch Surg. 2012;147:940–4.
Hemmer PR, Karon BS, Hernandez JS, Cuthbert C, Fidler ME, Tazelaar HD. Leadership and management training for residents and fellows: a curriculum for future medical directors. Arch Pathol Lab Med. 2007;131:610–4.
Kasuya RT, Nip IL. A retreat on leadership skills for residents. Acad Med. 2001;76:554.
Kochar MS, Robertson RG, Mone MA. A faculty leadership development program at the Medical College of Wisconsin. WMJ. 2003;102:24–8.
Korschun HW, Redding D, Teal GL, Johns MM. Realizing the vision of leadership development in an academic health center: the Woodruff Leadership Academy. Acad Med. 2007;82:264–71.
Kuo AK, Thyne SM, Chen HC, West DC, Kamei RK. An innovative residency program designed to develop leaders to improve the health of children. Acad Med. 2010;85:1603–8.
Levine SA, Chao SH, Brett B, et al. Chief resident immersion training in the care of older adults: an innovative interspecialty education and leadership intervention. J Am Geriatr Soc. 2008;56:1140–5.
LoPresti L, Ginn P, Treat R. Using a simulated practice to improve practice management learning. Fam Med. 2009;41:640–5.
McAlearney AS, Fisher D, Heiser K, Robbins D, Kelleher K. Developing effective physician leaders: changing cultures and transforming organizations. Hosp Top. 2005;83(2):11–8.
Murdock J, Brammer C. A successful model of leadership development for community practice physicians. Phys Exec. 2011;37(2):52–4. 6.
Mygdal WK, Monteiro M, Hitchcock M, Featherston W, Conard S. Outcomes of the first Family Practice Chief Resident Leadership Conference. Fam Med. 1991;23:308–10.
O’Donnell L, Bennett GL. Case management takes lead role in educating medical residents. Prof Case Manag. 2011;16:253–5.
Patterson D, Godden A, Rughani A, Smithson WH. A leadership programme in GP training: an action learning approach. Educ Prim Care. 2013;24:65–8.
Pearson SD, Silverman TP, Epstein AL. Leadership and management training: a skill-oriented program for medical residents. J Gen Intern Med. 1994;9:227–31.
Pugno PA, Dornfest FD, Kahn NB Jr, Avant R. The National Institute for Program Director Development: a school for program directors. J Am Board Fam Pract. 2002;15:209–13.
Richman RC, Morahan PS, Cohen DW, McDade SA. Advancing women and closing the leadership gap: the Executive Leadership in Academic Medicine (ELAM) program experience. J Womens Health Gend Based Med. 2001;10:271–7.
Singer SJ, Hayes J, Cooper JB, et al. A case for safety leadership team training of hospital managers. Health Care Manag Rev. 2011;36:1–13.
Steinert Y, Nasmith L, Daigle N. Executive skills for medical faculty: a workshop description and evaluation. Med Teach. 2003;25:666–8.
Stergiopoulos V, Maggi J, Sockalingam S. Teaching the physician-manager role to psychiatric residents: development and implementation of a pilot curriculum. Acad Psychiatry. 2009;33:125–30.
Stoller JK, Rose M, Lee R, et al. Teambuilding and leadership training in an internal medicine residency program: experience with a one-day retreat. J Gen Intern Med. 2004;19:692–7.
Stoller JK, Berkowitz E, Bailin PL. Physician management and leadership education at the Cleveland Clinic Foundation: program impact and experience over 14 years. J Med Pract Manag. 2007;22:237–42.
Vimr M, Dickens P. Building physician capacity for transformational leadership–revisited. Healthc Manag Forum. 2013;26:16–9.
Weiss RL. A clinical laboratory management elective for pathology residents. Arch Pathol Lab Med. 1992;116:108–10.
Wisborg T, Brattebo G, Brattebo J, Brinchmann-Hansen A. Training multiprofessional trauma teams in Norwegian hospitals using simple and low cost local simulations. Educ Health. 2006;19:85–95.
Wurster AB, Pearson K, Sonnad SS, Mullen JL, Kaiser LR. The Patient Safety Leadership Academy at the University of Pennsylvania: the first cohort’s learning experience. Qual Manag Health Care. 2007;16:166–73.
McAlearney AS. Leadership development in healthcare: a qualitative study. J Organ Behav. 2006;27:967–82.
Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ. 2014;6:21–31.
Acknowledgments
Support for this research was provided by The Commonwealth Fund. The views presented here are those of the authors and should not be attributed to The Commonwealth Fund or its directors, officers, or staff.
Conflict of interest
The authors each declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Frich, J.C., Brewster, A.L., Cherlin, E.J. et al. Leadership Development Programs for Physicians: A Systematic Review. J GEN INTERN MED 30, 656–674 (2015). https://doi.org/10.1007/s11606-014-3141-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-3141-1