Abstract
This paper presents a comprehensive update of life expectancy and mortality in 2002–2004 in the modern European Union (EU-27) and EFTA countries. We focus on causes of death at younger ages (0–64 year). EUROSTAT delivered updated population numbers and mortality data by sex, age and cause of death for 272 NUTS-2 regions. We compared mortality by life tables, cause decomposition life tables and age standardized rates. Gini coefficients estimated inequity of death rates over the regions. Life expectancy at birth in the EU-27 was 75.1 years (men) and 81.3 years (women). The difference between the 10th and 90th percentile of 272 regions was 8.0 (men) and 5.6 years (women). Men lived 6.1 years shorter in the new member states (NMS, new members since 2004) than in the EU-15 (members before 2004), women 3.9 years. 60% (men) and 33% (women) of the differences in life expectancy between EU 15 and NMS were explained by mortality under age 65. The main causes explaining differences in life expectancy were ischemic and other heart disease, stroke, alcohol related mortality, lung cancer and injuries. The fraction of ill defined causes of death was large and very variable between countries. Mortality differences in the EU-27 are dominated by smoking, alcohol, diseases related to diet and a sedentary lifestyle, unsafe roads and differences in health care performance. Closing the health gap is feasible and ought to be a major target of the European Union, but monitoring will need better registration of causes of death.
Similar content being viewed by others
Europe is a small continent, but with a long history of cultural diversity. Europe has been starting to define itself as a political and economic entity, designed as the European Union (EU), with a supranational statistics office, EUROSTAT. Since 2007, the EU has 27 member states. In Central and Eastern former socialist economies, life expectancy is about 5 years lower than in the EU15 (the 15 EU member countries before 2004). Mortality statistics are cheap administrative data, which may give powerful insights what people die from and at what age. By monitoring mortality, vital statistics are able to monitor how and if Europe is unifying, not only in economy but also in health.
This paper aims at giving a comprehensive, succinct and accessible update on European mortality in the EU-27. Other descriptive studies we found are comprehensive but outdated [1], or succinct but focus on isolated causes of death [2–9]. We focused on life expectancy at birth and the most important causes of death under 65, taking into account regional variability. Mortality under 65 describes premature mortality, and waste of life years at young, adult or middle age. Causes of death are more specific at these younger ages, not yet confounded by multi-morbidity at old age and complex causation of death at the end of a long life. We compare the loss of life by cause of death before the age 65 in the EU between the new Member States and the EU 15 in decomposition life tables and identify the most variable causes of death.
Data and methods
We present mortality data from 2002, 2003 and 2004 by sex, 5 year group up to 85 and over and 271 NUTS-2 regions in the European Union and EFTA countries (Switzerland, Norway and Iceland; Liechtenstein offered no data). The Nomenclature of Territorial Units for Statistics (NUTS) was established to provide a uniform breakdown of territorial units in the European Union. All cause mortality data are unavailable from Belgium, only from Flanders (five of the ten Belgian NUTS-2 regions). For the Flemish regions of Belgium and for Italy the figures relate to the period 2000–2002, for Denmark to 1999–2001. Data were missing at the NUTS 2 level for Scotland, Denmark and Slovenia, mortality by cause was missing from Cyprus. We present life expectancies for thirty countries (Flanders replacing Belgium) and cause specific mortality for 29 countries (Flanders replacing Belgium, Cyprus omitted). Cause specific analyses are presented by the EU 27 (the European Union after the inclusion of Romania and Bulgaria in 2007), the EU 15 (the 15 EU member countries between 1995 and 2004, see abbreviations for individual members) and the New Member States (NMS: the 12 states that joined after 2004, see abbreviations for individual members) which are, except for the smaller populations of Malta and Cyprus, all central and eastern former socialist countries. We had cause specific mortality from 270 NUTS-2 regions, 201 from the EU 15, 54 from the NMS and 15 from the EFTA countries (Norway, Iceland and Switzerland).
Causes of death are classified by the 65 causes of the ‘European shortlist’ of causes of death, a summary list based on the International Statistical Classification of Diseases and Related Health Problems (ICD). Causes of death were selected by their frequency. Table 1 shows the selected causes and the corresponding codes in the Eurostat shortlist. These are organised as large ICD chapters and smaller disease groups (see Table 1).
We took the registered codes at face value, but included ill defined causes of death. (Symptoms, signs, abnormal findings, ill-defined causes, see Table 1.) For the disease groups, we aggregated cancers of the colon, rectum and anus because of known problems of misclassification between these codes. We did the same for cancer of cervix and uterus. We also aggregated cancers of the mouth, pharynx and oesophagus together with chronic liver disease and alcohol abuse as “alcohol related mortality”. This choice is opportunistic, including non-alcohol related mortality but excluding the many alcohol related accidents and suicides. Age standardised rates for ages 0–64 years have been calculated using the WHO European population as direct standard. Confidence limits for standardised rates were small and have been omitted.
Regional life tables are cruder than national life tables: they have been calculated by mortality in 5 year age groups and with 85 + as open ended age group. At the national level decomposition life tables have been calculated by single year age groups. The decomposition life table shows the consequences for life expectancy of increased mortality by age and cause of death in the NMS, compared to the EU-15 [10]. More details can be found elsewhere[11]. Data were incomplete for Belgium, Italy, Denmark and Sweden (EU 15) and for Cyprus, the Czech and Slovak Republic. The decomposition life table therefore considers Austria, Germany, Spain, Finland, France, Greece, Ireland, Luxemburg, Netherlands, Portugal and the United Kingdom as representative for the EU-15; Bulgaria, Estonia, Hungary, Lithuania, Latvia, Malta, Poland, Romania and Slovenia as representative for the NMS.
Decomposition life tables contribute changes in mortality by age and cause to changes in life expectancy. The Arriaga method, named for it’s author, estimates the contribution of a changes in a specific cause of death at a specific age to changes in life expectancy [10].
Gini coefficients assess those causes of death with the highest variability (http://en.wikipedia.org/wiki/Gini_coefficient). We used the Gini coefficient as a measure of inequality between causes of mortality (0–64 year) in the European regions. The Gini coefficient plots the cumulative share of mortality of each region, from small to large. The coefficient is then the surface between the resulting line and the straight line of perfect equality. With perfect equality, the Gini coefficient is zero. With perfect inequality, all the mortality is in one region, the others are zero and the Gini coefficient is 1. A higher Gini coefficient indicates a more unequal distribution.
Results
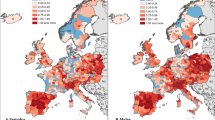
All cause mortality
Life expectancy in the EU-27 was 75.1 years (men) and 81.3 years (women). The difference in life expectancy at birth between the 10th and 90th percentile was 8.0 (men) and 5.6 years (women). Figure 1 shows the total life expectancy by region, Fig. 2 by country and sex.
Life expectancies at birth by the 27 EU and 3 EFTA members, ranked by total life expectancy. Belgium represented by Flanders only. † Data represent life expectancy of 66.9% of the Bulgarian population. Two regions omitted with life expectancy 11.0 and 9.1 years higher than the other four. ‡ Data represent life expectancy of 84.5% of the Romanian population. One region omitted with life expectancy 8.9 years higher than the other seven
Life expectancy in men was 76.4 (EU 15) and 70.3 (NMS), a difference of 6.1 years. Life expectancy in women was 82.1 (EU 15) and 78.2 (NMS), a difference of 3.9 years. Low life expectancy is associated with large gender gaps, caused by high male mortality. Iceland and Switzerland, both EFTA countries, took the lead in life expectancy in 2002–2004, with average life expectancies of 81 years, men and women combined. Italy, Spain and Sweden had life expectancies of more than 80. Of the ten NMS, six did not reach 70 years for male life expectancy. In one rural region of Bulgaria and one rural region in Romania, life expectancy is 9 higher than for the rest of Bulgaria or Romania (see Fig. 1). In another region, it is 11 years higher. We hypothesised this to be caused by lack of birth certificates, a relic of a turbulent history before and during the first world war, and eliminated these regions from Bulgaria (33.1% of the population) and Romania (15.5% of the population). Life expectancy dropped with 2.1 year in the remaining regions of Bulgaria and 0.9 year in those of Romania. Bulgaria has then the lowest life expectancy in the four remaining regions of six, preceded by Romania in the remaining seven regions of eight. Then the three Baltic States (Estland, Letland and Lithuania) follow with lowest life expectancies.
In the cause decomposition life tables (see Fig. 4), 60% of the difference in male life expectancy between EU 27 and the new MS could be explained by mortality under age 65. Among women, this was one-third. All cause mortality before age 65 shows large differences between high mortality and low mortality regions. In the highest decile men and women die at a 2.5 (men) and 1.9 (women) higher rate than at the lowest (see Tables 2, 3). In the NMS, age standardised mortality is 2.0 (men) and 1.5 (women) higher than in the EU 15, indicating that most of the variance is between NMS and EU 15.
The most important variability is in ill defined causes, warning against overinterpretation of cause of death data from different countries. Ill defined mortality is 14 times higher in the 90th than in the 10th percentile (see Tables 2, 3). The large difference between mean and median (50th percentile) indicates a skewed distribution with regions scoring very high. The absolute difference between 10th and 90th percentile is larger than or close to the fifth largest ICD chapter. Figure 3 shows the potential effect of misclassification by combining age standardised rates (ASR; 0–64 years) of ill defined with cardiovascular mortality, the largest cause of death. France is second in low cardiovascular mortality, but tenth in low cardiovascular mortality and ill defined causes combined. Countries that drop three place or more in the ranking of cardiovascular with ill defined countries combined are France (8 places), Portugal and Norway (4 places) and the Netherlands (3 places). Countries that mount three places or more are the UK (4 places) and Iceland (3 places) and Austria (3 places). The Netherlands is 6 places before the UK in cardiovascular mortality, but behind the UK if cardiovascular mortality is combined with ill defined causes.
Cancer mortality is the first cause of death in the 0–64 year old, but the absolute difference between high and low mortality regions is highest in circulatory diseases (chapters) and ischemic heart disease (individual diseases; Tables 2, 3). The same holds for the difference between EU-15 and NMS. Among men (Table 2), the absolute difference between NMS and EU 15 in injury related mortality is still higher than that among cancer. In the individual diseases, the absolute differences between EU15 and NMS are highest in ischemic heart disease, stroke, alcohol related mortality (dominated by chronic liver disease) and lung cancer. Mortality is twice as high in the NMS as in the EU 15 for four of the five major disease chapters, except for cancer. Relative disparities were highest for mortality from digestive diseases. In the individual disease groups, stroke stands out among men. A high mortality region at the 90th decile has a five fold risk of death from stroke, compared to a low mortality region at the 10th decile. Large relative differences for most important diseases in all regions suggest a large potential for prevention and improved health in the EU.
Among women, absolute differences are smaller as the absolute level of mortality is smaller. The highest absolute differences are found in ischemic heart disease, lung cancer, alcohol related mortality and stroke. The largest relative differences are found again in all heart diseases and stroke. Breast cancer is a notable outlier in this list, with very high mortality but limited differences in mortality between regions and no mortality differential between the EU 15 and the NMS. This suggests limited impact of prevention programmes. Differences observed are mainly due to differences in quality of treatment rather than changes in lifestyle risk factors or the result of screening programs [6]. At the other hand, cervical cancer shows more variance between high and low mortality countries. At lower ages, death from cervical cancer is more frequent and from uterus cancer is more rare, suggesting that these differences are explained by differences in cervical cancer death [2]. Here, effective cervical cancer screening programmes explain part of the observed mortality differential between high and low mortality countries [2].
The cause elimination life tables show the considerable loss of life, caused by earlier mortality. Among men, 4.0 years of life expectancy are lost by mortality before age 65, or 59.4% of the difference in total life expectancy between EU 15 and NMS (6.7 years, less countries participated in the cause elimination life tables, causing slight differences in differences in total life expectancy; See Fig. 4). Among women, this is 1.5 years of the 4.5, or 33.7%. Among men, high cardiovascular disease mortality (age 0–64) in the NMS caused a loss of life expectancy of 1.6 years (0.6 for IHD, 0.4 for stroke and 0.5 for the rest). Among women, this is more or less half, again evenly distributed over IHD, stroke and the rest. Among men, differences in cancer mortality (age 0–64) cause 0.69 life years, of which 0.44 years are due to smoking related cancers, predominantly lung cancer. Among women, differences in cancer cause 0.51 life years, of which 0.15 years are due to cervical/uterus cancers. Injury related mortality (age 0–64) causes 1.01 years more loss of life expectancy among men of the NMS, 0.21 years by traffic accidents and 0.20 by suicide but another large 0.6 years by a rest group of other injuries, mostly covered by other accidents. Among women of the NMS, injury related mortality caused less loss of life expectancy, some 0.22 year, mainly by other accidents (0.15 year) and traffic accidents (0.7 years). Among men of the NMS, alcohol related mortality before age 65 claimed 0.26 more among men, compared to the EU 15 and 0.09 years among men.
a Loss of life expectancy by age and aggregated cause of death, EU 15 compared to new member states (NMS; see “Methods” for countries included, at age 75 and older causes of death aggregated), women. b Loss of life expectancy by age and aggregated cause of death, EU 15 compared to new member states (NMS; see “Methods” for countries included, at age 75 and older causes of death aggregated), men
Table 4 shows the codes of death with the largest regional inequalities in Europe. Tuberculosis and HIV-AIDS reflect the patchy nature of infectious disease epidemics. Eastern Europe suffers from a severe epidemic of tuberculosis and multi resistant tuberculosis [12–15]: Poisoning, suicide, alcohol abuse, other causes of toxicomania, pneumonia, ill defined conditions and homicide are all linked to alcohol abuse, drug use, social isolation and homelessness. Unequal mortality from cervical and uterine cancer is dominated by higher cervical cancer mortality among the younger, suggesting possibilities for improved cancer control [2]. Stomach ulcus mortality may be linked again to alcohol misuse and lower access to good quality health care.
Discussion and conclusions
The health divides in Europe are large. Particularly men are heavily burdened by high mortality. Differences between NMS and EU 15 show very large preventable burdens of ischemic heart disease, stroke, other heart diseases, smoking related cancers, injuries and alcohol related mortality.
This article tries to present the available data in the most succinct way possible. The primary aim is descriptive. As numbers are large and these data are not samples, random error was irrelevant. The main problem is in the reliability and comparability of the data. In three regions of Bulgaria and Romania life expectancy was unrealistically high, compared with the other regions. Exclusion shifted national life expectancy of Bulgaria and Romania to the last places in the EU rankings. We can not exclude that these outlying regional life expectancies may be true, but Bulgaria has then the region with the lowest life expectancy of the EU (65.9 year) and a region at the third percentile of the EU (81.2 year), a difference of 15.3 years in adjacent regions (see Fig. 1).
Comparable cause of death certification is even more difficult. At ages under 65, death by many competing causes from elderly frailty should be rare. Nevertheless, we observe large differences in Europe between ill coded causes of death. Among men, ill defined causes of death would be seventh in the disease list. Total mortality varies 2.5 and 1.9 fold between extreme deciles, but ill defined mortality varies 14- to 15-fold. Ill defined causes have many causes: sudden death (often circulatory and cardiac from origin) [16], death in socially isolated people without a medical record [5, 17–19], migrants who return to their home country for dying [20, 21], or causes of death that are socially undesirable such as suicide or HIV-AIDS, either for financial or cultural reasons [5]. However, these factors can hardly explain such differences. While EUROSTAT wanted to focus on harmonisation of these codes [22], specific training on certifying procedures are insufficient if the registering medical doctor is not motivated [23]. Medical doctors should be made aware that death certification is a fundamental requirement for building up epidemiological data [23]. However, as shown, the disease specific patterns observed are consistent with more elaborated analyses of disease specific causes [2–8, 15, 24].
The data suggest that in Europe, health inequities are caused by the very traditional causes of poor health: smoking, excessive alcohol consumption, mortality from injury and suicide and deficiencies in access of health care. Injury mortality and suicide speak for themselves, although the importance of accidents other than traffic accidents and suicide, also among younger persons, was surprising. Differences in smoking related cancers highlight historical differences in smoking intensity.[25] Alcohol related mortality is but a crude proxy of the detrimental health effects of excessive alcohol use, but these crude mortality statistics are supported by more refined analyses of alcohol use in Eastern Europe.[7] Low levels of social support, lack of control over one’s life, material hardship, combined with a culture that approves of smoking and excessive drinking are underlying causes.[12] Access to health care is exemplified by large differences in cervical cancer mortality [2], but also the large differences in cardiovascular heart disease suggest large possibilities for improved control. Classic coronary risk factors are amenable by preventive interventions, smoking cessation therapies, blood pressure lowering and cholesterol lowering statins. The acute fatality of myocardial infarctions, the single most important cause of death, is vulnerable to effective coronary care [26, 27]. Variability of certain causes of death such as tuberculosis and HIV point to local epidemics or to the severe epidemic of tuberculosis in Eastern Europe.
The NMS can learn from the experience of the EU15 countries, in lowering accident mortality and smoking related mortality, where great advances have been made. Improving the health care sector, particularly in primary health care and in urgency care, should be able to control ischaemic heart disease, related heart disease and stroke, lower injury mortality and lower cervical cancer death by improved screening policies.
As the health policy targets are clear, well defined and vulnerable to public health policy: closing the health gap is a major target of the European Union [28]. This process can be monitored by regional vital statistics, as the main compass of public health. However, to do this, Europe will need a major effort of unification of its registers, directed both at the grassroots levels of the doctor registering the cause of death and at the regional statistical offices.
Key points
This paper present a comprehensive update of European mortality in the European Union in 2002–2004.
Comparability of causes of death is moderate. Europe needs an effort of more reliable declaration and standardisation of registered cause of death.
Large mortality differentials are dominated by avoidable causes at younger ages: smoking, alcohol, diseases related to diet and a sedentary lifestyle, unsafe roads and less well performing health care systems.
Closing the health gap is feasible and a major target of the European Union.
Abbreviations
- EFTA:
-
The European free trade association, European states not member of the EU. Members are Iceland, Norway, Switzerland, and Liechtenstein
- EU-27:
-
The European Union since 2007, with 27 member states
- EU-15:
-
The European Union before 2004, with 15 states: Austria, Belgium, Denmark, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden, United Kingdom
- EUROSTAT:
-
The statistics office of the European Commission, producing data for the European Union
- NMS:
-
New Member States, the 12 states that joined since 2004: Bulgaria, Cyprus, Czech Republic, Estonia, Hungary, Latvia, Lithuania, Malta, Poland, Romania, Slovakia, Slovenia
- NUTS-2:
-
Nomenclature of Territorial Units for Statistics, second level (see http://ec.europa.eu/eurostat/ramon/nuts/basicnuts_regions_en.html). NUTS subdivides each EU Member State into NUTS 1 regions, each of which is in turn subdivided into a whole number of NUTS 2 regions. NUTS-2 corresponds to provinces in most countries
References
Health Statistics. Atlas on mortality in the European Union: Data 1994–96. Luxembourg: Office for Official Publications of the European Communities; 2002.
Arbyn M, Raifu AO, Autier P, et al. Burden of cervical cancer in Europe: estimates for 2004. Ann Oncol. 2007;18:1708–15.
Boyle P, Ferlay J. Cancer incidence and mortality in Europe, 2004. Ann Oncol. 2005;16:481–8.
Muller-Nordhorn J, Binting S, Roll S, et al. An update on regional variation in cardiovascular mortality within Europe. Eur Heart J. 2008;29:1316–26.
Chishti P, Stone DH, Corcoran P, et al. Suicide mortality in the European Union. Eur J Public Health. 2003;13:108–14.
Tyczynski JE, Plesko I, Aareleid T, et al. Breast cancer mortality patterns and time trends in 10 new EU member states: mortality declining in young women, but still increasing in the elderly. Int J Cancer. 2004;112:1056–64.
Rehm J, Sulkowska U, Manczuk M, et al. Alcohol accounts for a high proportion of premature mortality in central and Eastern Europe. Int J Epidemiol. 2007;36:458–67.
Hamers FF, Infuso A, Alix J, et al. Current situation and regional perspective on HIV/AIDS surveillance in Europe. JAIDS. 2003;32:S39–48.
Shaw M, Orford S, Brimblecombe N, et al. Widening inequality in mortality between 160 regions of 15 European countries in the early 1990 s. Soc Sci Med. 2000;50:1047–58.
Arriaga EE. Measuring and explaining the change in life expectancies. Demography. 1984;21:83–96.
de Beer J, Bonneux L, Huisman C, et al. Decomposition of life expectancy changes by cause of death. In: Report commissioned by EUROSTAT. Netherlands Interdisciplinary Demographic Institute (NIDI) and Population Research Centre Groningen: The Hague; 2008.
Mackenbach JP, Stirbu I, Roskam A-JR, et al. Socioeconomic inequalities in health in 22 European Countries. N Engl J Med. 2008;358:2468–81.
Enserink M. European expansion. Outwitting TB on the E.U’.s eastern frontier. Science. 2004;304:199.
Odigwe C. Drug resistant tuberculosis soars in eastern Europe. BMJ. 2004;328:663.
Surendran A. AIDS, TB hit Eastern Europe. Nat Med. 2004;10:323.
Armstrong DL, Wing SB, Tyroler HA. United States mortality from ill-defined causes, 1968–1988: potential effects on heart disease mortality trends. Int J Epidemiol. 1995;24:522–7.
Andreev E, Pridemore WA, Shkolnikov VM, et al. An investigation of the growing number of deaths of unidentified people in Russia. Eur J Public Health. 2008;18:252–7.
Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331:304–9.
Hawton K, Harriss L, Zahl D. Deaths from all causes in a long-term follow-up study of 11, 583 deliberate self-harm patients. Psychol Med. 2006;36:397–405.
Bos V, Kunst AE, Keij-Deerenberg IM, et al. Ethnic inequalities in age- and cause-specific mortality in The Netherlands. Int J Epidemiol. 2004;33:1112–9.
Bijlsma F. Mortality among young people: causes and background. Ned Tijdschr Geneeskd. 1994;138:2439–43.
Jougla E, Pavillon G, Rossollin F, et al. Improvement of the quality and comparability of causes-of-death statistics inside the European Community. EUROSTAT Task Force on “causes of death statistics”. Rev Epidemiol Sante Publique. 1998;46:447–56.
D’Amico M, Agozzino E, Biagino A, et al. Ill-defined and multiple causes on death certificates—a study of misclassification in mortality statistics. Eur J Epidemiol. 1999;15:141–8.
Muller-Nordhorn J, Rossnagel K, Mey W, et al. Regional variation and time trends in mortality from ischaemic heart disease: East and West Germany 10 years after reunification. J Epidemiol Community Health. 2004;58:481–5.
Peto R, Lopez AD, Boreham J, et al. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–78.
Van Brabandt H, Camberlin C, Vrijens F, et al. More is not better in the early care of acute myocardial infarction: a prospective cohort analysis on administrative databases. Eur Heart J. 2006;27:2649–54.
Peeters A, Bonneux L, Barendregt JJ, et al. Improvements in treatment of coronary heart disease and cessation of stroke mortality rate decline. Stroke. 2003;34:1610–4.
World Health Organisation/Europe. The European health report 2005. Copenhagen: Public health action for healthier children and populations; 2005.
Acknowledgments
This research has been funded by contract number 35100.2005.001-2006.703, commissioned by EUROSTAT. The data have been forwarded by Eurostat as part of this contract. The CD with data and results is available on request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonneux, L.G., Huisman, C.C. & de Beer, J.A. Mortality in 272 European regions, 2002–2004. An update. Eur J Epidemiol 25, 77–85 (2010). https://doi.org/10.1007/s10654-009-9415-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-009-9415-y