Abstract
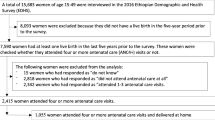
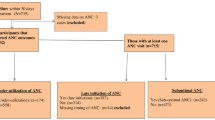
Objective While antenatal care does not directly contribute to reducing maternal mortality, it may play an indirect role by encouraging women to deliver with a skilled birth attendant or in a health facility. We investigated whether the frequency of visits and select characteristics of antenatal care were associated with facility delivery. Methods We selected a population-representative sample of households in a rural district of western Tanzania. Women who had given birth within five years were asked about their most recent delivery and antenatal care. Results Of 1,204 women interviewed, 1,195 (99.3%) made at least one antenatal care visit, while only 438 (36.4%) delivered in a health facility. In adjusted analysis, women were significantly more likely to deliver in a health facility if they attended antenatal care at a government health center (OR 3.17, 95% CI: 1.60–6.30) or a mission facility (OR 2.87, 95% CI: 1.36–6.07), rather than a government dispensary. Women were significantly less likely to deliver in a health facility if their nearest health facility was outside their village (OR 0.38, 95% CI: 0.22–0.66). Conclusion Though facility utilization for antenatal care is frequent, most women who accessed antenatal care did not deliver in a health facility. Women who obtained antenatal care at higher level government facilities or mission facilities, which offered better quality of care, were more likely to deliver in any facility. Improving the quality of antenatal care may improve the health of mothers through encouraging women to return to facilities for delivery.
Similar content being viewed by others
References
Freedman, L. W. M., Waldman, R., Chowdhury, M., & Rosenfield, A. (2004). Millennium project task force 4 child health and maternal health: Interim report. New York: United Nations.
Khan, K. S., Wojdyla, D., Say, L., Gulmezoglu, A. M., & Van Look, P. F. (2006). WHO analysis of causes of maternal death: A systematic review. Lancet, 367(9516), 1066–1074. doi:10.1016/S0140-6736(06)68397-9.
Campbell, O. M., & Graham, W. J. (2006). Strategies for reducing maternal mortality: Getting on with what works. Lancet, 368(9543), 1284–1299. doi:10.1016/S0140-6736(06)69381-1.
Kerber, K. J., de Graft-Johnson, J. E., Bhutta, Z. A., Okong, P., Starrs, A., & Lawn, J. E. (2007). Continuum of care for maternal, newborn, and child health: From slogan to service delivery. Lancet, 370(9595), 1358–1369. doi:10.1016/S0140-6736(07)61578-5.
Implementation of the UN Millennium Declaration Report of the UN Secretary General. (2004). Report number A/59/282. New York: The United Nations General Assembly 27 August.
Villar, J., & Bergsjo, P. (1997). Scientific basis for the content of routine antenatal care. I. Philosophy, recent studies, and power to eliminate or alleviate adverse maternal outcomes. Acta Obstetricia et Gynecologica Scandinavica, 76(1), 1–14. doi:10.3109/00016349709047778.
Villar, J., Ba’aqeel, H., Piaggio, G., Lumbiganon, P., Miguel Belizan, J., Farnot, U., et al. (2001). WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet, 357(9268), 1551–1564. doi:10.1016/S0140-6736(00)04722-X.
Darmstadt, G. L., Bhutta, Z. A., Cousens, S., Adam, T., Walker, N., & de Bernis, L. (2005). Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet, 365(9463), 977–988. doi:10.1016/S0140-6736(05)71088-6.
Barber, S. (2006). Does the quality of prenatal care matter in promoting skilled institutional delivery? A study in rural Mexico. Maternal and Child Health Journal, 10(5), 419–425. doi:10.1007/s10995-006-0079-x.
Bloom, S. S., Lippeveld, T., & Wypij, D. (1999). Does antenatal care make a difference to safe delivery? A study in urban Uttar Pradesh, India. Health Policy and Planning, 14(1), 38–48. doi:10.1093/heapol/14.1.38.
Stephenson, R., Baschieri, A., Clements, S., Hennink, M., & Madise, N. (2006). Contextual influences on the use of health facilities for childbirth in Africa. American Journal of Public Health, 96(1), 84–93. doi:10.2105/AJPH.2004.057422.
World Health Organization. (2007). Maternal mortality in 2005: Estimates developed by WHO, UNICEF, UNFPA and The World Bank.
National Bureau of Statistics.Dar es Salaam, United Republic of Tanzania, ORC Macro Calverton, Maryland, USA. (2005). Tanzania Demographic and Health Survey.
National Bureau of Statistics.Dar es Salaam, United Republic of Tanzania, ORC Macro Calverton, Maryland, USA. (2006). Tanzania Service Provision Assessment Survey.
National Bureau of Statistics. Dar es Salaam, United Republic of Tanzania. (2008). 2002 Tanzania Census.
Dovlo, D. (2004). Using mid-level cadres as substitutes for internationally mobile health professionals in Africa. A desk review. Human Resources for Health, 2(1), 7. doi:10.1186/1478-4491-2-7.
Filmer, D., & Pritchett, L. H. (2001). Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography, 38(1), 115–132.
Research Triangle Institute. (2005). SUDAAN. 9.0.3 ed. Research Triangle Park, NC.
Gilson, L. (1995). Management and health care reform in sub-Saharan Africa. Social Science and Medicine, 40(5), 695–710. doi:10.1016/0277-9536(94)E0111-5.
World Health Organization. (2007). Standards for Maternal and Neonatal Care.
Leonard, K. (2007). Learning in health care: Evidence of learning about clinican quality in Tanzania. Economic Development and Cultural Change, 55, 531–555. doi:10.1086/511192.
Thind, A., Mohani, A., Banerjee, K., & Hagigi, F. (2008). Where to deliver? Analysis of choice of delivery location from a national survey in India. BMC Public Health, 8(29), 29. doi:10.1186/1471-2458-8-29.
Chowdhury, M. E., Ronsmans, C., Killewo, J., Anwar, I., Gausia, K., Das-Gupta, S., et al. (2006). Equity in use of home-based or facility-based skilled obstetric care in rural Bangladesh: an observational study. Lancet, 367(9507), 327–332. doi:10.1016/S0140-6736(06)68070-7.
Anwar, I., Sami, M., Akhtar, N., Chowdhury, M. E., Salma, U., Rahman, M., et al. (2008). Inequity in maternal health-care services: Evidence from home-based skilled-birth-attendant programmes in Bangladesh. Bulletin of the World Health Organization, 86, 252–259. doi:10.2471/BLT.07.042754.
Mrisho, M., Schellenberg, J. A., Mushi, A. K., Obrist, B., Mshinda, H., Tanner, M., et al. (2007). Factors affecting home delivery in rural Tanzania. Tropical Medicine & International Health, 12(7), 862–872.
Acknowledgements
We thank Professor Sandro Galea for his guidance in the design of the study, and analysis and interpretation of the data. We thank the women from Kasulu District for their willingness to participate in the study. This work was funded by the William Davidson Institute at the Ross School of Business, University of Michigan, the Averting Maternal Death and Disability Program at the Mailman School of Public Health, Columbia University, and the Global Health Program at the School of Public Health, University of Michigan. The funders did not have any involvement in conducting the study or in deciding to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rockers, P.C., Wilson, M.L., Mbaruku, G. et al. Source of Antenatal Care Influences Facility Delivery in Rural Tanzania: A Population-Based Study. Matern Child Health J 13, 879–885 (2009). https://doi.org/10.1007/s10995-008-0412-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-008-0412-7