Abstract
This study investigated associations of degree of spread at diagnosis of breast cancer and socio-demographic factors with the risk of death among NSW females diagnosed in 1980–2003. Trends by diagnostic period, socio-demographic differences, and the implications for cancer control were considered. NSW Central Cancer Registry data were analyzed using regression and rank-order tests to show predictors of death from breast cancer and trends in degree of spread. Compared with localized disease, case fatality was thrice and 14 times higher for cancers with regional spread and distant metastases, respectively. After adjusting for degree of spread and socio-demographic differences, the relative risk of death from breast cancer has declined in recent diagnostic periods compared with the 1980–1983 baseline, reaching a low of 0.38 (0.35, 0.40) for 1999–2003. Age-specific analyses indicated that relative risks were lower in 1999–2003 for 50–69 year olds (RR = 0.31) than younger (RR = 0.40), or older (RR = 0.46) females. Regional or distant disease at diagnosis was lowest in the older age groups, the highest socio-economic stratum and in more recent periods. Females born in nonEnglish speaking countries presented with more advanced disease, as did metropolitan women with the highest access to health services. Degree of spread of cancer at diagnosis is a powerful predictor of case fatality. Case fatalities from breast cancer have declined by diagnostic period, after adjusting for degree of spread, which may reflect treatment and screening advances. Attention should be directed at reducing disparities by socio-economic status and encouraging migrant women to present earlier.
Similar content being viewed by others
Introduction
Despite reductions in breast cancer mortality in Australia since the early 1990s, breast cancer remains the leading cause of cancer death in females, with 2,641 deaths in 2004 [1]. It is recognized that risk of death in breast cancer patients relates to the extent of spread of the cancer at diagnosis [2, 3]. Earlier Australian data have shown that in the ten years following diagnosis, about 90% of TNM stage IV cases (i.e., those with distant metastases at diagnosis) died from their cancer, while the corresponding figure was only about 15% for stage I cases (i.e., those with localized cancers of 2 cm in diameter or less) [4].
Collective evidence from eight randomized trials indicates that screening mammography reduces death rates from breast cancer [5–13]. An expert committee of the International Agency for Research on Cancer reported in 2002 that a 35% reduction in breast cancer mortality would be expected in screening participants [14]. A further review of cohort and nonrandomized control trial studies found a combined 32% reduction in breast cancer mortality associated with attending screening, after adjustment for self selection [15]. In a New South Wales (NSW) study of breast-screened women and breast cancer mortality, a 70% biennial screening rate was also found to be associated with a 32% lower breast cancer mortality [16].
Australian health policy has long emphasized early detection as a means of reducing breast cancer mortality and promoting breast-conserving treatment [17, 18]. During the 1980s, emphasis was placed on breast self-examination and physical breast examination by a health professional [17, 18], but the emphasis shifted to population-based screening mammography when screening programs of this type were introduced in the 1990s [18, 19]. By the mid-1990s, about half the Australian female population in the 50–69 year target age range was participating in this screening, with the proportion reaching 57% by the early 2000s [19]. Participation in NSW is similar to the national average.
Meanwhile, other initiatives apart from earlier detection were introduced to improve breast cancer survival, including advances in adjuvant therapies, increased surgical specialization, the active promotion of evidence-based clinical guidelines and increased support for clinical audit [20–22]. In 1998, the Breast Section of the Royal College of Surgeons commenced data monitoring of clinical practice to assist Members audit their care and maintain high standards [22–24]. While it is clear that breast cancer mortality has reduced since the early 1990s, the respective contributions: (1) of treatment advances, as applying to tamoxifen and other adjuvant therapies, and (2) of screening and related earlier detection, are not known [25, 26].
The NSW Central Cancer Registry, the USA SEER system and some other population-based registries have monitored extent of disease at the diagnosis of breast cancer using degree of spread as a summary staging measure [27, 28]. In this classification, cancers are categorized as local (localized to the primary organ site), regional (involving regional nodes), or distant (metastasized to distant organs or lymph nodes). While this is a less-specific classification than the accepted clinical and pathological TNM staging, degree of spread can be coded by Registry and hospital staff from the pathology and other clinical reports available to them. In addition, this measure is widely applicable across many solid tumor types. Despite the potential for differences in methodology when recording degree of spread, the NSW distribution of breast cancers by degree of spread, and case survivals by category of degree of spread, is consistent to those observed in SEER data [27–29].
In this study, we investigate trends in case fatality by degree of spread for breast cancers diagnosed in 1980–2003 to confirm the validity of this measure as an outcome predictor. Proportional hazards regression analyses were also used: to confirm the prognostic importance of this measure; and to investigate whether reductions in case fatality were occurring which may reflect treatment effects; to identify subgroups of women at elevated risk of advanced disease who may require special attention in early-detection initiatives degree of spread of breast cancers at diagnosis in NSW during 1980–2003; and differences by socio-demographic characteristics were considered. In addition, the characteristics of women who present with localized cancer could direct recruitment strategies for screening programs. Implications of results for cancer-control planning are considered.
Methods
Data sources and definitions
The NSW Central Cancer Registry (the Registry) was the data source for this study. Death information was retrieved by electronic linkage of the Registry with NSW death records and with the National Death Index at the Australian Institute of Health and Welfare. Operational details of the Registry have been described previously [27]. Notifications to the Registry of invasive female breast cancers (ICD-10 code: C50) diagnosed in NSW are mandated from pathology laboratories, hospitals and other treatment centers under the NSW Public Health Act 1991 [27]. For the approximate 90% of breast cancers where data on degree of spread at diagnosis is available, these cancers are categorized as local, regional or distant.
Breast cancers in females notified to the Registry with a 1980–2003 diagnosis and a recorded degree of spread were investigated in this study, apart from a small number (<1%) identified from autopsy or death records. These cases were excluded because the date of diagnosis does not precede the date of death, leaving no survival period for analysis.
Women diagnosed with breast cancer were classified by: (1) age at diagnosis categorized in decades with open-ended categories under 40 and over 80 years; (2) socio-economic status—five ordinal categories using the residential local government area (LGA) based Socioeconomic Index of Relative Disadvantage for Areas (SEIFA) [30]; (3) service access—geographic access to services based on distance to services–five ordinal categories using the residential LGA-based Accessibility/Remoteness Index of Australia (ARIA)[31]; and (4) country of birth—Australian born, other English-speaking country or nonEnglish-speaking country. A small number (5.2%) with unknown country of birth were classified with the Australian born for the purposes of this study. Further details about these classifications have been reported previously [27, 30, 31]. Years of diagnosis were grouped into five diagnostic periods for statistical analysis. Degree of spread was classified as localized, regional and distant.
Statistical analyses
Analyses were undertaken using SAS version 9 software [32]
Case fatalities by degree of spread and other predictors
The percentages of women (±standard errors) dying of breast cancer within five and ten years of diagnosis were calculated using Kaplan Meier product-limit estimates [32, 33]. This cause-specific survival method has been shown to provide similar outcome estimates to relative-survival methods for NSW and other Australian jurisdictions [34, 35]. Live cases were censored on 31 December 2004, whereas those dying before this date were censored at their date of death. Percentages of patients diagnosed with and dying from their breast cancer by five and ten years from diagnosis were presented by degree of spread for each socio-demographic characteristic, and for successive diagnostic periods.
A multivariate Cox proportional hazards regression analysis was also undertaken to confirm the importance of degree of spread and other predictors of case fatality [32, 33]. Degree of spread, diagnostic period, and all socio-demographic variables were entered stepwise into the model, retaining those variables that increased model fit (p ≤ 0.05).
Degree of spread by diagnostic period and socio-demographic characteristic
Degree of spread was analyzed by diagnostic period, age at diagnosis, socioeconomic status, remoteness index, and country of birth. Inferential testing was based on Spearman rank order analyses for characteristics measured on an ordinal scale, and the Kruskal-Wallis ANOVA for nominal variables respectively [32, 33].
Multinomial logistic regression analysis was also undertaken to identify factors predictive of regional or distant as opposed to localized disease [32, 33]. Specifically, diagnostic period and all socio-demographic variables were entered stepwise into the model, retaining those variables that increased model fit (p ≤ 0.05).
Results
Case fatality
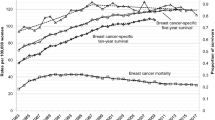
There were 59,731 cases of breast cancer diagnosed in NSW between 1980 and 2003 with a known extent of disease at diagnosis, which were included in this analysis. Of these, 34,688 (58.1%) had localized spread at diagnosis, 21,904 (36.7%) had regional lymph node involvement and 3,139 (5.3%) had distant metastases. Case fatality percentages declined progressively across successive diagnostic periods. Five-year case fatalities reduced from 15.4% in 1980–1983 to 4.5% in 1999–2003 for localized cancers (p < 0.001), with corresponding reductions from 37.8% to 17.0% for cancers with regional spread (p < 0.001), and from 80.5% to 59.2% for distant spread (p < 0.001). Case fatality percentages increased with age at diagnosis for distant cases, with five-year fatalities ranging from 61.3% among women less than 40 years to 90.2% for those aged 80 years or more (p < 0.001), with a similar trend applying for 10-year fatality percentages. While women aged 80 years or more also had the highest case fatality percentages in the localized and regional tumor categories—both at five and ten years from diagnosis—relatively high fatalities were also suggested for women less than 40 years of age. Case fatalities were lowest for women aged 50–69 years when the breast cancer was localized at diagnosis (p < 0.001). There were better outcomes in the highest socioeconomic areas, particularly for localized cancer (p < 0.001); and in women born in nonEnglish-speaking countries, regardless of spread of disease, especially at five years post diagnosis (p < 0.001) (Table 1).
The multivariate analysis confirmed that more advanced degree of spread, earlier diagnostic period, not being in the highest socio-economic category and either being less than 40 years or more than 70 years of age at diagnosis were predictive of a higher case fatality. While there was also the indication that women born in a nonEnglish-speaking country had a lower case fatality, the difference was small and only marginally statistically significant (p = 0.050). The model indicated a pronounced reduction in the relative risk of death across successive diagnostic periods, with a low relative risk of 0.38 (0.35, 0.40) for 1999–2003, when compared with the 1980–1983 base-line period (i.e., a 62% reduction), after adjusting for degree of spread, age, socioeconomic status and country of birth (Table 2).
Age-specific Cox models also showed a pronounced decline in hazard ratios for each age category, after adjusting for degree of spread, socioeconomic status, and country of birth. Compared with 1980–1983, the likelihood of death declined by diagnostic period to a low in 1999–2003 of 0.40 (0.35, 0.46) (i.e., a 60% reduction) in females under 50 years of age; 0.31 (0.28, 0.35) (i.e., a 69% reduction) in 50–69 year olds; and 0.46 (0.41, 0.51) (i.e., a 54% reduction) in females aged 70 years or more (data not shown).
Degree of spread
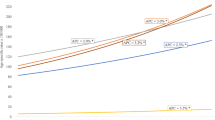
Degree of spread varied by age at diagnosis (p < 0.001). The percentage of cancers that were localized increased from 50.0% in females less than 40 years of age to 62.3% in 70–79 year olds and 61.9% in those aged 80 years or more. However, the percentage of patients with distant spread increased from 3.8% in females aged less than 50 years at diagnosis to 9.7% in those aged 80 years or more. Degree of spread also varied by diagnostic period (p < 0.001), with 1980–1983 data showing the highest percentage of distant spread, and with a trend toward localized spread in 1994–1998, after which there was a reversal in trend in 1999–2003. Differences in degree of spread also occurred by socioeconomic status (p < 0.001), with less distant disease found in the highest socioeconomic category; and by country of birth (p < 0.001), with women born in nonEnglish-speaking countries tending to have more regional spread of disease at diagnosis. Meanwhile, a difference also was observed by the remoteness index (ARIA index) (p = 0.004), with more extensive spread found in women in the lowest and highest remoteness index (Table 3).
There was an increase in the percentage of patients presenting with localized disease at diagnosis over the study period in all ages, but particularly in 50–69 and 70–79 year olds (p < 0.001). The percentage of cases with regional or distant metastases has declined in 50–69 year olds from 45.3% in 1980–1983 to 36.5% in 1994–1998, after which there was an increase to 41.1% in 1999–2003. Meanwhile corresponding percentages of regional or distant lesions in 70–79 year olds reduced from 39.4% in 1980–1983 to 33.8% in 1994–1998, after which there was an increase to 36.9% in 1999–2003. By comparison, percentages of regional or distant spread across time periods remained unchanged in women aged less than 50 years or those aged 80 years or more (p > 0.400) (data not shown).
Multinomial logistic regression analysis confirmed that the odds of regional spread at diagnosis compared to localized spread declined by age at diagnosis, but the odds of distant compared to localized increased by age at diagnosis. Odds ratios for both regional and distant spread, compared to localized spread declined by diagnostic period. This decline was only statistically significant for women diagnosed with distant disease, compared to localized. Women of high socioeconomic status were less likely to be diagnosed with regional and distant disease compared to localized, with odds ratios of 0.86 and 0.74, respectively. Patients residing in highly accessible areas were more likely to present with regional spread at diagnosis than localized or distant spread. Women born in nonEnglish-speaking countries were more likely to be diagnosed with regional and distant disease than localized disease at diagnosis (Table 4).
The model refitted with interaction terms for age and period of diagnosis showed that there was an interaction between age and period of diagnosis (p < 0.001), which was most evident in from 1989 onward in the age ranges of 50–59 and from 60 to 69 years (data not shown).
Due to the interaction between age and period of diagnosis, age-specific multinomial logistic regression analyses were undertaken, including the same predictor variables. These analyses indicated that the decreases in odds ratios for regional and distant spread between 1980 and 1983 and 1994 and 1998 were most pronounced in 50–69 year olds and least pronounced for females less than 50 years of age and 70 years and older. Nonetheless, a marked decline by period of diagnosis in women with distant metastases compared to localized spread was evident for all three age categories compared with the 1980–1983 baseline. The relative odds of distant spread for 1989–1993 and 1994–1998, respectively were: 0.69 (0.51, 0.93) and 0.54 (0.40, 0.73) for women under 50 years of age; 0.65 (0.54, 0.80) and 0.43 (0.35, 0.52) for 50–69 year olds and 0.74 (0.59, 0.92) and 0.57 (0.46, 0.71) for those aged 70 years or more diagnosed between 1989 and 2003. The relative odds of regional spread were only significant for women aged 50–69 years diagnosed between 1994 and 2003 (data not shown).
Discussion
Degree of spread is a powerful predictor of case fatality. Women have a much higher chance of surviving in NSW if they are diagnosed with localized breast cancer: three times more than regional and 14 times more than distant. The likelihood of death from breast cancer declined over time while controlling for the effects of age, stage of diagnosis, socio-economic status and country of birth with most of the reduction occurring between 1989 and 1998. This is the period when screening mammography was being introduced and extended. Larger reductions in case fatality by degree of spread were found in the 50–69 year old screening target than in younger or older women.
Women diagnosed with breast cancer also showed a trend toward more localized presentation at diagnosis, this was most evident between 1989 and 1998. This trend of a stage shift toward more localized spread at diagnosis was most prominent in the 50–69 year screening target range, which is suggestive of a screening effect. Localized breast cancer was more common in females in the highest socioeconomic category regardless of age at diagnosis, whereas women born in non-English speaking countries tended to present with more regional and distant extent of disease at diagnosis regardless of age.
The NSW Central Cancer Registry is the largest cancer registry in Australia and the only registry that routinely collects data on degree of spread. While clinical and pathological TNM stage coding would have been more ideal, the present degree of spread data represent the experience of the general population of females with invasive breast cancer and should be minimally affected by the selection biases (to which TNM data from hospital-based and other clinical collections would be prone). The data from the Registry provided a unique opportunity in Australia to explore trends in survival together with degree of spread.
Coding of extent of disease has shown some variability over time, in that from 1994 onwards, electronic inpatient hospital notifications provided more clinical information on whether a breast cancer was regional or distant metastases at diagnosis. While the increased likelihood of presentation with regional and distant disease in women aged over 70 years may be true, it may also indicate less extensive investigation in this age group compared to younger women.
The NSW Central Cancer Registry uses both pathology and hospital information to determine the final extent of disease over a 120-day period from first notification to the Registry. A higher proportion of localized and regional cases are histologically verified compared to cases with distant metastases this is because imaging and other clinical investigations are used to determine metastases. However, 75% of all breast cancer cases during this study had a pathology report that had been reviewed and coded by experienced NSW Central Cancer registry coding staff. When we repeated our analysis using only registry coded records our findings were the same. In addition, while about 10% of breast cancers did not have a recorded degree of spread, this appeared also not to affect findings. When we repeated our analyses, including cases with an unknown degree of spread, similar temporal and socio-demographic differences in regional and distant, as opposed to localized disease, presented to those reported. Specifically, the point estimates did not alter, but the confidence intervals were slightly wider, reflecting some reduction in statistical precision.
It is evident that progressive reductions in case fatality have also occurred for reasons independent of earlier detection. After adjusting for degree of spread, hazard ratios declined by period of diagnosis to 0.38 (0.35, 0.40) in 1999–2003, when compared with the 1980–1983 base-line period. It is unlikely that such a marked reduction would have been due to confounding from the coarseness of degree of spread as a staging measure. There have been advances in adjuvant therapies, increased surgical specialization, increases in the proportion of patients participating in clinical trials, promotion of evidence-based clinical guidelines, increased clinical audit, and other clinical initiatives, all of which may have contributed to these better outcomes [20–22]. The indication of a greater reduction in case fatality, after adjusting for degree of spread, in the 50–69 year old screening target, may also reflect the emphasis placed on an effective screening pathway (i.e., a higher quality of diagnosis and treatment for women with screen-detected cancers may have applied and contributed to this effect).
The reversal in trend toward a more extensive degree of spread in 1999–2003 compared with 1994–1998 was unexpected and not accompanied by a commensurate decrease in population-screening coverage [36]. It is possible that increased attention to regional lymph node investigation during this period, perhaps associated with the introduction and evaluation of sentinel node biopsies, may have led to an increase in sensitivity in detecting positive nodes [37]. Also, advances in imaging technology may have increased the probability of detecting distant metastases [38]. An alternative hypothesis is that increases in breast density associated with increased use of hormone replacement therapy may have led to a reduction in mammographic sensitivity [39, 40].
Additional investigation of this reversal in trend toward later diagnostic stages is indicated.
Case fatality also increased in older women aged 70 years or more, after adjusting for degree of spread. The poorer outcomes in older women may reflect increased co-morbidity and frailty with older age, and a reduced capacity to withstand negative effects of the cancer and its treatment [41]. It is likely that treatment plans often would be compromised to accommodate these factors in older patients, leading to poorer prospects for cure [41]. Additional research is needed to optimize treatment outcomes in older women, particularly in those with significant co-morbidity.
Determining the respective contribution of screening and treatment to reduction in mortality is a complex task. A USA study that employed seven independent statistical models found that the average contribution of screening was 46% (28–65%) with adjuvant treatment contributing to the rest [42]. In general, treatment outcomes appeared to be less favorable in NSW residents outside the highest socioeconomic areas. This was not explained by differences in degree of spread and warrants further health-service research. Socioeconomic differences in survival of breast cancer patients have been examined in 24 studies. In 19 studies, survival was poorest in low socioeconomic groups; in addition a multicenter study found the same pattern in three out of four countries. In 13 of these studies, differences were statistically significant or were wider than 10% at five years.
The evidence for marginally lower case fatalities in women from non-English speaking counties of birth was not strong (p = 0.050), and may reflect a tendency for some of these women to return to their countries of birth during terminal stages of their disease, such that their deaths are not notified to the Registry. Notably, women born in non-English speaking countries tended to have more regional cancers at diagnosis than other women and BreastScreen data indicate that they are less likely to participate in screening [36]. Increased emphases would appear to be warranted on early-detection initiatives in these women (e.g., as in the employment of community liaison officers of nonEnglish speaking background).
Breast cancers showed a trend toward more localized presentation at diagnosis between 1980 and 1983 and 1994 and 1998. Most of this gain occurred during the 1989–1993 and 1994–1998 period when population-based screening mammography was being introduced and extended [36, 43]. This trend of a stage shift toward more localized spread at diagnosis was most prominent in the 50–69 year screening target range, which is consistent with a screening effect. Localized breast cancer was more common in females in the highest socioeconomic category regardless of age at diagnosis, whereas women born in non-English speaking countries tended to present with more regional and distant extent of disease at diagnosis regardless of age. Means of reducing these inequalities require special attention.
In general, there was no significant improvement by period of diagnosis in women aged less than 49 years of age with regional spread and some improvement in women with distant disease diagnosed between 1989 and 1998. Women aged less than 40 years were not eligible for free mammographic screening (via BreastScreen) and would tend more to present with symptomatic disease [36]. Moreover, these women also had a higher case fatality than the 50–69 year olds. This observation is consistent with earlier evidence of poorer outcomes among younger females [44]. These women often have denser and more radio-opaque breast tissue, which could reduce opportunities for early cancer detection [45]. While age-standardized incidence trends in NSW and Australia have remained constant over time for the small proportion of women affected in this age category [43], a research focus on means of achieving earlier detection and better treatment outcomes in younger females should be a priority.
In women aged 70 years and older at diagnosis there was little improvement by period of diagnosis in women presenting with regional spread. The likelihood of presenting with distant disease at diagnosis declined for each diagnostic period from 1989 onwards, which is consistent with both a screening and treatment effect.
Metropolitan women living in highly accessible areas tended to have more advanced cancers at diagnosis than other women. Notably, relatively low BreastScreen screening participation rates have been reported in metropolitan NSW and in other major cities around Australia [19, 36]. While it was indicated in the BreastScreen Australia monitoring report for 2002–2003 that this may reflect a greater access to private radiology services in metropolitan areas, it was also suggested that some working women in major cities may have difficulties accessing BreastScreen services [19]. In addition, it is possible that lower BreastScreen participation rates among some metropolitan women could be indicative of less active participation in other early detection initiatives. Either way, the net effect appears to be more advanced cancers in highly accessible areas, compared to other categories. BreastScreen data also have pointed to a relatively low screening participation in remote areas, both in NSW and in Australia more generally [19, 36].
Many factors influence participation in public screening programs. A review of characteristics of women who attend screening found that women aged between 50 and 70 years were more likely to attend screening than older women; and that lower socio-economic and income status were associated with lower participation and was an independent predictor of attendance within racial or ethnic groups within the USA [46]. In Italy, however, this did not apply. Less well-educated women were more likely to attend a public screening program and socioeconomic status was not related to attendance. Findings from studies that investigated effects of rural residence on participation are inconsistent, as are findings on ethnic background and attendance [46, 47].
Women with a good knowledge of screening, who believe that attendance is effective in finding small cancers, are more likely to attend; as are married and single women compared to divorced and separated women. A strong fear that breast cancer will be detected was associated with a decreased likelihood of attendance [46]. A review of the evidence indicates that five interventions were found to be effective in increasing screening participation [47]. These included single letters of invitation at 12 and 24 months from screening; mailed educational material; a letter of invitation for screening plus a phone call; and an individual phone call plus training activities. The combination of a letter and a phone call achieved a better response than either intervention separately, particularly for women of low socio-economic status [47].
Our results are consistent with other research in Australia, which has showed a marked reduction in proportion of breast cancers detected when large (diameters ≥3 cm) following the introduction of population-based screening and related early-detection initiatives [48]. Larger tumors continue to present more frequently outside the principal screening age range of 50–69 years and in lower socioeconomic areas and in some country locations, in nonCaucasians, and among women born in a number of nonEnglish-speaking countries [48].
References
Australian Institute of Health and Welfare & National Breast Cancer Centre (2006) Breast Cancer in Australia: an overview, 2006. Canberra: AIHW, Cancer Series no. 34, cat no. CAN 29
Benson JR, Weaver DL, Mittra I, Hayashi M (2003) The TNM staging system and breast cancer. Lancet Oncol 4:56–60. doi:10.1016/S1470-2045(03) 00961-6
Bland K, Menck H, Scott-Conner C, Morrow M, Winchester DJ, Winchester DP (1998) The National Cancer Data Base 10-year srvey of breast carcinoma treatment at hospitals in the United States. Cancer 83:1262–1273. doi:10.1002/(SICI)1097-0142(19980915)83:6≤1262::AID-CNCR28≥3.0.CO;2-2
South Australian Cancer Registry (2000) Epidemiology of cancer in South Australia. Incidence, mortality and survival, 1977 to 1999. Incidence and mortality, 1999. Openbook Publishers, Adelaide, p 129
Demissie K, Mills OF, Rhoads GG (1998) Empirical comparison of the results of randomised controlled trials and case-control studies in evaluating the effectiveness of screening mammography. J Clin Epidemiol 51:81–91. doi:10.1016/S0895-4356(97) 00243-6
Shapiro S, Venet W, Strax P, Venet L, Roeser R (1985) Selection, follow-up and analysis in the health insurance plan study: a randomised trial with breast cancer screening. Natl Cancer Inst Monogr 67:65–74
Andersson I, Aspegren K, Janzon L, Landberg T, Lindholm K, Linell F, Ljungberg O, Ranstam J, Sigfusson B (1988) Mammographic screening and mortality from breast cancer: the Malmo mammographic screening trial. BMJ 297:943–948
Tabar L, Fagerberg G, Duffy S, Day N, Gas A, Grontoft O (1992) Update of the Swedish two county program of mammographic screening for breast cancer. Radiol Clin North Am 30:187–210
Roberts MM, Alexander FE, Anderson TJ, Chetty U, Donnan PT, Forrest P, Hepburn W, Huggins A, Kirkpatrick AE, Lamb J et al (1990) Edinburgh trial of screening for breast cancer: mortality at seven years. Lancet 335:241–246. doi:10.1016/0140-6736(90) 90066-E
Miller AB, Baines CJ, To T, Wall C (1992) Canadian National Breast Screening Study, 1: breast cancer detection and death rates among women aged 40 to 49 years. CMAJ 147:1459–1476
Miller AB, Baines CJ, To T, Wall C (1992) Canadian National Breast Screening Study, 2: breast cancer detection and death rates among women aged 50 to 59 years. CMAJ 147:1477–1488
Frisell J, Eklund G, Hellstrom L, Lidbrink E, Rutqvist LE, Somell A (1991) Randomized study of mammography screening: preliminary report on mortality in the Stockholm trial. Breast Cancer Res Treat 18:49–56. doi:10.1007/BF01975443
Nystrom L, Rutqvist LE, Wall S, Lindgren A, Lindqvist MJ, Ryden S, Andersson I, Bjurstam N, Fagerberg G, Frisell J et al (1993) Breast cancer screening with mammography: overview of Swedish randomised trials. Lancet 341:973–978. doi:10.1016/0140-6736(93) 91067-V
International Agency for Research on Cancer (IARC) (2002) Press Release No. 139. Mammography can reduce deaths from breast cancer. March 19th
Gabe R, Duffy SW (2005) Evaluation of service screening mammography in practice: the impact on breast cancer mortality. Ann Oncol 16(Suppl 2):ii153–ii162. doi:10.1093/annonc/mdi718
Taylor R, Morrell S, Estoesta J, Brassil A (2004) Mammography screening and breast cancer mortality in New South Wales, Australia. Cancer Causes Control 15:543–550. doi:10.1023/B:CACO.0000036153.95908.f2
MacLennan R (1987) A national cancer prevention policy for Australia, vol vol 1. Australian Cancer Society, Sydney
Australian Health Ministers Advisory Council, Breast Cancer Screening Evaluation Steering Committee (1990) Breast cancer screening in Australia: future directions. Canberra: Australian Institute of Health, cancer series no. 1
The Australian Institute of Health and Welfare & the Australian Government of Health and Ageing for the BreastScreen Australia Program (2006) BreastScreen Australia monitoring report 2002–2003. Canberra: Australian Institute of Health and Welfare, Cancer Series no.32, cat. no. CAN 27
National Health and Medical Research Council (1995) The management of early breast cancer. Clinical practice guidelines. National Health and Medical Research Council, Canberra
National Breast Cancer Centre (2004) Clinical practice guidelines for the management and support of younger women with breast cancer. Australian Government and National Health and Medical Research Council, Canberra
Malycha P, Tyson S (2000) National breast surgery audit. Aust NZ J Surg 70:834–836. doi:10.1046/j.1440-1622.2000.02002.x
Boult M, Cuncins-Hearn A, Tyson S, Kollias J, Babidge W, Maddern G (2005) National breast cancer audit: establishing a web-based data system. ANZ J Surg 75:844–847. doi:10.1111/j.1445-2197.2005.03547.x
Cuncins-Hearn A, Boult M, Babidge W, Zorbas H, Villanueva EV, Evans A, Oliver D, Kollias J, Reeve T, Maddern G (2006) National breast cancer audit: overview of invasive breast cancer management. ANZ J Surg 76:745–750. doi:10.1111/j.1445-2197.2006.03846.x
Paci E, Ponti A, Zappa M, Patriarca S, Falini P, Delmastro G, Bianchi S, Sapino A, Vezzosi V, Senore C, Crocetti E, Frigerio A, Zanetti R, Det Turco MR, Segnan N (2005) Early diagnosis, not differential treatment, explains better survival in service screening. Eur J Cancer 41:2728–2734. doi:10.1016/j.ejca.2005.06.026
Yu X, O’Connell D, Gibberd R, Coates AS, Armstrong BK (2006) Trends in survival and excess risk of death after diagnosis of cancer in 1980–1996 in New South Wales, Australia. Int J Cancer 119:894–900. doi:10.1002/ijc.21909
Tracey EA, Chen S, Baker D, Bishop J, Jelfs P (2006) Cancer in New South Wales: Incidence and mortality 2004: Sydney: Cancer Institute NSW
Ries LAG, Harkins D, Krapcho M, Mariotta A, Miller BA, Feuer EJ, Clegg L, Eisner MP, Horner MJ, Howlader N, Hatat M, Hankey BF, Edwards BK (eds) (2006) SEER Cancer Statistics Review, 1975–2003. National Cancer Institute, Bethesda MD
Jemal A, Siege R, Ward E, Murrat T, Xu J, Smigal C, Thun MJ (2006) Cancer Statistics, 2006. CA Cancer J Clin 56:106–130
Australian Bureau of Statistics (1998) 1996 census of population and housing. Socio-economic indexes for areas. Australian Bureau of Statistics, Canberra
Department of Health and Aged Care and the University of Adelaide (1999) Measuring remoteness: accessibility/remoteness index of Australia (ARIA). Occasional Papers: New Series No. 6. Canberra, Commonwealth of Australia
SAS/STAT software, Version 9.1 (2003) Cary, NC: SAS Institute Inc
Armitage P, Berry G (1987) Statistical methods in medical research, 2nd edn. Blackwell Scientific Publications, Oxford
Tracey EA, Bishop J, Roder D, Jelfs P (2006) Comparison of cause-specific and relative survival for major cancer sites in NSW. Asia Pac J Clin Oncol 2(Suppl 2):A70
South Australian Cancer Registry (1997) Epidemiology of cancer in South Australia. Incidence, mortality and survival, 1977 to 1996. Incidence and mortality, 1996. Openbook Publishers, Adelaide, p 21
Estoesta JV, Gao K, Ho C, Taylor RJ, Brassil AE, BreastScreen New South Wales (2004) BreastScreen NSW Statistical Report, 1999–2002. BreastScreen NSW, Sydney
Wetzig NR, Gill PG, Ung O, Collins J, Kollias J, Gillett D, Gebski V, Greig C, Ray A, Stockler M, RACS SNAC Group (2005) Participation in the RACS sentinel node biopsy versus axillary clearance trial. Aust NZ J Surg 75:98–100. doi:10.1111/j.1445-2197.2005.03310.x
Freeman M (2004) Imaging: new techniques. In: Harris JR, Lippman ME, Morrow M, Osborne CK (eds) Diseases of the breast. Lippincott Williams & Wilkins, Philadelphia, pp 181–198
Ruttner CM, Mandelson MT, Laya MB, Taplin S (2001) Changes in breast density associated with initiation, discontinuation, and continuing use of hormone replacement therapy. JAMA 285:171–176. doi:10.1001/jama.285.2.171
MacLennan AH, Wilson DH, Taylor AW (2004) Hormone replacement therapy use over a decade in an Australian population. Climacteric 7:138–142. doi:10.1080/13697130410001713733
Eaker S, Dickman PW, Bergkvist L, Holmberg L, and The Uppsala/Orebro Breast Cancer Group (2006) Differences in management of older women influence breast cancer survival: results from a population-based database in Sweden PloS Med 3:e25
Berry DA, Cronin KA, Plevritis SK, Fryback DG et al (2005) Effect of screening and adjuvent therapy on mortality from breast cancer. NE J Med. Boston: October 27th, 353(17): p 1784, 9 pp
Australian Institute of Health and Welfare & National Breast Cancer Centre (2006) Breast cancer in Australia: an overview, 2006. Cancer series no. 34. cat. no. CAN 29. Canberra: Australian Institute of Health and Welfare
Fowble BL, Schultz DJ, Overmoyer B, Solin LJ, Fox K, Jardines L, Orel S, Glick JH (1994) The influence of young age on outcome in early stage breast cancer. Int J Radiat Oncol Biol Phys 30:23–33
Leach MD, Boggis CR, Dixon AK, Easton DF, Eeles RA, Evans DG, Gilbert FJ, Griebsch I, Hoff RJ, Kessar P, Lakhani SR, Moss SM, Nerurkar A, Padhani AR, Pointon LJ, Thompson D, Warren RM, MARIBS study group (2005) Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 365:1769–1778. doi:10.1016/S0140-6736(05)66646-9
Bonfill X, Marzo M, Pladevall M, Marti J, Emparanza Jl (2006) Strategies for increasing the participation of women in community breast cancer screening (Review). The Cochrane Collaboration, Issue 4. John Wiley and Sons limited
Vainio H, B IARC Handbooks of Cancer Prevention (2002) Breast Cancer Screening. vol 7. IARC press International Agency for Research in Cancer Lyon
Luke C, Nguyen A-M, Priest K, Roder D (2004) Female breast cancers are getting smaller, but socio-demographic differences remain. Aust NZ J Public Health 28:312–316. doi:10.1111/j.1467-842X.2004.tb00435.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tracey, E., Roder, D., Zorbas, H. et al. Survival and degree of spread for female breast cancers in New South Wales from 1980 to 2003: implications for cancer control. Cancer Causes Control 19, 1121–1130 (2008). https://doi.org/10.1007/s10552-008-9177-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9177-y