Abstract
Concepts describing secondary trauma phenomena do not adequately capture the profound impact that collective catastrophic events can have on mental health professionals living and working in traumatogenic environments. Shared trauma, by contrast, contains aspects of primary and secondary trauma, and more accurately describes the extraordinary experiences of clinicians exposed to the same community trauma as their clients. Case vignettes from clinicians in Manhattan and Sderot, Israel are provided to illustrate the transformative changes that clinicians may undergo as a result of dual exposure to trauma. Discussion involves the importance of articulating one’s own trauma narrative and attending to self-care prior to resuming clinical work, as well as opportunities for enhanced therapeutic intimacy and caution regarding boundary alterations that may result from clinician self-disclosure. Agency settings can provide the necessary education, supervision, and support to mitigate the negative effects of shared trauma.
Similar content being viewed by others
Introduction
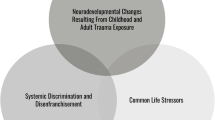
With the escalation of climate change and world-wide terrorism, and the concomitant increase in man-made and natural disasters, social workers and other mental health clinicians may find themselves exposed to and practicing in environments that could be characterized as traumatogenic. There are many examples of such environments, including areas that are host to tsunamis, cyclones, hurricanes, tornadoes, earthquakes, floods, bushfires, and volcanic activity, as well as those regions that are prone to chronic acts of terrorism. People subjected to catastrophic environmental events may find themselves impacted simultaneously on multiple levels—intrapsychic, interpersonal, and community—leading to potential alterations of their self-perception and worldviews.
While secondary trauma concepts help clinicians understand their reactions to the clients’ trauma narratives, none describe the entirety of the clinician’s experience when living and practicing in traumatogenic environments. Following the September 11th disaster there was call for a more exacting construct to capture the experience of mental health professionals striving to provide effective client services while addressing the same issue in their personal lives (Eidelson et al. 2003). Subsequently, the term shared trauma (Altman and Davies 2002; Saakvitne 2002; Tosone and Bialkin 2003; Tosone et al. 2003; Tosone 2006) was introduced into the professional literature to describe narrative accounts of clinicians exposed to the same collective trauma as their clients.
This paper defines shared trauma in relation to existing secondary trauma constructs, and describes the impact on the therapeutic situation, as well as the professional and personal alterations that may result from the clinician’s dual exposure to trauma. Agency-based case examples from Israel and Manhattan will be used to illustrate the transformative changes that clinicians may undergo under these circumstances. Recommendations for enhancing practice will be addressed, as will the important role agencies can play in enhancing the clinician’s performance in these environments.
Review of the Literature
The ramifications of working with trauma survivors has been variously described using several well-known concepts, including vicarious traumatization (McCann and Pearlman 1990; Pearlman and MacIan 1995; Pearlman and Saakvitne 1995), compassion fatigue (Figley 1995, 2002), secondary traumatic stress (Stamm 2002), and burnout (Leiter and Maslach 1988). Although these constructs have been compared and debated in the professional research literature, methodological limitations and contradictory results have necessitated additional conceptual and measurement clarity (Sabin-Farrell and Turpin 2003; Boscarino et al. 2004).
The first of these terms, burnout, describes a gradual, pathological process whereby symptoms of emotional exhaustion can develop due to the psychological strain of working with multiple stressors. These symptoms may include depression, cynicism, boredom, loss of compassion, erosion of idealism, and a reduced sense of professional accomplishment and commitment to the profession (Leiter and Maslach 1988).
Figley (1995) offered the term compassion fatigue to describe the long-term cumulative stress resulting from the “cost of caring.” As proposed, compassion fatigue was a broad term intended to encompass burnout, in addition to emotional contagion and secondary victimization (Figley 1995). He articulated a comprehensive description of the cognitive, emotional, behavioral, spiritual, and somatic symptoms that can manifest themselves in compassion fatigue, as well as ways in which it can negatively influence one’s personal relations and work performance.
Secondary traumatic stress, by contrast, can occur suddenly and is directly related to the client’s experience of trauma, and not to cumulative professional stress per se. Secondary trauma symptoms are akin to those of posttraumatic stress, and involve anxiety, depression, avoidance, and hyper-arousal. These symptoms are in response to the client’s trauma narrative, and the clinician’s reaction may mirror that of the client. Highly empathic and neophyte clinicians are more prone to the development of secondary traumatic stress than are seasoned mental health professionals (Stamm 1995).
Vicarious trauma, like secondary traumatic stress, occurs in the context of work with trauma survivors, but is not considered a pathological process as is secondary traumatic stress. The emphasis is on the cognitive and emotional transformations that occur as a result of empathic engagement with trauma survivors. As with secondary traumatic stress, these changes are most pronounced in highly empathic and neophyte therapists, as well as in clinicians with a previous trauma history. These changes take place in the totality of the therapist’s life, and include permanent alterations in one’s self-concept and worldview (Pearlman and Saakvitne 1995).
Other trauma-related clinician responses have been described under the rubric of countertransference. As commonly defined, countertransference refers to the affective and behavioral reactions of the clinician to the client, whether conscious or unconscious. The contemporary definition of countertransference includes both objective and subjective components; that is, it contains personal, subjective reactions of the clinician to the client as well as diagnostic, objective ones in which the clinician responds in accord with the client’s provocations (Boulanger 2007). Whereas vicarious traumatization and related concepts describe the short and long-term impact of hearing traumatic material on the entirety of the clinician’s life, countertransference is confined to the therapeutic setting. A critical point is that, although a frequent occurrence in treatment, countertransference reactions may not necessarily be of a traumatic nature. Those that are have been termed traumatic countertransference (Herman 1992) and traumatic reenactments (Davies 1996; Boulanger 2007).
To summarize, while these clinician-related terms are often used interchangeably, each presents a nuanced understanding of the clinician’s reaction to working with clients. Burnout is an early generic term, used in relation to all types of direct practice experience, whereas compassion fatigue, secondary trauma, and vicarious trauma are concepts used solely in relation to trauma work. Although secondary trauma is the umbrella term used to encompass these three related constructs, it is case-specific. Vicarious trauma and compassion fatigue, by contrast, can manifest in reaction to a particular case, but are generally cumulative reactions to working with trauma survivors. While compassion fatigue is not related to a specific theoretical orientation, vicarious trauma is associated with constructivist self-development theory and refers to permanent alterations in one’s self and world views as a result of trauma work. As discussed previously, traumatic countertransference refers to a gamut of induced clinician reactions taking place in treatment with a traumatized client.
The Relational Nature of Trauma
Traumatic reenactments take place in treatment and result from aspects of the client’s and clinician’s internal worlds that influence the transference-countertransference interaction. As a result of their unique interaction, the client and clinician develop a fuller, co-constructed understanding of the impact of trauma on their therapeutic relationship. Traumatized patients tend to elicit strong and often polarizing countertransference responses, unconsciously inducing their therapists into a reenactment of their ordeal (Courtois 2010). For instance, clinicians treating survivors of sexual abuse may find themselves experiencing a host of disturbing emotions such as guilt, arousal toward the client, and anger toward the perpetrator. The term countertransference is frequently but mistakenly used interchangeably to describe secondary trauma-related phenomena, the distinction being that countertransference is confined to the clinician’s affective responses to the client in the therapeutic setting while secondary trauma has implications for and manifestations in the clinician’s personal life.
The relational nature of trauma presupposes that each therapeutic dyad is capable of a distinct interaction based on the participants’ intrapsychic and interpersonal psychodynamics and trauma histories. As the pair works toward understanding the patient’s symptomotology, the clinician also has the opportunity for intrapsychic and interpersonal growth as each engage in their respective therapeutic reveries resulting from the interaction. A clinician, deeming her reaction as objective countertransference, may selectively disclose her affective response in an effort to help the client. Since her response is also influenced by personal experiences, it becomes essential for the clinician to be able to discern the nature of the reaction. Is it based primarily on a reaction to the client’s provocation, her own experience, or a combination of the two?
When the clinician and client share a personal traumatic experience, such as having been sexually abused in childhood, there may be opportunity for mutual reparation and growth but also boundary confusion. For example, the clinician, whether or not disclosing her own childhood trauma, may mistakenly assume she understands the client’s reactions based on her own personal experience. It is incumbent upon the clinician to ensure that her selective self-disclosure is in service of the client’s best therapeutic interests, not personal need. Self-disclosure is an optional intervention. When the clinician and client are exposed to the same collective trauma, however, self-disclosure may be a moot point as the client is aware of the clinician’s exposure to the community-based disaster.
Shared Trauma: A New Construct for Challenging Times
Although clinicians have been living and working in the same communities as their clients since the inception of the social work profession, the term shared trauma was only recently introduced in response to the 9/11 disaster. Shared trauma, also referred to as shared traumatic reality, is defined as the affective, behavioral, cognitive, spiritual, and multi-modal responses that clinicians experience as a result of dual exposure to the same collective trauma as their clients. Like vicarious traumatization, these reactions have the potential to lead to permanent alterations in the clinician’s existing mental schema and world-view, the difference being that having experienced the trauma primarily, these therapists are potentially more susceptible to posttraumatic stress, the blurring of professional and personal boundaries, and increased self-disclosure. Additionally, the symptomotology of shared trauma and compassion fatigue are synonymous, but shared trauma symptoms are attributed to the dual nature of the exposure (Tosone in press). The use of the term, shared trauma, however, does not imply that the clinician’s trauma response is identical to that of the client; clinicians and clients can be variably impacted by the same simultaneous event. Although this paper focuses on large-scale collective traumas, it is important to emphasize that the shared trauma concept can also be applied to local events of a traumatic nature, such as recent school shootings.
In a special issue devoted to psychoanalytic practice in the wake of 9/11, Altman and Davies (2002) and Saakvitne (2002) describe these varying responses. Although exposed to the same “shared trauma”, their narrative accounts of and responses to the disaster differed from those of their patients. Saakvitne noted that dual exposure to trauma could lead to unique stresses and to symptoms of vicarious traumatization. Tosone et al. (2003) also employed the term to describe the impact of 9/11 on students’ personal and professional lives. Student reactions varied from a preoccupation for safety and an inability to focus on clinical work to finding a deep sense of professional purpose as a result of the disaster. Several reported concern that their increased self-disclosure with clients was inappropriate while others appreciated the enhanced therapeutic intimacy.
In an effort to provide empirical validation of the construct, Tosone et al. (2011) examined a variety of risk factors associated with posttraumatic stress and secondary trauma in relation to shared traumatic stress, a supraordinate construct reflecting the dual exposure to trauma. They studied 481 social work clinicians living and working in Manhattan and found that insecure attachment, greater exposure to traumatic life events in general and 9/11 in particular, and enduring distress related to 9/11 was predictive of higher levels of shared traumatic stress. Resilience was also found to be a mediator between the relationships between insecure attachments, traumatic life events and shared traumatic stress. In a related qualitative study, Bauwens and Tosone (2010) found several common themes, including 9/11 serving as the impetus for enhancing clinical skills and self-care, as well as increased compassion and connectivity to clients. Negative themes included an increased sense of personal vulnerability, feeling unprepared to work in a traumatogenic environment, and disappointment in the response of professional organizations. Seeley (2008), also studying psychotherapists post 9/11, found that subjects reported experiences of emotional contagion and strong identifications with patients impacted directly by the disaster.
Although the term shared trauma was first used in relation to the 9/11 disaster, Baum (2010) traces the phenomenon back to a brief report by Schmideberg, a psychoanalyst during the World War II London Blitz. Schmideberg (1942) described the impact that the prolonged bombing had on her personally and on her psychotherapeutic work with clients. Baum notes that it was not until the 1991 Gulf War that the phenomenon was named using the terms shared traumatic reality and shared reality, both of which underscore the interaction of the clinician’s inner and outer realities in response to client work undertaken in the context of a communal disaster.
The term shared traumatic reality has garnered the most interest in Israel where its citizens are chronically exposed to terrorist attacks, particularly in Sderot and areas bordering the Gaza Strip (Nuttmann-Shwartz and Dekel 2009; Dekel and Baum 2009; Shamai and Ron 2009). According to Baum (2010), shared traumatic reality entails several key aspects, including that it is (1) a current, collective event, (2) the clinician and client belong to the same community, and (3) the clinician suffers from the double exposure of being a citizen of the region and working work individuals in the same community. With the exception of shared traumatic reality involving a current catastrophic event, it is similar to shared trauma in all other aspects.
Clinician Narratives from New York City and Sderot, Israel
Depending on the nature, intensity, extensiveness, and time frame of the shared trauma, the clinician can respond professionally and personally in myriad ways, with each arena impacting the other. The following narratives, written in the first person, illustrate the complexity of a dual perspective and the inherent distinctions between shared trauma and shared traumatic reality. The first shared trauma narrative is written by a Manhattan social work clinician (TS) who was a social work intern on 9/11/01 and later went on to work exclusively with survivors of the event; the second is written by a seasoned academic clinician (ON) in Sderot who, along with her students and clients, has been subject for years to Quassam rockets on a sporadic, unpredictable basis.
Shared Trauma: An Example from the World Trade Center Disaster
Lifton (2005) introduced the idea that in shared traumatic events such as the attacks of 09/11/2001 and the ensuing wars in Iraq and Afghanistan there are two separate groups of survivors: the immediate survivors (victims and combatants) and distant survivors (those who bear witness). My experience on 9/11/2001 placed me firmly in and between both groups simultaneously. As an evacuee I faced my own symptoms of acute stress reaction and as a social work intern I faced the challenge of working in a post 9/11 reality.
Personal Narrative
In September 2001 I was in the last year of the 1 year residency program of NYU’s MSW program and had started my internship at a community based mental health clinic. At 8:20 a.m. on the morning of September 11th, 2001 I was sitting at my desk checking emails and preparing for the day ahead. My office was located on the 98th floor of 2 World Trade Center. Our department manager, F, stayed behind to evacuate the floor. We would learn later that he and another colleague who remained with him died in the attacks. I evacuated along with my colleague V to the ground floor of the building, ignoring announcements along the way telling us to return to our desks.
On the ground floor there were emergency workers frantically trying to usher people out of the building. V and I stayed together as we went to the exit close to Cortland Street. V and I became separated as we exited the building. There were loud disorienting noises, things falling everywhere, paper, metal and small shards of glass. What was most overwhelming was the sound the building made as it swelled and buckled under the intense heat. I remember looking up and seeing the flames and not quite understanding how the flames from 1 WTC could have engulfed the top floors of 2 WTC. I had no idea a second plane had struck. I jumped into the back of a florist’s truck for safety and recall hearing a woman scream at the top of her lungs. I was frightened for her and looked around only to realize I was alone and the woman screaming was me. I recall looking up from the truck and thinking “I will die if I stay here … those buildings will come down and I will die.” I ran and the kindest police officer helped me run to safety.
I, like many New Yorkers, evacuated across the Brooklyn Bridge that day where I learned that there was nothing accidental about what had taken place. I had located another colleague and we walked together trying to process what was taking place. As we got to the Brooklyn side of the bridge we turned to look at the two smoldering towers and in that moment 2 WTC collapsed before our eyes. The building that I had been in no more than an hour before vanished into a pile of rubble and I thought “they are all gone … anyone left in those towers surely died.”
Getting Help
The great detail in which I am able to relate my 09/11 experience is only possible after many years of restorative work with an extremely talented clinician. I can recall my early months in treatment starting in October of 2001 when I experienced an incredibly insulated dissociation where I would arrive at my therapist’s office and not quite recall my route there. The literature on acute stress reaction and posttraumatic stress disorder is filled with descriptions of these types of dissociative experiences among trauma survivors (Boulanger 2007; Meichenbaum 1994; Van Der Kolk and Saporta 1991). At other times I was assaulted by intrusive thoughts and persistent fears that somehow I would be killed by a car jumping the curb. I was terrified to walk around the city. Like other New Yorkers, my post 9/11 world consisted of heightened terror alerts and anthrax scares. The nightmares began and the mood swings left me feeling helpless. Thankfully, I had landed in the safest place that I needed to be at that time, in a treatment room, where no matter how bizarre my fears were I was safe to explore their meaning and not be made to feel awkward or judged.
Working with World Trade Center Workers and Volunteers
From 2004 to 2008 I worked at a World Trade Center Mental Health Intervention Program (WTC-MHIP), an outpatient hospital setting devoted to the treatment of workers and victims of the 9/11 disaster. My decision to move to this new department was based on careful examination of my preparedness to handle work that was so closely related to my experience on 09/11. Cognizant of the warnings about the “wounded practitioners” who practice in an effort to heal their own wounds (Faust et al. 2008), I had been working in my own treatment through this decision and made it, confident that I could bring an added value to my work with that population. I was not naïve in this decision and soon garnered additional supports including: returning to school for formal education in advanced clinical practice; securing the guidance of a private supervisor; taking advantage of both formal and informal sources of support available through the clinic; and maintaining an active social life and self-care regimen.
There are instances when a shared trauma can heighten and strengthen the therapeutic intimacy in the treatment, and this shared traumatic experience can be used in a positive transformative manner within the therapy. While there can also be a blurring of boundaries in these situations that can impede the work, it is also possible to harness these relational exchanges to benefit the treatment. In this situation the clinician no longer maintains a superior role but opens up a space, to the “intimate edge” what Ehrenberg (1992) described as the clinician being acutely aware of subtle changes that are happening in both the clinician and client.
My work with W exemplifies the transformative possibilities of shared trauma. W is a middle-aged emergency medical technician (EMT) who responded to the WTC on 9/11, and spent several months doing recovery work at the site. During the course of the time he spent at ground zero, W recovered the remains of a close colleague and was seriously traumatized by this event. Shortly after the 09/11 attacks he separated from his wife and children but moved to a nearby apartment to remain close to them. W reported irritability, a heightened startle response, significant insomnia, nightmares when he was able to sleep, and intrusive thoughts that often forced him to avoid being in enclosed spaces with others.
When I first met with this client I was struck by his physical posture in the session. He avoided eye contact, sat hunched forward with blunted affect throughout the sessions. His breath was shallow and uneven. I was sensitive to this physical presentation having seen it with numerous other clients and recognizing my own uneven breathing patterns from my experience with trauma. Although he was physically imposing, I got the sense that he was very afraid of this environment and had lost any trust in a predictable reality from the time he spent at ground zero. I introduced the use of deep breathing exercises instead of regular talk therapy early in the treatment since W was so easily provoked by verbalization of his experience, and often missed sessions after he spoke about his experience.
W was responsive to the guided imagery and breathing techniques, and I was relieved, as I wanted to help him reconstruct his life, something that could not occur if he fled treatment. After several sessions using this approach, W began to relax visibly and came to treatment on a consistent basis. As he shared his experience I understood more fully why he was afraid to talk. He recalled finding the remains of one of his colleagues and reported knowing in that instant that his whole world had changed. I understood the idea that in an instant your entire world-view and personal outlook can change. I wanted to cry, but most of all I wanted to expel from my mind the image of his recovering his friend’s remains. I understood with a familiarity and intimacy all too well how W felt about the images he carried with him from his experience. I too carried horrific images of 9/11, and of the people I worked with who were trapped in the burning tower.
Supervisory and Administrative Considerations
There was formal weekly supervision available to the therapists at WTC-MHIP, and while I made use of this resource, I found the most resonant support with my peers. After W disclosed the specifics of his experience, I found myself doing something uncharacteristic. Usually, I strive to be open and receptive to feedback. However, in this instance, I found myself hiding details of W’s narrative from my colleagues; they picked up on my avoidance and confronted me. McCann and Pearlman (1992) underscore the importance of the clinician having the forum to explore painful and disturbing counter-transferential emotions that arise in treatment with traumatized clients. They posit that this process of sharing in the right supportive environment can help to counteract the damaging effects of vicarious traumatization. In my peer support group I was re-enacting W’s avoidance because I did not want to damage my colleagues. Their insight, receptivity and support allowed me to survive the retelling of W’s and my trauma narratives, and interrupt the emotional numbing that would have resulted had I remained silent.
The clinic administration struggled to find ways to support a mental health staff that was conducting 9/11 related trauma work, and provided weekly supervision and case conferences in response to the express need. However, initially WTC-MHIP was treated as any other outpatient mental health clinic; therapists would screen daily between 7 and 10 workers and volunteers from the site, some of whom were presenting with immediate crises. The clinical team expressed concern that administration lacked a full understanding of the unique impact that trauma treatment can have on the provider.
While clinical staff evinced the signs of secondary trauma, including insomnia, increased fearfulness and reduced satisfaction, they were also dedicated to provide a high level of quality service and reported instances of personal growth from work with clients. These clinicians described their pride in helping clients to return to some form of normal functioning. Lev-Weisel et al. (2009) referenced the importance of providing high quality supervision and peer supervision as a means of protecting the clinician from vicarious traumatization and preserving their ability to continue work in the trauma field. It took several years and a change in administration for the clinical concerns to be communicated effectively, eventually resulting in an enhanced case presentation and peer supervision process, as well as providing opportunities for clinicians to write about their work. These were welcome changes for a dedicated clinical team that needed organizational support mechanisms to effectively continue their work.
Shared Traumatic Reality: A Personal View from a Social Work Clinician in a Traumatized Society
Since 2001, the southern region of Israel has been the target of Qassam rockets. Qassams are fired at all hours, and have introduced considerable uncertainty and anxiety into the lives of the area residents. Over the past 8 years, eighteen area residents have been killed, and several hundred have been wounded. In addition, over 3,000 residents of the area experienced high levels of distress and PTSD during the course of 2008, prior to the Cast Lead Operation. Notably, 26 % of the Sderot residents and less than 9 % of the residents of kibbutzim in the area have been diagnosed with PTSD (Dekel and Nuttman-Shwartz 2009). For a long period, those attacks did not arouse enough public sympathy. However, prolonged exposure to the threat of missile attacks has led to serious psychological and economic consequences, which have intensified considerably in recent years.
Seven years ago, I was asked to initiate a Department of Social Work at a college located near the Israeli border with the Palestinian Authority. Since then, I have served as head of the department, which currently has 300 students and 35 faculty members. It is the largest public community college in Israel, with a total enrollment of about 8,000 students in all of its programs.
Over the past 8 years, more than 5,000 missiles have fallen over the area, including our campus. Before Operation Cast Lead, the “red alert” siren would sound several times a day. At the sound of the siren, people hurry to a sheltered area, where they stay for about 15 seconds or so until they hear the explosion. Sometimes we feel as if we are in the middle of a battlefield. In fact, missiles have exploded inside the campus and destroyed one or more classrooms. Until the middle of 2006, the administration did not address the situation with the faculty and continued operating as usual when Qassam missiles fell on the college campus. In addition, after each Qassam attack, administrators would go out to survey the damage, flouting security regulations. Some lecturers would go on teaching, and delegitimize the students’ expectable reactions to the threat.
Personal Narrative
The day after one of our students, Roni I of blessed memory, was killed by a Qassam missile, I entered my office early in the morning as I do every day to find my room in shambles. Files and some books are on the floor, my desk is full of dust, and fragments of glass and plaster are spread across the room. I see the room filled with fragments from the window pane; all of the windows have been shattered. I try to breathe to calm myself as I think of what might have happened had I been in my office when the missile fell, the same missile that killed Roni. What if I hadn’t had enough time to run away, or hadn’t heard the siren? Taking another breath, I muster the courage to look out the window to see the large hole in the ground left by the Qassam rocket, right where Roni was killed. As a social worker, I assume that people need my help, and I shift my frame of mind to that of a helper. I organize faculty members from my department to screen the campus and reach out to students who might have experienced acute stress reactions.
Later, I understand what I have witnessed. I understand why I heard such heart-rending cries coming from the office the day before. Then we hear the “red alert” siren again, so my students and I run to the sheltered area (which doesn’t offer much shelter). I encourage the students to get away from the window when a loud boom occurs. The telephone falls, a lamp tips over, and there’s someone wounded at the gate. We enter into another state of emergency. Now we’re social workers in the field and not college faculty members—with all that this entails. One of my faculty members and I go to all of the classrooms, handing out water, candy, cookies, but most of all, encouragement and comfort. We send people for crisis counseling, hug students who are trembling with fear, laugh with others who tell us how important it is for them to dress well in case they have to be hospitalized. It’s a bizarre scene and the “red alert” siren sounds yet again. Afterwards, I met with college administrators and government officials, all of whom are unable to provide the necessary support and assurances of safety. I eventually go home, and feeling at a total loss, I sit at the computer and cry.
Working with Clients in a Shared Traumatic Reality: A Case Illustration
This event changed my relationships with my clients, especially P, a widowed Holocaust survivor in her 60s who arrived in Israel immediately following World War II. Out of necessity she was forced to be strong and independent, and perpetually prepared for danger. Fear and doubt were suppressed at all costs, but the recent death of her husband prevented her from assuming this stance. Our sessions took place in a community mental health agency in southern Israel. In sessions, she was preoccupied for my safety due to the escalation of tensions in Sderot, despite the fact that she lived in the nearby area. I was able to interpret her excessive concern for me as reflecting a concern for herself as well; that is, she cared for me in a way that went beyond her empathy for my situation. After the event described above, she called me at home to make sure I was safe. At our next meeting, I had difficulty continuing as usual, and unconsciously let her take care of me. She started asking questions about my feelings and fears. Surprising myself, I answered her questions without even noticing that we had changed roles. I felt comforted by her caring comments, yet also tried to help her see that it was a shared concern.
Following an insightful supervisory session, I allowed myself to admit that I needed a protective figure, something I had not found in the college environment. I also realized that I was afraid to discuss my fears with my family because I wanted to protect them and also myself from their fear that something terrible might happen to me. Eventually, I was able to connect emotionally to the effects of this critical event, and to the reality of ongoing exposure to missile threats. In situations involving shared traumatic reality, I readily moved into the behavioral and emotional position of a client. As a result of these dynamics, our roles were reversed: my client was in a position of power, and I was drawn into the role of a girl, a client. In that role, I was under the illusion that I was being protected, in contrast to the situation in the real world.
This countertransferential awareness helped me to return to the role of clinician. We were able to talk about the period when her husband was sick, and how she felt abandoned by his death. She now had to live in a state of terror alone, and was able to discuss her fears of being hit by a Quassam missile. Importantly, we were able to talk about the fact that we were residing in the same terror-filled environment, something that impacts our therapeutic relationship in an ongoing way. We are “in the same boat”—a situation that has been referred to as shared traumatic reality in Israel (Dekel and Nuttman-Shwartz 2009). After 8 years of Qassam rocket attacks, I have learned how to function under fire, despite my long-held illusion that the situation could be controlled.
My reactions helped me identify several responses similar to conceptualizations in the literature (Cunningham 2003), especially related to shared trauma (Tosone and Bialkin 2003) and shared traumatic reality (Dekel and Nuttman-Shwartz 2009). Specifically, I had difficulty establishing professional boundaries with my client, and identifying countertransference reactions from those of my client. With time, empathy, and a relational stance, both my client and I were better able to acknowledge our shared vulnerable state as a result of chronic exposure to terrorism. With regard to my personal life, I experienced a long period of tension, uneasiness, and emotional detachment. At the same time, I also felt a stronger sense of Israeli nationalism and Zionist identity. My priorities also changed; I devoted more time to leisure and social activities, and travelled abroad more.
Discussion
As the above examples illustrate, shared trauma affords clinicians the opportunity for personal and professional growth, as well as heightened intimacy in the therapeutic encounter. These transformative changes are possible for clinicians exposed to singular catastrophic events such as 9/11, as well as for those exposed in an ongoing way to terrorism. In both these examples, clinicians are deprived of the clinical distance usually afforded them by having a different set of external experiences than those of their clients. In this way, their affective, behavioral and cognitive responses differ from colleagues experiencing secondary trauma phenomena alone.
More specifically, the shared traumas illustrated here suggest unique elements: both clinicians identified with their clients and interventions were as much geared toward self-need as the perceived needs of their clients; both were keenly aware that their own dissociative and traumatic responses altered the nature of their relationships to their patients; both sought supervision as a forum to process their reactions to ensure that professional boundaries were reestablished; and both subsequently invested in developing aspects of their personal lives.
There were notable differences in their reactions as well. Having experienced 9/11 as a student clinician, TS did not have the same degree of responsibility as did OS, and was able to take full advantage of the opportunities for professional posttraumatic growth. OS, by contrast, felt the strain of performing multiple roles- professor, administrator, colleague, and clinician. She performed these multiple roles without the perceived support of the college administration while exposed to unpredictable acts of terrorism. These added stressors likely contributed to the enactment she found herself in with her client. OS was in need of comfort and support, and P needed to nurture. As Israeli citizens with a shared legacy of trauma, cultural imperatives helped to shape the nature of their relationship. In comparing the experiences of these clinicians, the differences between shared trauma and shared traumatic experiences become more pronounced.
In both these examples, social and professional support can make an important contribution to mitigate the negative effects of shared trauma. Clinicians exposed to collective trauma should be encouraged to access all available resources, including organizational ones. The perceived level of support available to clinicians from their professional and educational organizations, agency-based work settings, supervisors, and colleagues, coupled with the personal support they receive from family and friends, can influence the quality of their professional work.
Agency-based, private, and peer supervision, in particular, are essential sources of professional support. If these resources are lacking, clinicians should consider advocating for changes in their work settings, educational institutions and professional associations to make these organizations more responsive to the training needs of mental health professionals impacted by collective trauma.
Conclusion
Shared trauma and its variant, shared traumatic stress represent a clinician experience that differs from secondary trauma. Due to the dual nature of the trauma, clinicians may experience significant positive and negative changes in their personal and professional lives, including increased self-care, personal and therapeutic intimacy, self-disclosure, and permeability of professional boundaries. Personal and peer support, supervision, and additional training are critical components to mitigate the negative effects of shared trauma.
References
Altman, N., & Davies, J. M. (2002). Out of the blue: Reflections on shared trauma. Psychoanalytic Dialogues, 12(3), 359–360.
Baum, N. (2010). Shared traumatic reality in communal disasters: Toward a conceptualization. Psychotherapy Theory, Research, Practice, 47(2), 249–259.
Bauwens, J., & Tosone, C. (2010). Professional posttraumatic growth after a shared traumatic experience: Manhattan clinicians’ perspectives on post 9/11 practice. Journal of Loss and Trauma, 15(6), 498–517.
Boscarino, J. A., Figley, C. R., & Adams, R. E. (2004). Compassion fatigue following the September 11 terrorist attacks: A study of secondary trauma among New York City social workers. International Journal of Emergency Mental Health, 62, 57–66.
Boulanger, G. (2007). Wounded by reality: Understanding and treating adult onset trauma. NJ: Analytic Press.
Courtois, C. (2010). Healing the incest wound: Adult survivors in therapy (2nd ed.). New York: Norton.
Cunningham, M. (2003). Impact of trauma work on social work clinicians: Empirical findings. Social Work, 48, 451–459.
Davies, J. (1996). Linking the pre-analytic with the postclassical: Integration, dissociation, and the multiplicity of unconscious process. Contemporary Psychoanalysis, 32, 553–576.
Dekel, R., & Baum, N. (2009). Intervention in a shared traumatic reality: A new challenge for social workers. British Journal of Social Work, 32, 1–18.
Dekel, R., & Nuttman-Shwartz, O. (2009). PTSD and PTG following Qassam attacks: Correlations and contributors among development town and kibbutz residents. Health and Social Work, 34, 87–96.
Ehrenberg, D. (1992). The intimate edge. Hillsdale, NJ: The Analytic Press.
Eidelson, R. J., D’Alessio, G. R., & Eidelson, J. I. (2003). The impact of September 11 on psychologists. Professional Psychology: Research and Practice, 34(2), 144–150.
Faust, D., Black, F., Abrahams, J., & Warner, M. (2008). After the storm: Katrina’s impact on psychological practice in New Orleans. Professional Psychology: Research and Practice, 39(1), 1–6.
Figley, C. R. (Ed.). (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner Mazel.
Figley, C. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self-care. Journal of Clinical Psychology, 58(11), 1433–1441.
Herman, J. (1992). Trauma and Recovery. New York: Basic Books.
Leiter, M. P., & Maslach, C. (1988). The impact of interpersonal environment on burnout and organizational commitment. Journal of Organizational Behavior, 9, 297–308.
Lev-Weisel, R., Godblatt, H., Eisikovits, Z., & Admi, H. (2009). Growth in the shadow of war: The case of social workers and nurses working in a shared war reality. British Journal of Social Work, 39, 1154–1174.
Lifton, R. (2005). Americans as survivors. New England Journal of Medicine, 352(22), 2263–2265.
McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3(1), 131–149.
McCann, I. L., & Pearlman, L. A. (1992). Constructivist self-development theory: A theoretical model of psychoanalytic adaptation to severe trauma. In D. K. Sakheim & S. E. Devine (Eds.), Out of darkness: Exploring satanism and ritual abuse (pp. 185–206). New York: Lexington Books.
Meichenbaum, D. (1994). A clinical handbook/practical therapist manual for assessing and treating adults with post-traumatic stress disorder (PTSD). Waterloo, ON, Canada: Institute Press.
Nuttmann-Shwartz, O., & Dekel, R. (2009). Challenges for students working in a shared traumatic reality. The British Journal of Social Work, 39, 522–538.
Pearlman, L., & MacIan, P. (1995). Vicarious traumatization: An empirical study of the effects of trauma work on trauma therapists. Professional Psychology: Research and Practice, 26, 558–565.
Pearlman, L., & Saakvitne, K. (1995). Trauma and the therapist: Countertransference and vicarious traumatization in psychotherapy with incest survivors. New York: Norton.
Saakvitne, K. W. (2002). Shared trauma: The therapist’s increased vulnerability. Psychoanalytic Dialogues, 12(3), 443–449.
Sabin-Farrell, R., & Turpin, G. (2003). Vicarious traumatization: Implications for the mental health of health workers. Clinical Psychology Review, 23, 449–480.
Schmideberg, M. (1942). Some observations on individual reactions to air raids. International Journal of Psychoanalysis, 23, 146–176.
Seeley, K. M. (2008). Therapy after terror: 9/11, psychotherapists, and mental health. New York: Cambridge University Press.
Shamai, M., & Ron, P. (2009). Helping direct and indirect victims of national terror: Experiences of Israeli social workers. Qualitative Health Research, 19, 42–54.
Stamm, B. H. (1995). The Professional Quality of Life Scale: Compassion satisfaction, burnout, & compassion fatigue/secondary trauma scales. Pocatello, ID: Sidran Press.
Stamm, B. H. (2002). Measuring compassion satisfaction as well as fatigue: Developmental history of the fatigue and satisfaction test. In C. R. Figley (Ed.), Treating compassion fatigue (pp. 107–119). New York: Brunner Mazel.
Tosone, C. (2006). Therapeutic intimacy: A post-9/11 perspective. Smith College Studies in Social Work, 76(4), 89–98.
Tosone, C. (in press). Shared trauma. In C. Figley (Ed.), Encyclopedia of Trauma. London: Sage Publishers.
Tosone, C., & Bialkin, L. (2003). The impact of mass violence and secondary trauma in clinical practice. In L. A. Straussner & N. Phillips (Eds.), Social work with victims of mass violence (pp. 157–167). New York: Jossey Bass.
Tosone, C., Bialkin, L., Campbell, M., Charters, M., Gieri, K., Gross, S., et al. (2003). Shared trauma: Group reflections on the September 11th disaster. Psychoanalytic Social Work, 10(1), 57–77.
Tosone, C., McTighe, J., Bauwens, J., & Naturale, A. (2011). Shared traumatic stress and the long-term impact of September 11th on Manhattan clinicians. Journal of Traumatic Stress, 24(5), 546–552.
Van Der Kolk, B., & Saporta, J. (1991). The biological response to psychic trauma: Mechanisms and treatment of intrusion and numbing. Anxiety Research, 4, 199–212.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tosone, C., Nuttman-Shwartz, O. & Stephens, T. Shared Trauma: When the Professional is Personal. Clin Soc Work J 40, 231–239 (2012). https://doi.org/10.1007/s10615-012-0395-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10615-012-0395-0