Abstract
Background
Despite growing emphasis on transitional care to reduce costs and improve quality, few studies have examined transitional care improvements in socioeconomically disadvantaged adults. It is important to consider these patients separately as many are high-utilizers, have different needs, and may have different responses to interventions.
Objective
To evaluate the impact of a multicomponent transitional care improvement program on 30-day readmissions, emergency department (ED) use, transitional care quality, and mortality.
Design
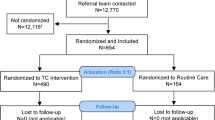
Clustered randomized controlled trial conducted at a single urban academic medical center in Portland, Oregon.
Participants
Three hundred eighty-two hospitalized low-income adults admitted to general medicine or cardiology who were uninsured or had public insurance.
Intervention
Multicomponent intervention including (1) transitional nurse coaching and education, including home visits for highest risk patients; (2) pharmacy care, including provision of 30 days of medications after discharge for those without prescription drug coverage; (3) post-hospital primary care linkages; (4) systems integration and continuous quality improvement.
Measurements
Primary outcomes included 30-day inpatient readmission and ED use. Readmission data were obtained using state-wide administrative data for all participants (insured and uninsured). Secondary outcomes included quality (3-item Care Transitions Measure) and mortality. Research staff administering questionnaires and assessing outcomes were blinded.
Results
There was no significant difference in 30-day readmission between C-TraIn (30/209, 14.4 %) and control patients (27/173, 16.1 %), p = 0.644, or in ED visits between C-TraIn (51/209, 24.4 %) and control (33/173, 19.6 %), p = 0.271. C-TraIn was associated with improved transitional care quality; 47.3 % (71/150) of C-TraIn patients reported a high quality transition compared to 30.3 % (36/119) control patients, odds ratio 2.17 (95 % CI 1.30–3.64). Zero C-TraIn patients died in the 30-day post-discharge period compared with five in the control group (unadjusted p = 0.02).
Conclusions
C-TraIn did not reduce 30-day inpatient readmissions or ED use; however, it improved transitional care quality.

Similar content being viewed by others
REFERENCES
Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: the care transitions measure. Med Care. 2005;43(3):246–255.
Rennke S, Nguyen OK, Shoeb MH, Magan Y, Wachter RM, Ranji SR. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):433–440.
Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549–555.
Englander H, Kansagara D. Planning and designing the care transitions innovation (C-train) for uninsured and medicaid patients. J Hosp Med. 2012;7(7):524–529.
Kangovi S, Barg FK, Carter T, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med. 2014;29(2):283–289.
Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. J Urban Health. 2009;86(2):230–241.
Kansagara D, Ramsay RS, Labby D, Saha S. Post-discharge intervention in vulnerable, chronically ill patients. J Hosp Med. 2012;7(2):124–130.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428.
US Congress. House Committee on Ways and Means, Committee on Energy and Commerce, Committee on Eduction and Labor. Compilation of Patient Protection and Affordable Care Act: as amended through 1 November 2010, including Patient Protection and Affordable Care Act health-related portions of the Health Care and Education Reconciliation Act of 2010. Washington, DC: US Government Printing Office; 2010:Xxii.
Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828.
Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187.
Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–684.
Davis MM, Devoe M, Kansagara D, Nicolaidis C, Englander H. “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
To access the appendix, click on the appendix link in the box to the right of the article online.
Oregon hospital discharge data set, owned by Oregon Health Authority and the Oregon Association of Hospitals & Health Systems. Accessed 5 Apr 2013.
Finkelstein A, Taubman S, Wright B, Bernstein M, Gruber J, Newhouse JP, Allen H, Baicker K, Oregon Health Study Group. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–1106.
OHSU EPIC Research data warehouse (RDW). Accessed 31 Jan 2012.
Oregon state vital records, Oregon health authority center for health statistics. Accessed 7 Feb 2013 via written request.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373-383.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251.
Health commons grant. http://www.healthcommonsgrant.org/.
Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–620.
Kangovi S, Mitra N, Grande D, White M, McCollum S, Sellman J, Shannon R, Long J. Patient-centered community HealthWorker intervention to improve posthospital outcomes. A randomized clinical trial. JAMA Intern Med. 2014;174:535–543. online first.
Joynt KE, Gawande AA, Orav EJ, Jha AK. Contribution of preventable acute care spending to total spending for high-cost medicare patients. JAMA. 2013;309(24):2572–2578.
van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402.
Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297–298.
Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587–593.
Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood). 2013;32(7):1196–1203.
Saha S, Solotaroff R, Oster A, Bindman AB. Are preventable hospitalizations sensitive to changes in access to primary care? The case of the Oregon health plan. Med Care. 2007;45(8):712–719.
Baicker K, Finkelstein A. The effects of Medicaid coverage–learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–685.
Kripalani S, Roumie CL, Dalal AK, Cawthon C, Businger A, Eden SK, Shintani A, Sponsler KC, Harris LJ, Theobald C, Huang RL, Scheurer D, Hunt S, Jacobson TA, Rask KJ, Vaccarino V, Gandhi TK, Bates DW, Williams MV, Schnipper JL. PILL-CVD (Pharmacist Intervention for Low Literacy in Cardiovascular Disease) Study Group. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med. 2012;157(1):1–10.
Kind AJ, Jensen L, Barczi S, et al. Low-cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at a VA hospital. Health Aff (Millwood). 2012;31(12):2659–2668.
Prieto-Centurion V, Markos MA, Ramey NI, Gussin HA, Nyenhuis SM, Joo MJ, Prasad B, Bracken N, Didomenico R, Godwin PO, Jaffe HA, Kalhan R, Pickard AS, Pittendrigh BR, Schatz B, Sullivan JL, Thomashow BM, Williams MV, Krishnan JA. Interventions to reduce rehospitalizations following chronic obstructive pulmonary disease exacerbations: a systematic review. Ann Am Thorac Soc. 2014;January.
ACKNOWLEDGMENTS
This work was funded by Oregon Health & Science University, which had no role in the study design or interpretation of results. Funding (Appendix D 15) included evaluation funds, salary for nurse and pharmacy care, and payment to community partners for primary care for uninsured patients who lacked a usual source of care.4
Dr. Kansagara is funded by the Department of Veterans Affairs. The findings and conclusions in this document are those of the author(s) who are responsible for its contents; the findings and conclusions do not necessarily represent the views of the Department of Veterans Affairs or the US government. Therefore, no statement in this article should be construed as an official position of the Department of Veterans Affairs.
Results described in this manuscript were presented at the Northwest Regional SGIM meeting in February 2013.
The authors would like to thank members of the C-TraIn Implementation and Research Team who contributed to the work described in this manuscript, including:
• Transitional Care Nurses: Stephanie Peña, Stacey Moultrie
• Pharmacy: Jackie Sharpe, Julie Kidd, Katie Foster, Daniel Kennedy
• Outpatient clinics: Kristy Butler, Lorri Aldridge, Paige Perry, Katie Bensching, Nic Granum, Carol Weber, Amanda Luocks, Billie Kay Stafford, Sandy Anderson, Rachel Solotaroff, Glory Coates, Ivan Wong, Ann Turner
• Clinical Informatics: Anita Murrin
• Hospital Administration: Char Riley, Peter Rapp, Marcha Hunt, Debbie Lamberger, Mayla Gant, Kippi Coffey, Desember Brucker, Jennifer Norquist
• Research Staff and Support: Chad Johnson, Chris Toomey, Christiane Winters, Katelynne Gardner, Sherry Kim, Russell Voth
• Advisors: Cynthia Morris, K. John McConnell, Christina Nicolaidis
Conflict of Interest
The authors declare that they do not have a conflict of interest.
IRB Approval
This study was approved by OHSU’s IRB (eIRB 6208). The full protocol can be accessed upon request to: Honora Englander, MD, englandh@ohsu.edu
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical Trials: This manuscript was registered with clinical trials.gov (NCT01906645)
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 87.0 KB)
Rights and permissions
About this article
Cite this article
Englander, H., Michaels, L., Chan, B. et al. The Care Transitions Innovation (C-TraIn) for Socioeconomically Disadvantaged Adults: Results of a Cluster Randomized Controlled Trial. J GEN INTERN MED 29, 1460–1467 (2014). https://doi.org/10.1007/s11606-014-2903-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2903-0