Abstract
Background
Little is known about first-fill adherence rates for diabetic medications and factors associated with non-fill.
Objective
To assess the proportion of patients who fill their initial prescription for a diabetes medication, understand characteristics associated with prescription first-fill rates, and examine the effect of first-fill rates on subsequent A1c levels.
Design
Retrospective, cohort study linking electronic health records and pharmacy claims.
Participants
One thousand one hundred thirty-two patients over the age of 18 who sought care from the Geisinger Clinic, had Geisinger Health Plan pharmacy benefits, and were prescribed a diabetes medication for the first time between 2002 and 2006.
Measurements
The primary outcome of interest was naïve prescription filled by the patient within 30 days of the prescription order date.
Results
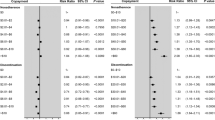
The overall first-fill adherence rate for antidiabetic drugs was 85%. Copays < $10 (OR 2.22, 95% CI 1.57–3.14) and baseline A1c > 9% (OR 2.63, 95% CI 1.35, 5.09) were associated with improved first-fill rates while sex, age, and co-morbidity score had no association. A1c levels decreased among both filling and non-filling patients though significantly greater reductions were observed among filling patients. Biguanides and sulfonylureas had higher first-fill rates than second-line oral agents or insulin.
Conclusions
First-fill rates for diabetes medication have room for improvement. Several factors that predict non-filling are readily identifiable and should be considered as possible targets for interventions.
Similar content being viewed by others
Abbreviations
- HER:
-
Electronic Health Records
- GHP:
-
Geisinger Health Plan
- A1c:
-
Hemoglobin A1c
References
Haynes TB, Taylor DW, Sackett DL. Compliance in Health Care. Baltimore, MD: Johns Hopkins University Press; 1979.
Balkrishnan R. The importance of medication adherence in improving chronic-disease related outcomes: what we know and what we need to further know. Med Care. 2005;43(6):517–20.
Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff (Millwood). 2003;22(4)220–9.
McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288(22):2868–79.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5)373–83.
Rothman KJ, Greenland S. Modern Epidemiology, 2nd edn. New York: Lippincott Williams & Wilkins; 1998.
Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diab Care. 2004;27(12):2800–5.
Schetman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an indigent population. Diab Care. 2002;25(6):1015–21.
Kienle GS, Kiene H. The powerful placebo effect: Fact or fiction? J Clin Epi. 1997;50(12):1311–8.
Johnson RE, Goodman MJ, Hornbrook MC, Eldredge MB. The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Med Care. 1997;35:1119–31.
Babazono A, Tsuda T, Yamamoto E, Mino Y, Une H, Hillman AL. Effects of an increase in patient copayments on medical service demands of the insured in Japan. Int J Technol Assess Health Care. 2003;19(3):465–75.
Chernew M, Gibson TB, Yu-Isenberg K, Sokol MC, Rosen AB, Fendrick AM. Effects of increased patient cost sharing on socioeconomic disparities in health care. J Gen Int Med 2008;epub ahead of print.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–9.
van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, Bensing J. Patient adherence to medical treatment: A review of reviews. BMC Health Services Research. 2007;7(55).
Ho PM, Magid DJ, Shetterly SM, et al. Importance of therapy intensification and medication nonadherence for blood pressure control in patients with coronary disease. Arch Intern Med. 2008;168(3):271–6.
Schmittdiel JA, Uratsu CS, Karter AJ, et al. Why don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. J Gen Intern Med. 2008;23(5):588–94.
American Diabetes Association. Diabetes statistics. Available at http://www.diabetes.org/diabetes-statistics.jsp. Accessed on May 7, 2008.
Acknowledgements
This work was supported by an unrestricted grant from Novartis Pharmaceuticals Corporation. Dr. Shah receives support from the Robert Wood Johnson Foundation as a Physician Faculty Scholar. None of the funders played any role in the design or conduct of the study, in the collection, analysis, or interpretation of the data, or in the preparation, review, or approval of the manuscript. Dr. Shah had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Nirav Shah has received unrestricted research grants from AstraZeneca, Berlex, GlaxoSmithKline, Merck, Novartis, Pfizer, and Roche; he has served as a consultant for Cerner Lifesciences and LifeTech Research. None of the authors have any financial interests in any of the devices or companies mentioned in this report, except that Chris Zacker works for the sponsor of this study.
Nirav Shah, Annemarie Hirsch, Scott Taylor, Chris Zacker, and Walter Stewart all played significant roles in the data collection, analysis, and write-up of the manuscript. Nirav Shah, Scott Taylor, and Walter Stewart conceived of the idea and obtained funding. Nirav Shah is the guarantor of the manuscript. Design and conduct of the study: Nirav Shah, Scott Taylor, Annemarie Hirsh, Walter Stewart, Chris Zacker; Collection, management, analysis: Nirav Shah, Craig Wood, Annemarie Hirsch; Interpretation of the data: Nirav Shah, Annemarie Hirsch, Scott Taylor, Walter Stewart, Craig Wood, Chris Zacker; Preparation, review, or approval of the manuscript: Nirav Shah, Annemarie Hirsch, Scott Taylor, Walter Stewart, Craig Wood.
Conflict of Interest Statement
Annemarie G. Hirsch, Scott Taylor, and G. Craig Wood report no conflicts of interest. Nirav R. Shah has held a consultancy position for Cerner LifeSciences within the past 3 years and has received grants from GlaxoSmithKline, Novartis, Roche Diagnostics, AstraZeneca, and Merck. Christopher Zacker has been employed with Novartis. Walter F. Stewart has received grants within the past 3 years from GlaxoSmithKline, Novartis, Roche Diagnostics, AstraZeneca, and Merck.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, N.R., Hirsch, A.G., Zacker, C. et al. Factors Associated with First-Fill Adherence Rates for Diabetic Medications: A Cohort Study. J GEN INTERN MED 24, 233–237 (2009). https://doi.org/10.1007/s11606-008-0870-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0870-z