ABSTRACT
BACKGROUND
While there has been extensive research into patient-specific predictors of medication adherence and patient-specific interventions to improve adherence, there has been little examination of variation in clinic-level medication adherence.
OBJECTIVE
We examined the clinic-level variation of oral hypoglycemic agent (OHA) medication adherence among patients with diabetes treated in the Department of Veterans Affairs (VA) primary care clinics. We hypothesized that there would be systematic variation in clinic-level adherence measures, and that adherence within organizationally-affiliated clinics, such as those sharing local management and support, would be more highly correlated than adherence between unaffiliated clinics.
DESIGN
Retrospective cohort study.
SETTING
VA hospital and VA community-based primary care clinics in the contiguous 48 states.
PATIENTS
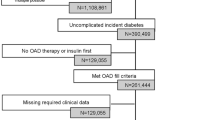
444,418 patients with diabetes treated with OHAs and seen in 158 hospital-based clinics and 401 affiliated community primary care clinics during fiscal years 2006 and 2007.
MAIN MEASURES
Refill-based medication adherence to OHA.
KEY RESULTS
Adjusting for patient characteristics, the proportion of patients adherent to OHAs ranged from 57 % to 81 % across clinics. Adherence between organizationally affiliated clinics was high (Pearson Correlation = 0.82), and adherence between unaffiliated clinics was low (Pearson Correlation = 0.04).
CONCLUSION
The proportion of patients adherent to OHAs varied widely across VA primary care clinics. Clinic-level adherence was highly correlated to other clinics in the same organizational unit. Further research should identify which factors common to affiliated clinics influence medication adherence.




Similar content being viewed by others
REFERENCES
Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–24.
Choudhry NK, Avorn J, Glynn RJ, et al. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365(22):2088–97.
Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonald HP. Interventions to enhance medication adherence. Cochrane Database Syst Rev. 2005(4):CD000011.
http://www.va.gov/primarycare/pcmh/. Accessed 12/24/12
Chapko MK, Borowsky SJ, Fortney JC, et al. Evaluation of the Department of Veterans Affairs community-based outpatient clinics. Med Care. 2002;40(7):555–60.
Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med. 2003;18(8):624–33.
Piette JD, Bibbins-Domingo K, Schillinger D. Health care discrimination, processes of care, and diabetes patients’ health status. Patient Educ Couns. 2006;60(1):41–8.
Piette JD, Heisler M, Horne R, Caleb AG. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med. 2006;62(4):846–57.
Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med. 2010;153(8):507–15.
Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(Suppl 2):B10–21.
Wong ES, Piette JD, Liu CF, et al. Measures of adherence to oral hypoglycemic agents at the primary care clinic level: the role of risk adjustment. Med Care. 2012;50(7):591–8.
Bryson CL, Au DH, Young B, McDonell MB, Fihn SD. A refill adherence algorithm for multiple short intervals to estimate refill compliance (ReComp). Med Care. 2007;45:497–504.
Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;50(1):105–16.
Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15(8):565–74.
Cohen HW, Shmukler C, Ullman R, Rivera CM, Walker EA. Measurements of medication adherence in diabetic patients with poorly controlled HbA(1c). Diabet Med. 2010;27(2):210–6.
Hansen RA, Kim MM, Song L, Tu W, Wu J, Murray MD. Comparison of methods to assess medication adherence and classify nonadherence. Ann Pharmacother. 2009;43(3):413–22.
Efron BT. R. bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci. 1986;1(1):54–75.
Crawford SL. Correlation and regression. Circulation. 2006;114(19):2083–8.
Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–60.
Vermeire E, Wens J, Van Royen P, Biot Y, Hearnshaw H, Lindenmeyer A. Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;(2):CD003638.
Rose AJ, Hylek EM, Ozonoff A, Ash AS, Reisman JI, Berlowitz DR. Risk-adjusted percent time in therapeutic range as a quality indicator for outpatient oral anticoagulation: results of the Veterans Affairs Study to Improve Anticoagulation (VARIA). Circ Cardiovasc Qual Outcomes. 2011;4(1):22–9.
Krumholz HM, Curry LA, Bradley EH. Survival after acute myocardial infarction (SAMI) study: the design and implementation of a positive deviance study. Am Heart J. 2011;162(6):981–7. e989.
Anderson MA, Helms LB. Comparison of continuing care communication. Image J Nurs Sch. 1998;30(3):255–60.
Risser DT, Rice MM, Salisbury ML, Simon R, Jay GD, Berns SD. The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium. Ann Emerg Med. 1999;34(3):373–83.
Weiner BJ, Shortell SM, Alexander J. Promoting clinical involvement in hospital quality improvement efforts: the effects of top management, board, and physician leadership. Health Serv Res. 1997;32(4):491–510.
Lammers JC, Cretin S, Gilman S, Calingo E. Total quality management in hospitals: the contributions of commitment, quality councils, teams, budgets, and training to perceived improvement at Veterans Health Administration hospitals. Med Care. 1996;34(5):463–78.
Jackson D, White I, Kostis JB, et al. Systematically missing confounders in individual participant data meta-analysis of observational cohort studies. Stat Med. 2009;28(8):1218–37.
Blundell R, Windmeijer F. Identifying demand for health resources using waiting times information. Health Econ. 2000;9(6):465–74.
Acknowledgements
This research was supported by an Investigator Initiated Research Award (IIR 07-068-2) from the Department of Veterans Affairs, Health Services Research and Development. Dr. Bryson was supported by VA Career Development Award 03-177. Dr. Jackson was supported for a portion of this project by a VA Career Development Award. Dr. Piette is a VA Senior Research Career Scientist; Dr. Maciejewski and Dr. Yano are VA Research Career Scientists. Dr. Wong was supported by VA Health Services Research and Development Postdoctoral Fellowship TPP 61-024. An earlier version of this manuscript was presented as a poster at the Society of General Internal Medicine 32nd Annual Meeting in Miami, FL in 2009. Dr. Bryson takes responsibility for the integrity of the data and the accuracy of the data analysis. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
All authors are federal employees for the Department of Veterans Affairs. Dr. Au has received consultation funds from Bosch Inc. and a grant from Gilead Sciences. Dr. Maciejewski has received consultation funds from Takeda Pharmaceuticals, Novartis and the Surgical Review Corporation. Dr. Maciejewski also owns stock in Amgen.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bryson, C.L., Au, D.H., Maciejewski, M.L. et al. Wide Clinic-Level Variation in Adherence to Oral Diabetes Medications in the VA. J GEN INTERN MED 28, 698–705 (2013). https://doi.org/10.1007/s11606-012-2331-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2331-y