Abstract
Purpose
The benefit of tranexamic acid (TXA) in pediatric cardiac surgery on postoperative bleeding has varied among studies. It is also unclear whether the effects of TXA differ between cyanotic patients and acyanotic patients. The aim of this study was to test the benefit of TXA in pediatric cardiac surgery in a well-balanced study population of cyanotic and acyanotic patients.
Methods
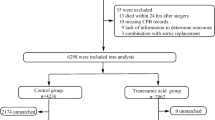
A total of 160 pediatric patients undergoing cardiac surgery with cardiopulmonary bypass (81 cyanotic, 79 acyanotic) were included in this single-blinded, randomized trial at a tertiary care university-affiliated teaching hospital. Eighty-one children (41 cyanotic, 40 acyanotic) were randomly assigned to a TXA group, in which they received 50 mg/kg of TXA as a bolus followed by 15 mg/kg/h infusion and another 50 mg/kg into the bypass circuit. The other 79 patients were randomly assigned to a placebo group. The primary end point was the amount of 24-h blood loss.
Results
The amount of 24-h blood loss was significantly less in the TXA group than in the placebo group [mean (95% confidence interval): 18.6 (15.8–21.4) vs. 23.5 (19.4–27.5) ml/kg, respectively; mean difference −4.9 (−9.7 to −0.01) ml/kg; p = 0.049]. This effect of TXA was already significant at 6 h [9.5 (7.5–11.5) vs. 13.2 (10.6–15.9) ml/kg, respectively; mean difference −3.47 (−7.0 to −0.4) ml/kg; p = 0.027]. However, there was no significant difference in the amount of blood transfusion between the groups. There was also no statistical difference in the effect of TXA in each cyanotic and acyanotic subgroup.
Conclusion
TXA can reduce blood loss in pediatric cardiac surgery but not the transfusion requirement (http://ClinicalTrials.gov number NCT00994994).



Similar content being viewed by others
References
Belisle S, Hardy JF. Hemorrhage and the use of blood products after adult cardiac operations: myths and realities. Ann Thorac Surg. 1996;62:1908–17.
Petaja J, Lundstrom U, Leijala M, Peltola K, Siimes MA. Bleeding and use of blood products after heart operations in infants. J Thorac Cardiovasc Surg. 1995;109:524–9.
Manno CS, Hedberg KW, Kim HC, Bunin GR, Nicolson S, Jobes D, Schwartz E, Norwood WI. Comparison of the hemostatic effects of fresh whole blood, stored whole blood, and components after open heart surgery in children. Blood. 1991;77:930–6.
Kneyber MC, Hersi MI, Twisk JW, Markhorst DG, Plotz FB. Red blood cell transfusion in critically ill children is independently associated with increased mortality. Intensive Care Med. 2007;33:1414–22.
Miller BE, Guzzetta NA, Tosone SR, Levy JH. Rapid evaluation of coagulopathies after cardiopulmonary bypass in children using modified thromboelastography. Anesth Analg. 2000;90:1324–30.
Eisses MJ, Chandler WL. Cardiopulmonary bypass parameters and hemostatic response to cardiopulmonary bypass in infants versus children. J Cardiothorac Vasc Anesth. 2008;22:53–9.
Williams GD, Bratton SL, Riley EC, Ramamoorthy C. Association between age and blood loss in children undergoing open heart operations. Ann Thorac Surg. 1998;66:870–5. (discussion 5–6).
Ekert H, Gilchrist GS, Stanton R, Hammond D. Hemostasis in cyanotic congenital heart disease. J Pediatr. 1970;76:221–30.
Williams GD, Bratton SL, Nielsen NJ, Ramamoorthy C. Fibrinolysis in pediatric patients undergoing cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 1998;12:633–8.
Eaton MP. Antifibrinolytic therapy in surgery for congenital heart disease. Anesth Analg. 2008;106:1087–100.
Bulutcu FS, Ozbek U, Polat B, Yalçin Y, Karaci AR, Bayindir O. Which may be effective to reduce blood loss after cardiac operations in cyanotic children: tranexamic acid, aprotinin or a combination? Paediatr Anaesth. 2005;15:41–6.
Chauhan S, Das SN, Bisoi A, Kale S, Kiran U. Comparison of epsilon aminocaproic acid and tranexamic acid in pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:141–3.
Chauhan S, Bisoi A, Kumar N, Mittal D, Kale S, Kiran U, Venugopal P. Dose comparison of tranexamic acid in pediatric cardiac surgery. Asian Cardiovasc Thorac Ann. 2004;12:121–4.
Chauhan S, Bisoi A, Modi R, Gharde P, Rajesh MR. Tranexamic acid in paediatric cardiac surgery. Indian J Med Res. 2003;118:86–9.
Levin E, Wu J, Devine DV, Alexander J, Reichart C, Sett S, Seear M. Hemostatic parameters and platelet activation marker expression in cyanotic and acyanotic pediatric patients undergoing cardiac surgery in the presence of tranexamic acid. Thromb Haemost. 2000;83:54–9.
Reid RW, Zimmerman AA, Laussen PC, Mayer JE, Gorlin JB, Burrows FA. The efficacy of tranexamic acid versus placebo in decreasing blood loss in pediatric patients undergoing repeat cardiac surgery. Anesth Analg. 1997;84:990–6.
Zonis Z, Seear M, Reichert C, Sett S, Allen C. The effect of preoperative tranexamic acid on blood loss after cardiac operations in children. J Thorac Cardiovasc Surg. 1996;111:982–7.
Mauer HM, McCue CM, Caul J, Still WJ. Impairment in platelet aggregation in congenital heart disease. Blood. 1972;40:207–16.
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123:110–8.
Dowd NP, Karski JM, Cheng DC, Carroll JA, Lin Y, James RL, Butterworth J. Pharmacokinetics of tranexamic acid during cardiopulmonary bypass. Anesthesiology. 2002;97:390–9.
Martin K, Wiesner G, Breuer T, Lange R, Tassani P. The risks of aprotinin and tranexamic acid in cardiac surgery: a one-year follow-up of 1188 consecutive patients. Anesth Analg. 2008;107:1783–90.
Murkin JM, Falter F, Granton J, Young B, Burt C, Chu M. High-dose tranexamic acid is associated with nonischemic clinical seizures in cardiac surgical patients. Anesth Analg. 2010;110:350–3.
Miller BE, Mochizuki T, Levy JH, Bailey JM, Tosone SR, Tam VK, Kanter KR. Predicting and treating coagulopathies after cardiopulmonary bypass in children. Anesth Analg. 1997;85:1196–202.
Kern FH, Morana NJ, Sears JJ, Hickey PR. Coagulation defects in neonates during cardiopulmonary bypass. Ann Thorac Surg. 1992;54:541–6.
Petaja J, Peltola K, Sairanen H, Leijala M, Kekomaki R, Vahtera E, Siimes MA. Fibrinolysis, antithrombin III, and protein C in neonates during cardiac operations. J Thorac Cardiovasc Surg. 1996;112:665–71.
Williams GD, Bratton SL, Ramamoorthy C. Factors associated with blood loss and blood product transfusions: a multivariate analysis in children after open-heart surgery. Anesth Analg. 1999;89:57–64.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shimizu, K., Toda, Y., Iwasaki, T. et al. Effect of tranexamic acid on blood loss in pediatric cardiac surgery: a randomized trial. J Anesth 25, 823–830 (2011). https://doi.org/10.1007/s00540-011-1235-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1235-z