ABSTRACT
BACKGROUND
Specialty referral patterns can affect health care costs as well as clinical outcomes. For a given clinical problem, referring physicians usually have a choice of several physicians to whom they can refer. Once the decision to refer is made, the choice of individual physician may have important downstream effects.
OBJECTIVE
To examine the reasons why primary care and specialist physicians choose certain specific colleagues to refer to and how those reasons differ by specialty.
DESIGN
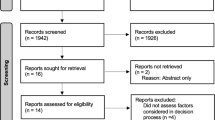
Cross-sectional Web-based survey supplemented with analysis of administrative claims data.
PARTICIPANTS
A total of 616 physicians in office-based patient care specialties who were members of an academic physicians’ organization and treated Medicare patients in 2006.
MAIN MEASURES
A total of 386 respondents (63% response rate) were presented with a “roster” of other physicians’ names with whom we predicted they had a relationship based on sharing Medicare patients. Among physicians in their “professional network” (consisting of any listed physician with whom respondents acknowledged a professional relationship), respondents reported if they referred to those physicians, and if so, provided up to two reasons why they referred to that particular colleague. Using logistic regression, we examined the likelihood that different specialists would endorse specific reasons for referring to chosen colleagues.
KEY RESULTS
Primary care physicians (PCPs) initiated referrals to 66% of their “professional network” colleagues, while medical and surgical specialists initiated referrals to 49% and 52%, respectively (p < 0.001 for both versus PCPs). After adjustment, medical specialists were less likely than PCPs to cite ease of communication with colleagues (RR = 0.69, 95% CI = 0.49–0.91), and medical and surgical specialists were less likely than PCPs to cite “shares my medical record system” as a reason to refer (medical specialist RR = 0.13, 95% CI 0.03–0.40, surgical specialist RR = 0.26, 95% CI = 0.05–0.78).
CONCLUSIONS
Specialists frequently initiate referrals, bypassing PCPs. In choosing specific physicians to refer to, PCPs are more often concerned with between-physician communication and patient access. Modifying referral practices among doctors may need to account for such patterns of behavior.
Similar content being viewed by others
References
Glenn JK, Lawler FH, Hoerl MS. Physician referrals in a competitive environment. An estimate of the economic impact of a referral. JAMA. 1987;258:1920–3.
Boulware LE, Troll MU, Jaar BG, Myers DI, Powe NR. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48:192–204.
Franks P, Zwanziger J, Mooney C, Sorbero M. Variations in primary care physician referral rates. Health Serv Res. 1999;34:323–9.
Forrest CB, Nutting PA, Starfield B, von Schrader S. Family physicians' referral decisions: results from the ASPN referral study. J Fam Pract. 2002;51:215–22.
Schneider EC, Epstein AM. Influence of cardiac-surgery performance reports on referral practices and access to care. A survey of cardiovascular specialists. N Engl J Med. 1996;335:251–6.
Selby JV, Schmittdiel JA, Lee J, et al. Meaningful variation in performance: what does variation in quality tell us about improving quality? Med Care. 2010;48:133–9.
Safran DG, Karp M, Coltin K, et al. Measuring patients' experiences with individual primary care physicians. Results of a statewide demonstration project. J Gen Intern Med. 2006;21:13–21.
Sirovich B, Gottlieb D, Welch H, Fisher E. Variation in the Tendency of Primary Care Physicians to Intervene. Archives of Internal Medicine. 2005;165:2252.
Lucas FL, Sirovich BE, Gallagher PM, Siewers AE, Wennberg DE. Variation in cardiologists' propensity to test and treat: is it associated with regional variation in utilization? Circ Cardiovasc Qual Outcomes. 2010;3:253–60.
Song Z, Safran DG, Landon BE, et al. Health Care Spending and Quality in Year 1 of the Alternative Quality Contract. New England Journal of Medicine;0.
Javalgi R, Joseph WB, Gombeski WR Jr, Lester JA. How physicians make referrals. J Health Care Mark. 1993;13:6–17.
Kinchen K, Cooper L, Levine D, Wang N, Powe N. Referral of patients to specialists: factors affecting choice of specialist by primary care physicians. Ann Family Med. 2004;2:245–52.
Forrest CB, Nutting PA, von Schrader S, Rohde C, Starfield B. Primary care physician specialty referral decision making: patient, physician, and health care system determinants. Med Decis Making. 2006;26:76–85.
Forrest CB, Reid RJ. Prevalence of health problems and primary care physicians' specialty referral decisions. J Fam Pract. 2001;50:427–32.
Shea D, Stuart B, Vasey J, Nag S. Medicare physician referral patterns. Health Serv Res. 1999;34:331–48.
Forrest CB. A typology of specialists' clinical roles. Arch Intern Med. 2009;169:1062–8.
Barnett ML, Landon BE, O'Malley AJ, Keating NL, Christakis NA. Mapping Physician Networks with Self-Reported and Administrative Data. Health Serv Res, Epub April 28, 2011.
Pagano M, Gauvreau K. Principles of Biostatistics: 2nd Edition. 2nd ed. Pacific Grove, CA: Duxbury; 2000.
Carey VJ. gee: Generalized Estimation Equation solver. In. R package version 4.13-16 ed; 2010.
Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1.
King G, Tomz M, Wittenberg J. Making the Most of Statistical Analyses: Improving Interpretation and Presentation. Am J Polit Sci. 2000;44:341–55.
R Development Core Team. R: A language and environment for statistical computing. In. Vienna, Austria: R Foundation for Statistical Computing; 2009.
Imai K, King G, Lau O. Zelig: Everyone's Statistical Software. In. R package version 3.4-8 ed; 2010.
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502.
Keirns CC, Goold SD. Patient-centered care and preference-sensitive decision making. JAMA. 2009;302:1805–6.
Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA. 2006;296:2848–51.
Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–52.
Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–36.
Contributors
We gratefully acknowledge Georgina Barahona for research assistance, and Laurie Meneades for expert data management and technical support.
Funders
Supported by a grant from National Institute of Aging (P-01 AG-031093). Mr. Barnett’s effort was supported by a Doris Duke Charitable Foundation Clinical Research Fellowship and a Harvard Medical School Research Fellowship.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
APPENDIX TABLE
APPENDIX TABLE
Rights and permissions
About this article
Cite this article
Barnett, M.L., Keating, N.L., Christakis, N.A. et al. Reasons for Choice of Referral Physician Among Primary Care and Specialist Physicians. J GEN INTERN MED 27, 506–512 (2012). https://doi.org/10.1007/s11606-011-1861-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1861-z