Abstract
Purpose
The aims of the study were (1) to understand the relationship between women’s marital coping efforts and body image as well as sexual relationships and (2) to test a hypothesized model suggesting that marital coping efforts have a mediating effect on the relationship between body image and sexual relationships among breast cancer survivors.
Methods
A total of 135 breast cancer survivors who had finished cancer treatment completed a self-reported questionnaire concerning body image, marital coping efforts, and sexual relationship.
Results
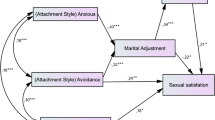
Body image, marital coping, and sexual relationship were found to be significantly correlated with each other. The final path model showed that negative marital coping efforts, including avoidance and self-blame, significantly mediated the effect of women’s body image on their sexual relationships. Although a positive approach did not correlate with body image, it did significantly correlate with women’s sexual relationships.
Conclusions
Our study demonstrated that negative marital coping using self-blame and avoidance mediated the association between body image and sexual relationship. Future interventions to address the body image and sexual life of breast cancer survivors should be considered using positive approaches that prevent disengaged avoidance or self-blame coping efforts intended to deal with marital stress.



Similar content being viewed by others
References
GLOBOCAN (2014) Estimated cancer incidence, mortality and prevalence worldwide in 2012. World Health Organization. http://globocan.iarc.fr/Pages/Editors.aspx. Accessed 22, Apr. 2014
Howlader N, Noone A, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse S, Kosary C, Ruhl J, Tatalovich Z (2011) SEER cancer statistics review, 1975–2008. Bethesda, MD: National Cancer Institute 19
Emilee G, Ussher J, Perz J (2010) Sexuality after breast cancer: a review. Maturitas 66(4):397–407
Hill EK, Sandbo S, Abramsohn E, Makelarski J, Wroblewski K, Wenrich ER, McCoy S, Temkin SM, Yamada SD, Lindau ST (2011) Assessing gynecologic and breast cancer survivors’ sexual health care needs. Cancer 117(12):2643–2651
Manganiello A, Hoga LAK, Reberte LM, Miranda CM, Rocha CAM (2011) Sexuality and quality of life of breast cancer patients post mastectomy. Eur J Oncol Nurs 15(2):167–172
Fobair P, Stewart SL, Chang S, D'Onofrio C, Banks PJ, Bloom JR (2006) Body image and sexual problems in young women with breast cancer. Psycho-oncology 15(7):579–594. doi:10.1002/pon.991
Berterö C, Wilmoth MC (2007) Breast cancer diagnosis and its treatment affecting the self: a meta-synthesis. Cancer Nurs 30(3):194–202
Andersen BL (2009) In sickness and in health: maintaining intimacy after breast cancer recurrence. Cancer J (Sudbury, Mass) 15(1):70
Garrusi B, Faezee H (2008) How do Iranian women with breast cancer conceptualize sex and body image? Sex Disabil 26(3):159–165
Speer JJ, Hillenberg B, Sugrue DP, Blacker C, Kresge CL, Decker VB, Zakalik D, Decker DA (2005) Study of sexual functioning determinants in breast cancer survivors. Breast J 11(6):440–447. doi:10.1111/j.1075-122X.2005.00131.x
Ganz PA, Desmond KA, Belin TR, Meyerowitz BE, Rowland JH (1999) Predictors of sexual health in women after a breast cancer diagnosis. J Clin Oncol: Off J Am Soc Clin Oncol 17(8):2371–2380
Reese JB, Keefe FJ, Somers TJ, Abernethy AP (2010) Coping with sexual concerns after cancer: the use of flexible coping. Support Care Cancer 18(7):785–800
Kinsinger SW, Laurenceau J-P, Carver CS, Antoni MH (2011) Perceived partner support and psychosexual adjustment to breast cancer. Psychol Health 26(12):1571–1588
Northouse LL, Katapodi MC, Schafenacker AM, Weiss D (2012) The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin Oncol Nurs 28(4):236–245
Kayser K, Scott JL (2008) Helping couples cope with women’s cancers, vol 229. Springer,
Skerrett K (1998) Couple adjustment to the experience of breast cancer. Families, systems, & health 16 (3):281
Zunkel G (2003) Relational coping processes: couples’ response to a diagnosis of early stage breast cancer. J Psychosoc Oncol 20(4):39–55
Krueger DW (2004) Psychodynamic perspectives on body image. In: Cash TF, Pruzinsky T (eds) Body image: a handbook of theory, research, and clinical practice. The Guilford Press, New York, pp 30–37
Crompvoets S (2006) Comfort, control, or conformity: women who choose breast reconstruction following mastectomy. Health Care Women Int 27(1):75–93. doi:10.1080/07399330500377531
Fang SY, Balneaves LG, Shu BC (2010) “A struggle between vanity and life”: the experience of receiving breast reconstruction in women of Taiwan. Cancer Nurs 33(5):E1–E11. doi:10.1097/NCC.0b013e3181d1c853
Yurek D, Farrar W, Andersen BL (2000) Breast cancer surgery: comparing surgical groups and determining individual differences in postoperative sexuality and body change stress. J Consult Clin Psychol 68(4):697–709
Badr H, Carmack CL, Kashy DA, Cristofanilli M, Revenson TA (2010) Dyadic coping in metastatic breast cancer. Health Psychol 29(2):169
Fang SY, Chang HT, Shu BC (2014) The links of objectified body consciousness, body image discomfort, and depressive symptoms among breast cancer survivors in Taiwan. Psychol Women Quart 38(4):563–574
Scott JL, Halford WK, Ward BG (2004) United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol 72(6):1122–1135. doi:10.1037/0022-006X.72.6.1122
Norton TR, Manne SL, Rubin S, Hernandez E, Carlson J, Bergman C, Rosenblum N (2005) Ovarian cancer patients’ psychological distress: the role of physical impairment, perceived unsupportive family and friend behaviors, perceived control, and self-esteem. Health Psychol: Off J Div Health Psychol Am Psychol Assoc 24(2):143–152. doi:10.1037/0278-6133.24.2.143
Bowman ML (1990) Coping efforts and marital satisfaction: measuring marital coping and its correlates. J Marriage Fam 52:463–474
Lee LJ (1997) Model testing of the process of marital coping behavior. J Chengchi Univ 74:53–94
Berglund G, Nystedt M, Bolund C, Sjödén P-O, Rutquist L-E (2001) Effect of endocrine treatment on sexuality in premenopausal breast cancer patients: a prospective randomized study. J Clin Oncol 19(11):2788–2796
Taylor‐Brown J, Kilpatrick M, Maunsell E, Dorval M (2000) Partner abandonment of women with breast cancer: myth or reality? Cancer Pract 8(4):160–164
Kline RB (2011) Principles and practice of structural equation modeling. The Guilford Press, London
Lt H, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model: Multidiscip J 6(1):1–55
Fu MR, Xu B, Liu Y, Haber J (2008) ‘Making the best of it’: Chinese women’s experiences of adjusting to breast cancer diagnosis and treatment. J Adv Nurs 63:155–165
Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, Clayton S, Williams I, Hills D (2004) Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-oncol 13:408–428
Giese-Davis J, Hermanson K, Koopman C, Weibel D, Spiegel D (2000) Quality of couples’ relationship and adjustment to metastatic breast cancer. J Fam Psychol 14(2):251
Scott JL, Kayser K (2009) A review of couple-based interventions for enhancing women's sexual adjustment and body image after cancer. Cancer J 15(1):48–56. doi:10.1097/PPO.1090b1013e31819585df
Anderson J, Gerbing D (1984) The effect of sampling error on convergence, improper solutions, and goodness-of-fit indices for maximum likelihood confirmatory factor analysis. Psychometrika 49(2):155–173
Bearden WO, Sharma S, Teel JE (1982) Sample size effects on chi square and other statistics used in evaluating causal models. J Mark Res 19(4):425–430
Bollen KA (1990) Overall fit in covariance structure models: two types of sample size effects. Psychol Bull 107(2):256–259
Iacobucci D (2010) Structural equations modeling: fit indices, sample size, and advanced topics. J Consum Psychol 20(1):90–98
Su CT, Ng HS, Yang AL, Lin CY (2014) Psychometric evaluation of the Short Form 36 Health Survey (SF-36) and the World Health Organization Quality of Life Scale Brief Version (WHOQOL-BREF) for patients with schizophrenia. Psychol Assess 26(3):980–989
Boquiren VM, Esplen MJ, Wong J, Toner B, Warner E (2013) Exploring the influence of gender‐role socialization and objectified body consciousness on body image disturbance in breast cancer survivors. Psycho‐Oncol 22:2177–2185
Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, Fox K (2004) Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. J Consult Clin Psychol 72(4):660–670. doi:10.1037/0022-006X.72.4.660
Acknowledgments
The authors are grateful for the Ditmanson Medical Foundation Chia-Yi Christian Hospital of Taiwan for its support of this study.
Conflict of interest
The authors declare that they have no conflict of interest. The authors have full control of all primary data and agree to allow the journal to review the data if required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fang, SY., Lin, YC., Chen, TC. et al. Impact of marital coping on the relationship between body image and sexuality among breast cancer survivors. Support Care Cancer 23, 2551–2559 (2015). https://doi.org/10.1007/s00520-015-2612-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2612-1