Abstract
Purpose
In oncology patients, hospital malnutrition is associated with a greater risk of morbidity and mortality. The objective of this study was to determine the prevalence of nutritional risk and the clinical and economic consequences of hospital malnutrition in oncology patients hospitalised in Spanish centres.
Methods
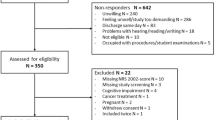
This was an observational, cross-sectional, multicentre study. The prevalence of nutritional risk was determined using the Nutrition Risk Screening®-2002 (NRS®-2002).
Results
Four hundred one oncology patients were included; 33.9 % (136/401) were at nutritional risk (NRS®-2002 ≥ 3) at admission and 36.4 % (135/371) at discharge. On average, patients at nutritional risk were more elderly and had lower weights, body mass indices and arm and calf circumferences, as well as lower serum albumin levels than patients not at risk. Mean duration of hospitalisation and healthcare costs were greater in patients at nutritional risk at discharge (12.1 days; 95 % confidence interval (CI) 10.83–13.39) than in well-nourished patients (8.6 days; 95 % CI 7.86–9.40). Only a third of the patients at risk of malnutrition at discharge had received any kind of nutritional support.
Conclusions
This study shows that hospital malnutrition is a prevalent and undertreated condition in oncology patients that is associated with longer hospital stays and increased healthcare costs.


Similar content being viewed by others
References
Norman K, Pichard C, Lochs H, Pirlich M (2008) Prognostic impact of disease-related malnutrition. Clin Nutr 27(1):5–15
Correia MI, Hegazi RA, Higashiguchi T, Michel JP, Reddy BR, Tappenden KA, Uyar M, Muscaritoli M (2014) Evidence-based recommendations for addressing malnutrition in health care: an updated strategy from the feedM.E. Global Study Group. J Am Med Dir Assoc 15(8):544–550
Kwag SJ, Kim JG, Kang WK, Lee JK, Oh ST (2014) The nutritional risk is an independent factor for postoperative morbidity in surgery for colorectal cancer. Ann Surg Treat Res 86(4):206–211
Yu K, Zhou XR, He SL (2013) A multicentre study to implement nutritional risk screening and evaluate clinical outcome and quality of life in patients with cancer. Eur J Clin Nutr 67(7):732–737
Vashi PG, Gupta D, Lammersfeld CA, Braun DP, Popiel B, Misra S, Brown KC (2013) The relationship between baseline nutritional status with subsequent parenteral nutrition and clinical outcomes in cancer patients undergoing hyperthermic intraperitoneal chemotherapy. Nutr J 12:118
Nitenberg G, Raynard B (2000) Nutritional support of the cancer patient: issues and dilemmas. Crit Rev Oncol Hematol 34(3):137–168
Fiorelli A, Vicidomini G, Mazzella A, Messina G, Milione R, Di Crescenzo VG, Santini M (2014) The influence of body mass index and weight loss on outcome of elderly patients undergoing lung cancer resection. Thorac Cardiovasc Surg 62(7):578–587
Rey-Ferro M, Castaño R, Orozco O, Serna A, Moreno A (1997) Nutritional and immunologic evaluation of patients with gastric cancer before and after surgery. Nutrition 13(10):878–881
Gupta D, Lis CG, Granick J, Grutsch JF, Vashi PG, Lammersfeld CA (2006) Malnutrition was associated with poor quality of life in colorectal cancer: a retrospective analysis. J Clin Epidemiol 59(7):704–709
Jager-Wittenaar H, Dijkstra PU, Vissink A, van der Laan BF, van Oort RP, Roodenburg JL (2011) Malnutrition and quality of life in patients treated for oral or oropharyngeal cancer. Head Neck 33(4):490–496
Lis CG, Gupta D, Lammersfeld CA, Markman M, Vashi PG (2012) Role of nutritional status in predicting quality of life outcomes in cancer—a systematic review of the epidemiological literature. Nutr J 11:27
Ma L, Wu T, Pan J, Kong X, Guo Q, Yang L, Zhang Y, Lin S, Chen C, Huang C (2014) The correlation between the comprehensive nutrition index and quality of life of patients with nasopharyngeal carcinoma treated by intensity-modulated radiotherapy. Nutr Cancer 66(1):152–158
Van Cutsem E, Arends J (2005) The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs 9(Suppl 2):S51–S63
Nicolini A, Ferrari P, Masoni MC, Fini M, Pagani S, Giampietro O, Carpi A (2013) Malnutrition, anorexia and cachexia in cancer patients: a mini-review on pathogenesis and treatment. Biomed Pharmacother 67(8):807–817
Von Haehling S, Anker SD (2010) Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachex Sarcopenia Muscle 1(1):1–5
Tong H, Isenring E, Yates P (2009) The prevalence of nutrition impact symptoms and their relationship to quality of life and clinical outcomes in medical oncology patients. Support Care Cancer 17(1):83–90
Olsson U, Bosaeus I, Svedlund J, Bergbom I (2007) Patients’ subjective symptoms, quality of life and intake of food during the recovery period 3 and 12 months after upper gastrointestinal surgery. Eur J Cancer Care (Engl) 16(1):74–85
Russi EG, Raber-Durlacher JE, Sonis ST (2014) Local and systemic pathogenesis and consequences of regimen-induced inflammatory responses in patients with head and neck cancer receiving chemoradiation. Mediat Inflamm 2014:518261
Silver HJ, Dietrich MS, Murphy BA (2007) Changes in body mass, energy balance, physical function, and inflammatory state in patients with locally advanced head and neck cancer treated with concurrent chemoradiation after low-dose induction chemotherapy. Head Neck 29(10):893–900
Baldwin C, McGough C, Spiro A, Thomas K, Cunningham DC, Andreyev HJN (2009) Nutritional and clinical characteristics of patients with gastrointestinal tract (GI) cancers at presentation. Proceedings of the Nutrition Society 68(OCE1)
Andreyev HJ, Norman AR, Oates J, Cunningham D (1998) Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies? Eur J Cancer 34(4):503–509
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, Cohen MH, Douglass Jr HO, Engstrom PF, Ezdinli EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW, Tormey DC (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 69(4):491–497
Segura A, Pardo J, Jara C, Zugazabeitia L, Carulla J, de Las PR, García-Cabrera E, Luz Azuara M, Casadó J, Gómez-Candela C (2005) An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin Nutr 24(5):801–814
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M (2003) Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr 22(4):415–421
Álvarez-Hernández J, Planas Vila M, León-Sanz M, García de Lorenzo A, Celaya-Pérez S, García-Lorda P, Araujo K, Sarto Guerri B (2012) PREDyCES researchers. Prevalence and costs of malnutrition in hospitalized patients; the PREDyCES study. Nutr Hosp 27(4):1049–1059
Planas Vila M, Álvarez Hernández J, García de Lorenzo A, Celaya Pérez S, León Sanz M, García-Lorda P, Brosa M (2010) The burden of hospital malnutrition in Spain: methods and development of the PREDyCES® study. Nutr Hosp 25(6):1020–1024
Olivares J, Ayala L, Salas-Salvadó J, Muñiz MJ, Gamundí A, Martínez-Indart L, Masmiquel LL (2014) Assessment of risk factors and test performance on malnutrition prevalence at admission using four different screening tools. Nutr Hosp 29(3):674–680
Mercadal-Orfila G, Lluch-Taltavull J, Campillo-Artero C, Torrent-Quetglas M (2012) Association between nutritional risk based on the NRS-2002 test and hospital morbidity and mortality. Nutr Hosp 27(4):1248–1254
Velasco C, García E, Rodríguez V, Frias L, Garriga R, Alvarez J, García-Peris P, León M (2011) Comparison of four nutritional screening tools to detect nutritional risk in hospitalized patients: a multicentre study. Eur J Clin Nutr 65(2):269–274
Gur AS, Atahan K, Aladag I, Durak E, Cokmez A, Tarcan E, Tavusbay C (2009) The efficacy of Nutrition Risk Screening-2002 (NRS-2002) to decide on the nutritional support in general surgery patients. Bratisl Lek Listy 110(5):290–292
Bozzetti F, Mariani L, Lo Vullo S, SCRINIO Working Group, Amerio ML, Biffi R, Caccialanza G, Capuano G, Correja I, Cozzaglio L, Di Leo A, Di Cosmo L, Finocchiaro C, Gavazzi C, Giannoni A, Magnanini P, Mantovani G, Pellegrini M, Rovera L, Sandri G, Tinivella M, Vigevani E (2012) The nutritional risk in oncology: a study of 1,453 cancer outpatients. Support Care Cancer 20(8):1919–1928
Gheorghe C, Pascu O, Iacob R, Vadan R, Iacob S, Goldis A, Tantau M, Dumitru E, Dobru D, Miutescu E, Saftoiu A, Fraticiu A, Tomescu D, Gheorghe L (2013) Nutritional risk screening and prevalence of malnutrition on admission to gastroenterology departments: a multicentric study. Chirurgia (Bucur) 108(4):535–541
Alvarez-Altamirano K, Delgadillo T, García-García A, Alatriste-Ortiz G, Fuchs-Tarlovsky V (2014) Prevalence of nutritional risk evaluated with nrs-2002 in Mexican oncology population. Nutr Hosp 30(1):173–178
Illa P, Tomíšková M, Skřičková J (2014) Screening of malnutrition risk versus indicators of nutritional status and systemic inflammatory response in newly diagnosed lung cancer patients]. Klin Onkol 27(4):261–268
Tangvik RJ, Tell GS, Guttormsen AB, Eisman JA, Henriksen A, Nilsen RM, Ranhoff AH (2014) Nutritional risk profile in a university hospital population. Clin Nutr S0261-5614(14)00205-00202. doi:10.1016/j.clnu.2014.08.001
Freijer K, Bours MJ, Nuijten MJ, Poley MJ, Meijers JM, Halfens RJ, Schols JM (2014) The economic value of enteral medical nutrition in the management of disease-related malnutrition: a systematic review. J Am Med Dir Assoc 15(1):17–29
Arends J, Bodoky G, Bozzetti F, Fearon K, Muscaritoli M, Selga G, van Bokhorst-de van der Schueren MA, von Meyenfeldt M, DGEM (German Society for Nutritional Medicine), Zürcher G, Fietkau R, Aulbert E, Frick B, Holm M, Kneba M, Mestrom HJ, Zander A (2006) ESPEN (European Society for Parenteral and Enteral Nutrition). ESPEN guidelines on enteral nutrition: non-surgical oncology. Clin Nutr 25(2):245–259
Bozzetti F, Arends J, Lundholm K, Micklewright A, Zurcher G, Muscaritoli M, ESPEN (2009) ESPEN guidelines on parenteral nutrition: non-surgical oncology. Clin Nutr 28(4):445–454
Bosch R, García A, Mañas A (2008) Guía clínica multidisciplinar sobre el manejo de la nutrición en el paciente con cáncer. http://www.oncologiaynutricion.com/archivos/pubs/libroconsenso.pdf. Accessed: 18 Mar 2015
Platek ME, Popp JV, Possinger CS, Denysschen CA, Horvath P, Brown JK (2011) Comparison of the prevalence of malnutrition diagnosis in head and neck, gastrointestinal, and lung cancer patients by 3 classification methods. Cancer Nurs 34(5):410–416
Pressoir M, Desné S, Berchery D, Rossignol G, Poiree B, Meslier M, Traversier S, Vittot M, Simon M, Gekiere JP, Meuric J, Serot F, Falewee MN, Rodrigues I, Senesse P, Vasson MP, Chelle F, Maget B, Antoun S, Bachmann P (2010) Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer 102(6):966–971
Amaral TF, Antunes A, Cabral S, Alves P, Kent-Smith L (2008) An evaluation of three nutritional screening tools in a Portuguese oncology centre. J Hum Nutr Diet 21(6):575–583
Gavazzi C, Colatruglio S, Sironi A, Mazzaferro V, Miceli R (2011) Importance of early nutritional screening in patients with gastric cancer. Br J Nutr 106(12):1773–1778
Takahashi H, Chiba T, Tairabune T, Kimura Y, Wakabayashi G, Takahashi K, Kudo K (2014) A retrospective study on the influence of nutritional status on pain management in cancer patients using the transdermal fentanyl patch. Biol Pharm Bull 37(5):853–857
Isenring EA, Capra S, Bauer JD (2004) Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer 91(3):447–452
Moreland SS (2012) Nutrition screening and counseling in patients with lung cancer in an outpatient setting. J Adv Pract Oncol 3(3):191–193
Tan CR, Yaffee PM, Jamil LH, Lo SK, Nissen N, Pandol SJ, Tuli R, Hendifar AE (2014) Pancreatic cancer cachexia: a review of mechanisms and therapeutics. Front Physiol 5:88
Acknowledgments
The authors would like to thank the economic support provided by Nestlé Health Science for the conduct of this study and the technical support provided by Oblikue Consulting in the analysis of results and drafting of this manuscript. The authors also thank all the investigators who participated in the PREDyCES® study for their kind collaboration.
Compliance with ethical standards
Funding
This study was sponsored by the Spanish Society for Parenteral and Enteral Nutrition (SENPE), with the technical support and funding from Nestlé Health Science.
Conflict of interest
The authors declare that the funding provider was not involved in analysing the results and preparing the conclusions of this study, and that no conflict of interest exists with the aforementioned organisations.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Planas, M., Álvarez-Hernández, J., León-Sanz, M. et al. Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES® study. Support Care Cancer 24, 429–435 (2016). https://doi.org/10.1007/s00520-015-2813-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2813-7