Abstract
The purpose of this investigation was to compare the efficacy of colistin-based therapies in extremely drug-resistant Acinetobacter spp. bloodstream infections (XDR-ABSI). A retrospective study was conducted in 27 tertiary-care centers from January 2009 to August 2012. The primary end-point was 14-day survival, and the secondary end-points were clinical and microbiological outcomes. Thirty-six and 214 patients [102 (47.7 %): colistin–carbapenem (CC), 69 (32.2 %): colistin–sulbactam (CS), and 43 (20.1 %: tigecycline): colistin with other agent (CO)] received colistin monotherapy and colistin-based combinations, respectively. Rates of complete response/cure and 14-day survival were relatively higher, and microbiological eradication was significantly higher in the combination group. Also, the in-hospital mortality rate was significantly lower in the combination group. No significant difference was found in the clinical (p = 0.97) and microbiological (p = 0.92) outcomes and 14-day survival rates (p = 0.79) between the three combination groups. Neither the timing of initial effective treatment nor the presence of any concomitant infection was significant between the three groups (p > 0.05) and also for 14-day survival (p > 0.05). Higher Pitt bacteremia score (PBS), Acute Physiology and Chronic Health Evaluation II (APACHE II) score, Charlson comorbidity index (CCI), and prolonged hospital and intensive care unit (ICU) stay before XDR-ABSI were significant risk factors for 14-day mortality (p = 0.02, p = 0.0001, p = 0.0001, p = 0.02, and p = 0.01, respectively). In the multivariable analysis, PBS, age, and duration of ICU stay were independent risk factors for 14-day mortality (p < 0.0001, p < 0.0001, and p = 0.001, respectively). Colistin-based combination therapy resulted in significantly higher microbiological eradication rates, relatively higher cure and 14-day survival rates, and lower in-hospital mortality compared to colistin monotherapy. CC, CS, and CO combinations for XDR-ABSI did not reveal significant differences with respect to 14-day survival and clinical or microbiological outcome before and after propensity score matching (PSM). PBS, age, and length of ICU stay were independent risk factors for 14-day mortality.
Similar content being viewed by others
Introduction
Extremely drug-resistant Acinetobacter (XDR-A) infections cause significant mortality and morbidity among hospitalized patients, particularly in intensive care units (ICUs). Extreme drug resistance is defined by susceptibility to only one or two categories [1]. The optimal treatment of infections caused by XDR-A has not yet been established [2]. Therefore, bloodstream infections (BSI) due to XDR-A has become a major therapeutic challenge in the last two decades [3]. Inappropriate treatment of Acinetobacter infections is associated with higher mortality [2, 4, 5]. Therefore, treatment choices should be carefully considered [2].
Although prospective, randomized controlled trials are still lacking, colistin (COL) has become the foremost therapeutic option in recent years owing to its potent bactericidal efficacy even against XDR Gram-negative bacteria [6]. While XDR-A strains are supposed to be COL-sensitive, in vitro heteroresistance has been reported during COL monotherapy [7–12]. Moreover, several combination regimens show increased in vitro activity compared to single agents and are recommended to prevent the development of resistance [8]. Due to the increasing carbapenem resistance, COL-based combinations including sulbactam, carbapenem, tigecycline, rifampicin, and aminoglycosides have become virtually the only treatment of choice in Acinetobacter bloodstream infections (ABSI) [9–18]. Despite studies reporting increased treatment success with COL-based combinations compared to monotherapy in extremely drug-resistant Acinetobacter spp. bloodstream infections (XDR-ABSI), clinical studies comparing different combinations are scarce. The available clinical studies usually consisted of relatively limited numbers of patients managed at a single center. Moreover, the proportion of bacteremic cases amongst all infections due to Acinetobacter spp. was low in small-sized studies [19, 20]. Therefore, well-designed clinical trials comparing antimicrobial combinations in the treatment of XDR-A infections are necessary. In this study, we aimed to compare the efficacy of COL monotherapy and COL-based combinations with carbapenems, sulbactams, and other antimicrobials in patients with XDR-ABSI.
Materials and methods
Study design and data collection
We conducted a retrospective, observational, multicenter study including 27 tertiary-care centers across Turkey. Patients who met the criteria for either primary or secondary XDR-ABSI and who were treated with colistin monotherapy or any of the COL-based antimicrobial combinations during the study period were included. Data regarding the demographical characteristics, clinical and laboratory features, treatment modalities, adverse events, and outcome measures were obtained from patient records or hospital databases.
Inclusion criteria
-
1.
Isolation of XDR-A from ≥2 separate sets of hemoculture (peripheral veins and/or catheters) [21]
-
2.
Treatment with a COL monotherapy intravenously for ≥72 h (the dosages and routes of administration being in accordance with standard institutional practice or current medical recommendations)
-
3.
Treatment with a COL-based combination intravenously for ≥72 h (the dosages and routes of administration being in accordance with standard institutional practice or current medical recommendations)
-
4.
Treatment is considered “early” or “late” if it was initiated within or after first 24 h, respectively
-
5.
Patients could not already be on any monotherapy effective against the isolated Acinetobacter spp. when the culture was drawn and before colistin use
-
6.
Patients should not have received treatment with monotherapy that is effective against XDR-A for any period of time during their treatment course
-
7.
Only the first episode of Acinetobacter bacteremia and only an index culture collected from each patient were included in case of more than one bacteremic episode due to the same pathogen
-
8.
Any concomitant infection should have to be treated appropriately and effectively
Exclusion criteria
-
1.
Concomitant BSI with an organism other than XDR-A
-
2.
Treatment intravenously with colistin lasting <72 h
-
3.
Contraindications for colistin use
-
4.
Pregnancy
-
5.
Age <18 years
Definitions
Primary XDR-ABSI [21]
In addition to at least two of the following criteria:
-
1.
Fever (38 °C) or hypothermia (<36 °C)
-
2.
Tachypnea (respiratory rate >24/min)
-
3.
Tachycardia (pulse rate > 90/min)
-
4.
Leukocytosis (WBC > 12,000/mm3) or leukopenia (WBC < 4,000/mm3)
plus at least one of the following:
-
1.
Acinetobacter spp. cultured from two or more blood cultures drawn on separate occasions
-
2.
Acinetobacter spp. cultured from at least one blood culture from a patient with an intravascular line, and the physician institutes appropriate antimicrobial therapy and signs and symptoms and positive laboratory results are not related to an infection at another site [21]
Secondary XDR-ABSI
Isolation of XDR-A with an identical resistance pattern of the blood isolate from remote body sites (i.e., from endotracheal aspirate, urine, or wound culture).
Multidrug-resistant (MDR)
“Acquired non-susceptibility to at least one agent in three or more antimicrobial categories” (i.e., ampicillin–sulbactam, aminoglycosides, antipseudomonal carbapenems, antipseudomonal fluoroquinolones, antipseudomonal penicillins + beta-lactamase inhibitors, extended-spectrum cephalosporins, trimethoprim–sulfamethoxazole, tetracyclines, polymyxins) [1].
Extremely drug-resistant (XDR)
“Non-susceptibility to at least one agent in all but two or more antimicrobial categories” (i.e., susceptibility to only one or two categories) [1].
Pandrug-resistant (PDR)
“Non-susceptibility to all agents in all antimicrobial categories” [1].
Severity assessment scores
The severity of bacteremia, patients’ clinical status, and the underlying diseases were determined by the Pitt bacteremia score (PBS) [22], the Acute Physiology and Chronic Health Evaluation II (APACHE II) score [23, 24], and the Charlson comorbidity index (CCI), respectively [25].
Clinical outcomes
-
1.
Complete response (cure): Recovery of all symptoms, signs, and laboratory findings of infection
-
2.
Partial response: Disappearance of only some of the initial symptoms, signs, and laboratory findings of infection (fever or hypothermia, tachypnea, tachycardia, leukocytosis or leukopenia, elevated acute-phase reactants such as CRP, procalcitonin), including the condition not fulfilling all the requirements for complete response
-
3.
Treatment failure: Persistence or worsening of all symptoms and signs of infection despite antimicrobial treatment
Microbiological outcome
Microbiological eradication of Acinetobacter spp. in any control blood cultures.
The primary end-point was survival/death on the 14th day of treatment. The secondary end-points were clinical outcome, microbiological outcome, or colistin toxicity/adverse effect (nephrotoxicity, neurotoxicity).
Effective therapy
Therapy that will result in clinical cure and microbiological eradication.
Normal renal function
Baseline serum creatinine (SCR) ≤ 1.3 mg/dl (without complicated DM, chronic kidney disease, nephrotoxic drug use, hypovolemia). Nephrotoxicity: According to the RIFLE criteria [26], ≥50 % increase in baseline SCR or requirement of renal replacement therapy. Neurotoxicity: Development of peripheral and orofacial paresthesias, visual disturbances, vertigo, irritability, mental confusion, ataxia, seizures, and any neurologic impairment defined by a neurologist as neurotoxicity that did not pre-exist at the time of the start of therapy [27].
Microbiological tests
The identification of Acinetobacter baumannii isolated from blood samples was made by conventional methods and automated systems. Antimicrobial susceptibility was tested with the disk diffusion and agar dilution methods at the participating hospitals. The minimum inhibitory concentration (MIC) values were determined by the Etest, and the results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) criteria [“Performance standards for antimicrobial disk susceptibility tests; Approved standard—Eleventh edition (M02-A11)”, “Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; Approved standard—Ninth edition (M07-A9)”, and “Performance standards for antimicrobial susceptibility testing; Twenty-second informational supplement (M100-S22)”; CLSI, 940 West Valley Road, Suite 1400, Wayne, PA 19087-1898, USA, 2012].
Ethical statement/approval
This study was approved by the Institutional Review Board of Kartal Dr. Lutfi Kirdar Education and Research Hospital.
Statistical analyses
For all statistical analyses, the SPSS 17.0 software package (SPSS Inc., Chicago, IL, USA) was used. In a general comparison, categorical variables were compared by the χ2 or Fisher’s exact test, and continuous variables were tested with Student’s t-test or one-way analysis of variance (ANOVA), as appropriate. In the survival analyses, the survival rates for each treatment group were determined by the Kaplan–Meier method. In the univariate analysis, the survival rates of the groups were tested by the log-rank χ2 test for discrete random variables (i.e., categorical data) and by Cox regression analysis for continuous random variables (i.e., continuous data). Significant variables were tested by stepwise multiple Cox regression in order to determine the independent risk factors for 14-day mortality in XDR-ABSI. Propensity score matching (PSM) was performed to adjust for selection bias. The propensity score (PS) was estimated by multinomial logistic regression including all prognostic factors related to the treatment allocation. Patients who had similar PS in three different groups were matched by using the nearest neighbor matching method. Some patients who had PS < 0.35 and PS > 0.7 were excluded from groups to form the new sample. After PSM, groups had similar characteristics in risk factors. The entire analysis was repeated after PSM. A p-value < 0.05 was considered to be statistically significant.
Results
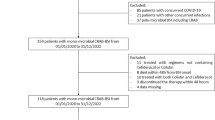
Out of the pooled data of 376 patients who were treated for ABSI in 27 tertiary-care centers in seven provinces of Turkey from January 2009 to August 2012, a total of 37 patients who received COL monotherapy and 218 patients who received COL-based combinations were enrolled in this study. Four patients in the combination therapy group and one patient in the monotherapy group who did not meet the inclusion criteria or had inadequate data were excluded (Fig. 1). Thirty-six (21, 58 % male, mean age 58.3 ± 20.5 years) patients received COL monotherapy. Among a total of 214 patients who received COL-based combination therapy, 141 (65.9 %) were male and the mean age was 59.1 ± 19.6 years. The mean durations of in-hospital follow-up were 45.8 ± 37.8 (range: 9–223) days and 56.9 (range: 5–497) days in the COL monotherapy and COL-based combination groups, respectively. The baseline characteristics of the patients, mean durations of hospitalization and ICU stay before the diagnosis of ABSI, mean CCI, mean APACHE II score, and mean PBS in the monotherapy and combination therapy groups were similar (Table 1).
Among the patients in the COL-based combination group, 102 (47.7 %), 69 (32.2 %), and 43 (20.1 %) received colistin–carbapenem (CC) (47: imipenem 4 × 500 mg, 43: meropenem 3 × 1 g, 12: doripenem 3 × 500 mg), colistin–sulbactam (CS) (in the form of ampicillin–sulbactam 4 × 3 g or sulbactam 4 × 1.5 g), and COL plus other antimicrobial agents (CO) [24: tigecycline (TIG) 2 × 50 mg after an initial 100-mg loading dose, 7: amikacin 1 × 1,000 mg, 3: netilmicin 3 × 2 mg/kg, 3: gentamicin 2 × 160 mg; in total: 13 aminoglycoside (AG), 3: rifampicin (RIF) 1 × 600 mg, 3: piperacillin–tazobactam 3 × 4.5 g], respectively. A loading dose for colistin had not been recommended at the time the study was conducted (the Sanford guide modified the colistin dosage schedule on October 08, 2012), so in our retrospective study, none of the patients had received a loading dose of colistin. Colistin daily dose in patients with normal renal function was 5 mg colistin base activity/kg/day divided into 2–3 doses in each treatment group. There were no differences in the MICs of the isolates against colistin and other antibiotics between the different treatment groups. As the number of patients receiving any of the “other” drugs in combination with COL was low in each group, we grouped them into a single group.
First of all, we compared the efficacy of colistin monotherapy and colistin-based antimicrobial combinations in patients with ABSI who had similar baseline characteristics, CCI, PBS, and APACHE II scores. The rates of complete response/cure and 14-day survival were relatively higher in the combination group compared to the monotherapy group (46.3 % vs. 30.6 % and 68.2 % vs. 55.5 %, respectively), and microbiological eradication was significantly much higher in the combination group than the monotherapy group (79.9 % vs. 55.6 %, p = 0.001). Also, the in-hospital mortality rate was significantly lower in the combination group compared to the monotherapy group (52.3 % vs. 72.2 %, p = 0.03) (Table 1). Therefore, we compared the three different combination groups with each other in terms of efficacy.
The baseline patient characteristics, bacteremia type (primary, secondary, or catheter-related BSI), and outcomes of 214 cases with XDR-ABSI, according to the three different combination modalities, are demonstrated in Table 2. The mean duration of hemoculture positivity was 5.29 ± 3.21 days, and it did not differ significantly between the three groups (p = 0.27). Catheters had been withdrawn in 28 (96.5 %) cases with catheter-related BSI. All MIC values of colistin for Acinetobacter baumannii were less than 1 μg/ml.
A total of 128 (59 %) of the patients had another concomitant infection. The presence of any concomitant infection did not differ significantly between the three groups (p = 0.17). The primary sources of bacteremia are summarized in Table 3. The proportion of secondary bacteremia did not differ significantly between the three treatment groups (p = 0.3).
Effective antimicrobial treatment was initiated in the first 24 h of infection (i.e., early) in 152 (71 %) and after 24 h (i.e., late) in 62 (29 %) of the patients. Only 36 (16.7 %) of the patients developed nephrotoxicity under COL treatment; the COL dose was decreased in 29 (13.6 %) and discontinued in 7 (3 %). Because of unconsciousness/pharmacological sedation in 118 (55 %) patients, the neurological status could not be evaluated. Only 3 (0.14 %) patients among those with assessable neurological status had any neurotoxicity, but none of them had discontinuation of colistin therapy. The all-cause in-hospital crude mortality was 52.3 %. The rates of all-cause mortality ranged from 46.4 to 55.8 % in the three groups, being relatively lower in the CS group, but they were not statistically different between the groups (p = 0.44).
Prolonged hospital and ICU stay before XDR-ABSI were significant risk factors for 14-day mortality (p = 0.02 and p = 0.01, respectively). Neither the timing of initial effective treatment nor the presence of any concomitant infection was significant between the three combination groups (p = 0.38 and p = 0.17, respectively) or for 14-day survival (p = 0.7 and p = 0.8, respectively). No significant difference was observed regarding the clinical (p = 0.97) and microbiological (p = 0.92) outcomes and 14-day survival rates (p = 0.79) between the three groups. The PBS, APACHE II score (calculated in 169 patients), and CCI as risk-adjustment severity parameters were not significantly different between the three groups, while higher PBS, APACHE II score, and CCI were related to higher 14-day mortality (p = 0.02, p = 0.0001, and p = 0.0001, respectively) in the univariate analysis. Gender, concomitant other infection, initiation time of antibiotic treatment, nephrotoxicity, and neurotoxicity were not significant for 14-day survival (all p > 0.05) (Table 4). Multivariable analysis showed that PBS, age, and duration of ICU stay before XDR-ABSI were independent risk factors for 14-day mortality in patients with XDR-ABSI (p < 0.0001, p < 0.0001, and p = 0.001 respectively) (Table 5).
After PSM, 152 (78: colistin–carbapenem group, 43: colistin–sulbactam, 31: colistin plus other agent) patients remained in our data set and we repeated the survival analysis. The rates of 14-day survival, clinical outcome, microbiological eradication, and the independent risk factors for 14-day mortality did not change after PSM. The results before and after PSM are shown in Tables 4, 5, and 6. Only the length of hospital stay, which was significant for 14-day survival in the univariate analysis before PSM, became insignificant after PSM. However, the independent risk factors for 14-day mortality did not change after PSM in the multivariable analysis.
Discussion
As there has been a diversity of definitions in publications regarding MDR and PDR Acinetobacter and Pseudomonas [28], an international proposal for definitions of MDR, XDR, and PDR bacteria was published in 2012 [1]. We preferred to use the updated definitions of resistance in this manuscript, although the majority of the references we have cited used previous MDR definitions regarding resistance, as they were published before 2012.
Colistin has become the first-line treatment choice in XDR-ABSI. Although there is no proof that combination therapies including COL are superior to COL monotherapy in the treatment of XDR-ABSI, due to heteroresistance during COL monotherapy, rapid selection of resistance in some strains, and lower clinical efficacy, COL-based combinations are widely recommended [10–19]. This was confirmed in the first-step analysis of the present study, and colistin-based combinations were found to be significantly superior to colistin monotherapy in terms of efficacy and survival outcomes. We further compared the efficacies of three different combination groups.
Clinical studies comparing different combinations are very scarce in the literature. Data regarding synergy or combination of antimicrobials rely on in vitro or animal studies, whereas the results of in vitro and animal studies may not translate into clinical practice [29]. Even the same antimicrobial combinations have been reported to have different results, causing conflict [30, 31]. Despite a few studies reporting no benefit from combinations [32], the majority of studies highlight the superiority of combination therapy compared to monotherapy [10–19]. In a recently published randomized, clinical trial, although the all-cause 30-day mortality, infection-related death, and length of hospitalization were not statistically significant between the COL monotherapy group and the COL–rifampicin combination group, a significant increase of the microbiologic eradication rate was observed in the combination group [33]. The authors concluded that “increased rate of A. baumannii eradication with combination therapy could still imply a clinical benefit”. In addition, a commentary on this article has recently been published by Pogue and Kaye [34]. The authors concluded that, for the treatment of invasive infections caused by A. baumannii, combination therapy could not definitely be stated as unwarranted regarding the aforementioned study, but rifampicin was not an ideal agent to be combined with colistin. Furthermore, monotherapy leads to the development of high-level resistance through the overexpression of efflux pumps. The colistin–rifampicin combination has been shown to prevent the development of resistant mutants with available in vitro and in vivo data [35]. Also, in our study, the microbiologic eradication rate was significantly higher in the combination group compared to the monotherapy group, but it was not statistically different between the three combination groups. Only three patients had received a colistin–rifampicin combination.
As the literature lacks clinical data about better and more effective combinations, we further designed our study to reply to the question: Which combination would be clinically optimal in the treatment of XDR-ABSI? This multicenter study included quite a large number of patients with XDR-ABSI, and the study groups were adjusted for clinical severity indices and comorbidities. Furthermore, PSM analysis was performed to adjust for all confounding variables.
In clinical practice, the safety profile, potential to induce resistance selection or collateral damage, cost of drug(s), and, also, the local antimicrobial usage strategy should be taken into consideration while deciding on combination therapy. Despite recommendations on the use of carbapenem-based combinations in the treatment of MDR-ABSI because of synergistic activity, the widespread use of carbapenems has been reported to cause increased selection of carbapenem-resistant strains [36]. Carbapenem use had been significantly associated with increased incidence of carbapenem-resistant A. baumannii [37]. A very recently published study has reported a 2.24-fold decrease in the prevalence of infections due to MDR A. baumannii strains achieved after implementing a policy of restricted carbapenem use in the ICU [38]. In addition to resistance selection, widespread carbapenem use may result in more frequent adverse effects/collateral damage and increased therapeutic costs. When the indifferent therapeutic results of the three COL-based combination groups in our study are considered, a carbapenem-sparing regimen including an antimicrobial agent with the lowest cost and risk of collateral damage should be preferred.
Sulbactam has moderate bacteriostatic activity, even against imipenem-resistant Acinetobacter isolates. Though not recommended as monotherapy in severe infections [39], it is a reasonable option for combined regimens. The COL–sulbactam combination revealed high in vitro synergistic activity against imipenem-resistant Acinetobacter, particularly in COL-resistant strains [40].
The CO group in our study included combinations of COL–TIG, COL–AG, and COL–RIF. The COL–TIG combination (24/43) has shown synergistic activity against XDR A. baumannii strains in in vitro studies [41]. Nevertheless, due to low plasma concentrations, TIG is disadvantageous in bacteremic patients.
When the outcomes and 14-day survival rates of combined regimens were evaluated separately or cumulatively, CC and CS combinations did not differ significantly. For the CO group, due to the relatively low numbers of cases in each treatment subgroup, it is difficult to comment on the treatment outcomes. In vitro studies including those combinations also reported similar results [10–12, 21, 39].
The presence of confounding factors such as various underlying diseases or severities of the infection due to patient factors, delays in diagnostic procedures, and onset of proper treatment were significant impediments that complicate comparing the efficacies of combined antimicrobial regimens in XDR-ABSI. Concerning the major importance of these confounders, we have made risk/severity adjustments, as the mean values of the CCI, PBS, and APACHE II score did not significantly differ between monotherapy, the combination therapy group as a whole, or the three different combination groups.
In the univariate analysis of predictors of 14-day survival, the age of the patient, PBS, CCI, APACHE II score, and length of stay in hospital and in the ICU before the diagnosis of XDR-ABSI were found to be significant. In the multivariable analysis, age, PBS, and length of ICU stay were independent predictors of 14-day survival. Older age (>50 years) has been reported to be significantly associated with increased mortality [42]. In similar clinical studies, the CCI, APACHE II score, and PBS had been used for adjustment of the severity of underlying comorbidities, clinical status, and bacteremia, and all severity assessment tools have been reported as independent risk factors for mortality [25, 43]. High APACHE II score (≥21) in patients with MDR-ABSI has been reported to be an independent risk factor for 14-/30-day or in-hospital mortality in various studies [24, 32, 37].
The all-cause in-hospital mortality is usually high in patients with MDR- and/or XDR-ABSI due to the coexistence of comorbidities and high clinical severity scores. In our study, the duration of hospital and ICU stay of patients before the diagnosis of XDR-ABSI was significantly associated with survival, as MDR- and XDR-ABSI usually develops in patients with longer durations of hospital or ICU stay and prolongs the duration of hospital stay even more. The length of hospital stay before the diagnosis of bacteremia has been reported to be longer in patients with carbapenem-resistant Acinetobacter bacteremia and has been a predictor of mortality [44].
Before making any conclusions, we should declare some limitations of our study. Its retrospective design seems to be the basic limitation of our study. We were not able to measure the concentrations of formed colistin and other antibiotics in the plasma of these patients. There might be suboptimal exposure to the antibiotics in blood. Colistin population analysis profiles of these isolates were not examined. Also, pharmacokinetics and pharmacodynamics must be considered when examining the efficacy of antibiotic combinations. Other limitations were the presence of concomitant foci of infections other than XDR-ABSI and the use of other drugs for concomitant infections in some patients, unstandardized doses of colistin use, and inadequate data about effective source control because of the retrospective design. Because of ethical concerns, it is very difficult to conduct prospective clinical trials on this issue. Besides, we think that the results of our study, which included a remarkable number of cases, would provide significant benefits in making a decision on the therapeutic choices in XDR-ABSI. To our knowledge, this is the first study comparing monotherapy and combination therapy where three severity assessment tools (CCI, APACHE II score, and PBS) have been used for the adjustment of clinical severities of patients. Furthermore, PSM analysis was performed to adjust for all confounding variables.
In conclusion, the rates of cure and 14-day survival were relatively higher in the combination group compared to the monotherapy group, and the microbiological eradication rate was significantly much higher in the combination group than the monotherapy group. Also, the in-hospital crude mortality rate was significantly lower in the combination group compared to the monotherapy group. Colistin-based combinations with CC, CS, and CO for XDR-ABSI did not reveal significant differences with respect to the 14-day survival, clinical response, or microbiological outcome. PBS, age, and length of ICU stay were found to be independent risk factors for 14-day mortality before and after PSM. Although the outcomes of the combination treatment groups did not differ significantly, colistin–sulbactam may be a suggestible and more favorable combination. Carbapenem-sparing combinations may be preferable in the treatment of Acinetobacter infections to prevent collateral damage, particularly resistance selection and to decrease the prevalence of Acinetobacter infections. Well-designed controlled prospective clinical trials are needed in order to determine the optimal antimicrobial therapy in critically ill patients with XDR-ABSI.
References
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281
Vila J, Pachón J (2008) Therapeutic options for Acinetobacter baumannii infections. Expert Opin Pharmacother 9(4):587–599
Falagas ME, Karveli EA, Siempos II, Vardakas KZ (2008) Acinetobacter infections: a growing threat for critically ill patients. Epidemiol Infect 136(8):1009–1019
Erbay A, Idil A, Gözel MG, Mumcuoğlu I, Balaban N (2009) Impact of early appropriate antimicrobial therapy on survival in Acinetobacter baumannii bloodstream infections. Int J Antimicrob Agents 34(6):575–579
Kim YJ, Kim SI, Hong KW, Kim YR, Park YJ, Kang MW (2012) Risk factors for mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteremia: impact of appropriate antimicrobial therapy. J Korean Med Sci 27(5):471–475
Kallel H, Bahloul M, Hergafi L, Akrout M, Ketata W, Chelly H, Hamida CB, Rekik N, Hammami A, Bouaziz M (2006) Colistin as a salvage therapy for nosocomial infections caused by multidrug-resistant bacteria in the ICU. Int J Antimicrob Agents 28(4):366–369
Li J, Rayner CR, Nation RL, Owen RJ, Spelman D, Tan KE, Liolios L (2006) Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother 50(9):2946–2950
Rahal JJ (2006) Novel antibiotic combinations against infections with almost completely resistant Pseudomonas aeruginosa and Acinetobacter species. Clin Infect Dis 43(Suppl 2):S95–S99
Petrosillo N, Chinello P, Proietti MF, Cecchini L, Masala M, Franchi C, Venditti M, Esposito S, Nicastri E (2005) Combined colistin and rifampicin therapy for carbapenem-resistant Acinetobacter baumannii infections: clinical outcome and adverse events. Clin Microbiol Infect 11(8):682–683
Pantopoulou A, Giamarellos-Bourboulis EJ, Raftogannis M, Tsaganos T, Dontas I, Koutoukas P, Baziaka F, Giamarellou H, Perrea D (2007) Colistin offers prolonged survival in experimental infection by multidrug-resistant Acinetobacter baumannii: the significance of co-administration of rifampicin. Int J Antimicrob Agents 29(1):51–55
Montero A, Ariza J, Corbella X, Doménech A, Cabellos C, Ayats J, Tubau F, Borraz C, Gudiol F (2004) Antibiotic combinations for serious infections caused by carbapenem-resistant Acinetobacter baumannii in a mouse pneumonia model. J Antimicrob Chemother 54(6):1085–1091
Saballs M, Pujol M, Tubau F, Peña C, Montero A, Domínguez MA, Gudiol F, Ariza J (2006) Rifampicin/imipenem combination in the treatment of carbapenem-resistant Acinetobacter baumannii infections. J Antimicrob Chemother 58(3):697–700
Rodríguez-Hernández MJ, Pachón J, Pichardo C, Cuberos L, Ibáñez-Martínez J, García-Curiel A, Caballero FJ, Moreno I, Jiménez-Mejías ME (2000) Imipenem, doxycycline and amikacin in monotherapy and in combination in Acinetobacter baumannii experimental pneumonia. J Antimicrob Chemother 45(4):493–501
Bernabeu-Wittel M, Pichardo C, García-Curiel A, Pachón-Ibáñez ME, Ibáñez-Martínez J, Jiménez-Mejías ME, Pachón J (2005) Pharmacokinetic/pharmacodynamic assessment of the in-vivo efficacy of imipenem alone or in combination with amikacin for the treatment of experimental multiresistant Acinetobacter baumannii pneumonia. Clin Microbiol Infect 11(4):319–325
Haddad FA, Van Horn K, Carbonaro C, Aguero-Rosenfeld M, Wormser GP (2005) Evaluation of antibiotic combinations against multidrug-resistant Acinetobacter baumannii using the E-test. Eur J Clin Microbiol Infect Dis 24(8):577–579
Ko WC, Lee HC, Chiang SR, Yan JJ, Wu JJ, Lu CL, Chuang YC (2004) In vitro and in vivo activity of meropenem and sulbactam against a multidrug-resistant Acinetobacter baumannii strain. J Antimicrob Chemother 53(2):393–395
Kiffer CR, Sampaio JL, Sinto S, Oplustil CP, Koga PC, Arruda AC, Turner PJ, Mendes C (2005) In vitro synergy test of meropenem and sulbactam against clinical isolates of Acinetobacter baumannii. Diagn Microbiol Infect Dis 52(4):317–322
Sobieszczyk ME, Furuya EY, Hay CM, Pancholi P, Della-Latta P, Hammer SM, Kubin CJ (2004) Combination therapy with polymyxin B for the treatment of multidrug-resistant Gram-negative respiratory tract infections. J Antimicrob Chemother 54(2):566–569
Kasiakou SK, Michalopoulos A, Soteriades ES, Samonis G, Sermaides GJ, Falagas ME (2005) Combination therapy with intravenous colistin for management of infections due to multidrug-resistant Gram-negative bacteria in patients without cystic fibrosis. Antimicrob Agents Chemother 49(8):3136–3146
Bassetti M, Repetto E, Righi E, Boni S, Diverio M, Molinari MP, Mussap M, Artioli S, Ansaldi F, Durando P, Orengo G, Bobbio Pallavicini F, Viscoli C (2008) Colistin and rifampicin in the treatment of multidrug-resistant Acinetobacter baumannii infections. J Antimicrob Chemother 61(2):417–420
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Chow JW, Yu VL (1999) Combination antibiotic therapy versus monotherapy for gram-negative bacteraemia: a commentary. Int J Antimicrob Agents 11(1):7–12
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13(10):818–829
Chen SJ, Chao TF, Chiang MC, Kuo SC, Chen LY, Yin T, Chen TL, Fung CP (2011) Prediction of patient outcome from Acinetobacter baumannii bacteremia with Sequential Organ Failure Assessment (SOFA) and Acute Physiology and Chronic Health Evaluation (APACHE) II scores. Intern Med 50(8):871–877
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8(4):R204–R212
Spapen H, Jacobs R, Van Gorp V, Troubleyn J, Honoré PM (2011) Renal and neurological side effects of colistin in critically ill patients. Ann Intensive Care 1(1):14
Falagas ME, Koletsi PK, Bliziotis IA (2006) The diversity of definitions of multidrug-resistant (MDR) and pandrug-resistant (PDR) Acinetobacter baumannii and Pseudomonas aeruginosa. J Med Microbiol 55(Pt 12):1619–1629
Fowler RA, Flavin KE, Barr J, Weinacker AB, Parsonnet J, Gould MK (2003) Variability in antibiotic prescribing patterns and outcomes in patients with clinically suspected ventilator-associated pneumonia. Chest 123(3):835–844
Vouillamoz J, Moreillon P, Giddey M, Entenza JM (2008) In vitro activities of tigecycline combined with other antimicrobials against multiresistant gram-positive and gram-negative pathogens. J Antimicrob Chemother 61(2):371–374
Principe L, D’Arezzo S, Capone A, Petrosillo N, Visca P (2009) In vitro activity of tigecycline in combination with various antimicrobials against multidrug resistant Acinetobacter baumannii. Ann Clin Microbiol Antimicrob 8:18
Falagas ME, Rafailidis PI, Ioannidou E, Alexiou VG, Matthaiou DK, Karageorgopoulos DE, Kapaskelis A, Nikita D, Michalopoulos A (2010) Colistin therapy for microbiologically documented multidrug-resistant Gram-negative bacterial infections: a retrospective cohort study of 258 patients. Int J Antimicrob Agents 35(2):194–199
Durante-Mangoni E, Signoriello G, Andini R, Mattei A, De Cristoforo M, Murino P, Bassetti M, Malacarne P, Petrosillo N, Galdieri N, Mocavero P, Corcione A, Viscoli C, Zarrilli R, Gallo C, Utili R (2013) Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: a multicenter, randomized clinical trial. Clin Infect Dis 57(3):349–358
Pogue JM, Kaye KS (2013) Is there really no benefit to combination therapy with colistin? Expert Rev Anti Infect Ther 11(9):881–884
Gauthier TP (2013) Editorial commentary: rifampicin plus colistin in the era of extensively drug-resistant Acinetobacter baumannii infections. Clin Infect Dis 57(3):359–361
Song JY, Cheong HJ, Choi WS, Heo JY, Noh JY, Kim WJ (2011) Clinical and microbiological characterization of carbapenem-resistant Acinetobacter baumannii bloodstream infections. J Med Microbiol 60(Pt 5):605–611
Kuo SC, Lee YT, Yang SP, Chiang MC, Lin YT, Tseng FC, Chen TL, Fung CP (2013) Evaluation of the effect of appropriate antimicrobial therapy on mortality associated with Acinetobacter nosocomialis bacteraemia. Clin Microbiol Infect 19(7):634–639
Ogutlu A, Guclu E, Karabay O, Utku AC, Tuna N, Yahyaoglu M (2014) Effects of Carbapenem consumption on the prevalence of Acinetobacter infection in intensive care unit patients. Ann Clin Microbiol Antimicrob 13(1):7
Deveci A, Coban AY, Acicbe O, Tanyel E, Yaman G, Durupinar B (2012) In vitro effects of sulbactam combinations with different antibiotic groups against clinical Acinetobacter baumannii isolates. J Chemother 24(5):247–252
Cıkman A, Ceylan MR, Parlak M, Karahocagil MK, Berktaş M (2013) Evaluation of colistin–ampicillin/sulbactam combination efficacy in imipenem-resistant Acinetobacter baumannii strains. Mikrobiyol Bul 47(1):147–151
Dizbay M, Tozlu DK, Cirak MY, Isik Y, Ozdemir K, Arman D (2010) In vitro synergistic activity of tigecycline and colistin against XDR-Acinetobacter baumannii. J Antibiot (Tokyo) 63(2):51–53
Michalopoulos A, Falagas ME, Karatza DC, Alexandropoulou P, Papadakis E, Gregorakos L, Chalevelakis G, Pappas G (2011) Epidemiologic, clinical characteristics, and risk factors for adverse outcome in multiresistant gram-negative primary bacteremia of critically ill patients. Am J Infect Control 39(5):396–400
Tseng YC, Wang JT, Wu FL, Chen YC, Chie WC, Chang SC (2007) Prognosis of adult patients with bacteremia caused by extensively resistant Acinetobacter baumannii. Diagn Microbiol Infect Dis 59(2):181–190
Sunenshine RH, Wright MO, Maragakis LL, Harris AD, Song X, Hebden J, Cosgrove SE, Anderson A, Carnell J, Jernigan DB, Kleinbaum DG, Perl TM, Standiford HC, Srinivasan A (2007) Multidrug-resistant Acinetobacter infection mortality rate and length of hospitalization. Emerg Infect Dis 13(1):97–103
Conflict of interest
None to declare.
Funding
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Batirel, A., Balkan, I.I., Karabay, O. et al. Comparison of colistin–carbapenem, colistin–sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis 33, 1311–1322 (2014). https://doi.org/10.1007/s10096-014-2070-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2070-6