Abstract
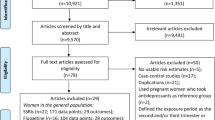
Evidence of an association between early pregnancy exposure to selective serotonin reuptake inhibitors (SSRI) and congenital heart defects (CHD) has contributed to recommendations to weigh benefits and risks carefully. The objective of this study was to determine the specificity of association between first trimester exposure to SSRIs and specific CHD and other congenital anomalies (CA) associated with SSRI exposure in the literature (signals). A population-based case-malformed control study was conducted in 12 EUROCAT CA registries covering 2.1 million births 1995–2009 including livebirths, fetal deaths from 20 weeks gestation and terminations of pregnancy for fetal anomaly. Babies/fetuses with specific CHD (n = 12,876) and non-CHD signal CA (n = 13,024), were compared with malformed controls whose diagnosed CA have not been associated with SSRI in the literature (n = 17,083). SSRI exposure in first trimester pregnancy was associated with CHD overall (OR adjusted for registry 1.41, 95 % CI 1.07–1.86, fluoxetine adjOR 1.43 95 % CI 0.85–2.40, paroxetine adjOR 1.53, 95 % CI 0.91–2.58) and with severe CHD (adjOR 1.56, 95 % CI 1.02–2.39), particularly Tetralogy of Fallot (adjOR 3.16, 95 % CI 1.52–6.58) and Ebstein’s anomaly (adjOR 8.23, 95 % CI 2.92–23.16). Significant associations with SSRI exposure were also found for ano-rectal atresia/stenosis (adjOR 2.46, 95 % CI 1.06–5.68), gastroschisis (adjOR 2.42, 95 % CI 1.10–5.29), renal dysplasia (adjOR 3.01, 95 % CI 1.61–5.61), and clubfoot (adjOR 2.41, 95 % CI 1.59–3.65). These data support a teratogenic effect of SSRIs specific to certain anomalies, but cannot exclude confounding by indication or associated factors.
Similar content being viewed by others
References
Bijl R, Ravelli A, Van Zessen G. Prevalence of psychiatric disorder in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998;33(12):587–95.
Meyer C, Rumpf H, Hapke U, Dilling H, John U. Lifetime prevalence of mental disorders in general adult population. Results of TACOS study. Nervenarzt. 2000;71(7):535.
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand. 2004;420:21–7.
Jacobi F, Wittchen HU, Holting C, Hofler M, Pfister H, Muller N, et al. Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS). Psychol Med. 2004;34(4):597–612.
Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, Koren G. Perinatal risks of untreated depression during pregnancy. Can J Psychiatry. 2004;49(11):726–35.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384:1800–19.
Lo WY, Friedman JM. Teratogenicity of recently introduced medications in human pregnancy. Obstet Gynecol. 2002;100(3):465–73.
NICE. Antenatal and postnatal mental health: clinical management and service guidance. London: British Psychological Society and Gaskell; 2007.
Andrade SE, Gurwitz JH, Davis RL, Chan KA, et al. Prescription drug use in pregnancy. Obstet Gynecol. 2004;191(2):398–407.
Ververs T, Kaasenbrood H, Visser G, Schobben F, de Jong-van den Berg L, Egberts T. Prevalence and patterns of antidepressant drug use during pregnancy. Eur J Clin Pharmacol. 2006;62(10):863–70.
Ramos E, Oraichi D, Rey E, Blais L, Berard A. Prevalence and predictors of antidepressant use in a cohort of pregnant women. BJOG. 2007;114(9):1055–64.
Petersen I, Gilbert RE, Evans SJW, Man S, Nazareth I. Pregnancy as a major determinant for discontinuation of antidepressants: an analysis of data from the health improvement network. J Clin Psychiatry. 2011;72(7):979–85.
Cooper WO, Willy ME, Pont SJ. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544e1–5.
Charlton R, Jordan S, Pierini A, Garne E, Neville A, Hansen A, Gini R, Thayer D, Tingay K, Puccini A, Bos H, Nybo Andersen A, Sinclair M, Dolk H, de Jong-van den Berg L. Selective serotonin reuptake inhibitor prescribing before, during and after pregnancy: a population-based study in six European regions. BJOG. 2014;. doi:10.1111/1471-0528.13143.
Andrade SE, Raebel MA, Brown J, Lane K, Livingston J, Boudreau D, et al. Use of antidepressant medications during pregnancy: a multisite study. Obstet Gynecol. 2008;198(2):194.e1–5.
Bakker MK, Kolling P, van den Berg PB, de Walle HE, de Jong van den Berg LT. Increase in use of selective serotonin reuptake inhibitors in pregnancy during the last decade, a population-based cohort study from the Netherlands. Br J Clin Pharmacol. 2008;65(4):600–6.
Pastuszak A, Schick-Boschetto B, Zuber C, Feldkamp M, Pinelli M, Sihn S, et al. Pregnancy outcome following first-trimester exposure to fluoxetine (Prozac). J Am Med Assoc. 1993;269(17):2246–8.
Chambers CD, Johnson KA, Dick LM. Birth outcomes in pregnant women taking fluoxetine. N Engl J Med. 1996;335(14):1010–5.
Kulin NA, Pastuszak A, Sage SR, Schick-Boschetto B, Spivey G, Feldkamp M, et al. Pregnancy outcome following maternal use of the new selective serotonin reuptake inhibitors; a prospective controlled multicenter study. J Am Med Assoc. 1998;279(8):609–10.
Simon GE, Cunningham ML, Davis RL. Outcomes of prenatal antidepressant exposure. Am J Psychiatry. 2002;159(12):2055–61.
Kallen B. Fluoxetine use in early pregnancy. Birth Defects Res B Dev Reprod Toxicol. 2004;71(6):395–6.
GlaxoSmithKline. Preliminary report on bupropion in pregnancy and the occurrence of cardiovascular and major congenital malformation. 2005.
Ban L, Gibson JE, West J, Fiaschi L, Sokal R, Smeet L, Doyle P, Hubbard RB, Tata LJ. Maternal depression, antidepressant prescriptions, and congenital anomaly risk in offspring: a population based cohort study. BJOG. 2014;121:1471–81.
Davis RL, Rubanowice D, McPhillips H. Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiol Drug Saf. 2007;16(10):1086–94.
Cole JA, Ephross SA, Cosmatos IS, Walker AM. Paroxetine in the first trimester and the prevalence of congenital malformations. Pharmacoepidemiol Drug Saf. 2007;16(10):1075–85.
Diav-Citrin O, Shechtman S, Weinbaum D, Wajnberg R, Avgil M, Di Gianantonio E, et al. Paroxetine and fluoxetine in pregnancy: a prospective, multicentre, controlled, observational study. Br J Clin Pharmacol. 2008;66(5):695–705.
Merlob P, Birk E, Sirota L, Linder N, Berant M, Stahl B, et al. Are selective serotonin reuptake inhibitors cardiac teratogens? Echocardiographic screening of newborns with persistent heart murmur. Birth Defects Res A Clin Mol Teratol. 2009;85(10):837–41.
Pedersen LH, Henriksen TB, Vestergaard M, Olsen J, Bech BH. Selective serotonin reuptake inhibitors in pregnancy and congenital malformations: population based cohort study. BMJ. 2009;23(339):b3569.
Reis M, Kallen B. Delivery outcome after maternal use of antidepressant drugs in pregnancy: an update using Swedish data. Psychol Med. 2010;40(10):1723–33.
Kornum JB, Nielsen RB, Pedersen L, Mortensen PB, Norgaard M. Use of selective serotonin-reuptake inhibitors during early pregnancy and risk of congenital malformations: updated analysis. Clin Epidemiol. 2010;9(2):29–36.
Malm H, Artama M, Gissler M, Ritvanen A. Selective serotonin reuptake inhibitors and risk for major congenital anomalies. Obstet Gynecol. 2011;118(1):111–20.
Colvin L, Slack-Smith L, Stanley FJ, Bower C. Dispensing patterns and pregnancy outcomes for women dispensed selective serotonin reuptake inhibitors in pregnancy. Birth Defects Res A Clin Mol Teratol. 2011;91(3):142–52.
Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Jensen JK, Afzal S, et al. Exposure to selective serotonin reuptake inhibitors and the risk of congenital malformations: a nationwide cohort study. BMJ Open. 2012;. doi:10.1136/bmjopen-012-001148.
Alwan S, Reefhuis J, Rasmussen SA, Olney RS, Friedman JM. National birth defects prevention study. use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. N Engl J Med. 2007;356(26):2684–92.
Louik C, Lin AE, Werler MM, Hernandez-Diaz S, Mitchell AA. First-trimester use of selective serotonin-reuptake inhibitors and the risk of birth defects. N Engl J Med. 2007;356(26):2675–83.
Bakker MK, Kerstjens-Frederikse WS, Buys CH, de Walle HE, de Jong-van den Berg LT. First-trimester use of paroxetine and congenital heart defects: a population-based case-control study. Birth Defects Res A Clin Mol Teratol. 2010;88(2):94–100.
Berard A, Ramos E, Rey E, Blais L, St-Andre M, Oraichi D. First trimester exposure to paroxetine and risk of cardiac malformations in infants: the importance of dosage. Birth Defects Res B Dev Reprod Toxicol. 2007;80(1):18–27.
Sivojelezova A, Shuhaiber S, Sarkissian L, Einarson A, Koren G. Citalopram use in pregnancy: prospective comparative evaluation of pregnancy and fetal outcome. Obstet Gynecol. 2005;193(6):2004–9.
Wen SW, Yang Q, Garner P, Fraser W, Olatunbosun O, Nimrod C, et al. Selective serotonin reuptake inhibitors and adverse pregnancy outcomes. Obstet Gynecol. 2006;194(4):961–6.
Einarson A, Pistelli A, DeSantis M, Malm H, Paulus WD, Panchaud Alice, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749–52.
Manakova E, Hubickova L. Antidepressant drug exposure during pregnancy. CZTIS small prospective study. Neuro Endocrinol Lett. 2011;32(Suppl 1):53–6.
Klieger-Grossmann C, Weitzner B, Panchaud A, Pistelli A, Einarson T, Koren G, et al. Pregnancy outcomes following use of escitalopram: a prospective comparative cohort study. J Clin Pharmacol. 2012;52(5):766–70.
Nordeng H, van Gelder MM, Spigset O, Koren G, Einarson A, Eberhard-Gran M. Pregnancy outcome after exposure to antidepressants and the role of maternal depression: results from the Norwegian Mother and Child Cohort Study. J Clin Psychopharmacol. 2012;32(2):186–94.
Reis M, Kallen B. Combined use of selective serotonin reuptake inhibitors and sedatives/hypnotics during pregnancy: risk of relatively severe congenital malformations or cardiac defects. A register study. BMJ Open. 2013;. doi:10.1136/bmjopen-2012-002166.
Vasilakis-Scaramozza C, Aschengrau A, Cabral H, Jick SS. Antidepressant use during early pregnancy and the risk of congenital anomalies. Pharmacother J Human Pharmacol Drug Ther. 2013;33(7):693–700.
Wurst KE, Poole C, Ephross SA, Olshan AF. First trimester paroxetine use and the prevalence of congenital, specifically cardiac, defects: a meta-analysis of epidemiological studies. Birth Defects Res A Clin Mol Teratol. 2010;88(3):159–70.
Myles N, Newall H, Ward H, Large M. Systematic meta-analysis of individual selective serotonin reuptake inhibitor medications and congenital malformations. Aust N Z J Psychiatry. 2013;47(11):1002–12.
Koren G, Nordeng HME. Selective serotonin reuptake inhibitors and malformations: case closed? Semin Fetal Neonatal Med. 2013;18:19–22.
Painuly N, Heun R, Painuly R, Sharan P. Risk of cardiovascular malformations after exposure to paroxetine in pregnancy: meta-analysis. The Psychiatrist. 2013;37(6):198–203.
Grigoriadis S, VonderPorten EH, Mamisashvili L, Roerecke M, Rehm J, Dennis C, et al. Antidepressant exposure during pregnancy and congenital malformations: Is there an association? A systematic review and meta-analysis of the best evidence. J Clin Psychiatry. 2013;74(4):e293–308.
Skurtveit S, Selmer R, Tverdal A, Furu K, Nystad W, Handal M. Drug exposure: inclusion of dispensed drugs before pregnancy may lead to underestimation of risk associations. J Clin Epidemiol. 2013;66:964–72.
Olivier JDA, Akerud H, Kaihola H, Pawluski JL, Skalkidou A, Hogberg U, et al. The effects of maternal depression and maternal selective serotonin reuptake inhibitor exposure on the offspring. Front Clin Neurosci. 2013;7:73.
Preskorn Sheldon H. Clinically relevant pharmacology of selective serotonin reuptake inhibitors. Clin Pharmacokinet. 1997;32(1):1–21.
Sadler TW. Selective serotonin reuptake inhibitors (SSRIs) and heart defects: potential mechanisms for the observed associations. Reprod Toxicol. 2011;32(4):484–9.
Choi DS, Kellermann O, Richard S, Colas JF, Bolanos-Jimenez F, Tournois C, Launay J, Maroteaux L. Mouse 5-HT2B receptor-mediated serotonin trophic functions. Ann NY Acad Sci. 1998;861(1):67–73.
Sari Y, Zhou FC. Serotonin and its transporter on proliferation of fetal heart cells. Int J Dev Neurosci. 2003;21(8):417–24.
Scialli AR. Paroxetine exposure during pregnancy and cardiac malformations. Birth Defects Res A Clin Mol Teratol. 2010;88(3):175–7.
Bar-Oz B, Einarson T, Einarson A, Boskovic R, O’Brien L, Malm H, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918–26.
Huybrechts KF, Palmsten K, Avorn J, Cohen LS, Holmes LB, Franklin JM, Mogun H, Levin R, Kowal M, Setoguchi S, Hernandez-Diaz S. N Engl J Med. 2014;370:2397–407.
Boyd PA, Haeusler M, Barisic I, Loane M, Garne E, Dolk H. Paper 1: the EUROCAT network-organization and processes. Birth Defects Res A Clin Mol Teratol. 2011;91(Suppl 1):S2–15.
Jentink J, Loane MA, Dolk H, Barisic I, Garne E, Morris JK, de Jong-van den Berg LTW, EUROCAT Antiepileptic Drug Working Group. Valproic acid monotherapy exposure in the first trimester of pregnancy and risk of specific birth defects. N Engl J Med. 2010;362(23):2185–93.
Greenlees R, Neville A, Addor MC, Amar E, Arriola L, Bakker M, et al. Paper 6: eUROCAT member registries: organization and activities. Birth Defects Res A Clin Mol Teratol. 2011;91(Suppl 1):S51–100.
EUROCAT. EUROCAT Guide 1.3 and reference documents. Instructions for the registration and surveillance of congenital anomalies. http://www.eurocat-network.eu/aboutus/datacollection/guidelinesforregistration/guide1_3instructionmanual (2005). Accessed Nov 2014.
Dolk H, Loane M, Garne E, EUROCAT Working Group. Congenital heart defects in Europe: prevalence and perinatal mortality, 2000 to 2005. Circulation. 2011;123:841–9.
Garne E, Dolk H, Loane M, Wellesley D, Barisic I, Calzolari E, et al. Paper 5: surveillance of multiple congenital anomalies: implementation of a computer algorithm in European registers for classification of cases. Birth Defects Res A. 2011;91(S1):S44–50.
Wellesley D, Boyd P, Dolk H, Pattenden S. An aetiological classification of birth defects for epidemiological research. J Med Genetics. 2005;42(1):54–7.
Rasmussen SA, Olney RS, Holmes LB, Lin AE, Keppler-Noreuil KM, Moore CA, et al. Guidelines for case classification for the National Birth Defects Prevention Study. Birth Defects Res. 2003;67(3):193–201.
Bakker, M, De Jonge L. EUROCAT Special Report: Sources of information on medication use in pregnancy. http://www.eurocat-network.eu/content/Special-Report-Medication-Use-In-Pregnancy.pdf. Accessed Nov 2014.
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2010. http://www.whocc.no/atc_ddd_index/ (2009) Accessed 24 April 2010.
Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–6.
Palmsten K, Huybrechts KF, Kowal MK, Mogun H, Hernandez-Diaz S. Validity of maternal and infant outcomes within nationwide Medicaid data. Pharmacoepidemiol Drug Saf. 2014;23:646–55.
Carmichael SL, Shaw GM, Yang W, Abrams B, Lammer EJ. Maternal stressful life events and risks of birth defects. Epidemiology. 2007;18(3):356–61.
Källén B, Tandberg A. Lithium and pregnancy. A cohort study on manic-depressive women. Acta Psychiatr Scand. 1983;68(2):134–9.
Jones I, Chandra PS, Dazzan P, Howard LM. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384:1789–99.
Torfs CP, Velie EM, Oechsli FW, Bateson TF, Curry CJR. A population-based study of gastroschisis: demographic, pregnancy, and lifestyle risk factors. Teratology. 1994;50(1):44–53.
Stothard KJ, Tennant PWG, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies. JAMA J Am Med Assoc. 2009;301(6):636–50.
Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum Reprod Update. 2011;17(5):589–604.
Martínez-Frías ML, Bermejo E, Rodríguez-Pinilla E, Frías JL. Risk for congenital anomalies associated with different sporadic and daily doses of alcohol consumption during pregnancy: a case–control study. Birth Defects Res A. 2004;70(4):194–200.
Krauss MJ, Morrissey AE, Winn HN, Amon E, Leet TL. Microcephaly: an epidemiologic analysis. Obstet Gynecol. 2003;188(6):1484–90.
Johansen RLR, Mortensen LH, Nybo Andersen A-M, Vinkel Hansen A, Strandberg-Larsen K. Maternal use of selective serotonin reuptake inhibitors and risk of miscarriage—assessing potential biases. Paediatr Perinatal Epidemiol. 2014;. doi:10.1111/ppe.12160.
Czeizel AE, Puho EH, Acs N, Banhidy F. Use of specified critical periods of different congenital abnormalities instead of the first trimester concept. Birth Defects Res Part A Clin Molecul Teratol. 2008;82(3):139–46.
Acknowledgments
We thank the many people throughout Europe involved in providing and processing information, including affected families, clinicians, health professionals, medical record clerks and registry staff.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
AW was funded by a Ulster University Vice Chancellor’s Research Studentship. EUROCAT is co-funded by the EC, under the framework of the EU Health Programme 2008–2013, Grant Agreement 2010 22 04 (Executive Agency for Health & Consumers). EUROCAT registries are funded as fully described in Paper 6 of EUROCAT Report 9—EUROCAT Member Registries: Organization and Activities.
Conflict of interest
The congenital anomaly registries and institutions where EG, MKB, DT, BK, VN, MoM, AP, MG, MCA, AR, LA, LdJvdB and HD are employed have previously received funding from Glaxo Smith Kline for a study of safety of antiepileptic lamotrigine use in pregnancy. No author has had any association with or interest in any antidepressant manufacturer in relation to the current study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wemakor, A., Casson, K., Garne, E. et al. Selective serotonin reuptake inhibitor antidepressant use in first trimester pregnancy and risk of specific congenital anomalies: a European register-based study. Eur J Epidemiol 30, 1187–1198 (2015). https://doi.org/10.1007/s10654-015-0065-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-015-0065-y