Abstract
Background
Mesh fixation during laparoscopic total extraperitoneal (TEP) inguinal hernia repair is still controversial. Although many surgeons considered it necessary to fix the mesh, some published studies supported elimination of mesh fixation. Therefore, a meta-analysis based on randomized controlled trials (RCTs) was conducted to compare the effectiveness and safety of fixation versus nonfixation of mesh in TEP.
Methods
RCTs were identified from PubMed, Embase, the Cochrane Library, SCI, and the Chinese Biomedical Literature Database (CBM). Two reviewers assessed the quality of the studies and extracted data independently. The methodological quality was evaluated according to the Cochrane Handbook 5.0.2. Statistical analysis was conducted using the Cochrane software RevMan 5.0.21.
Results
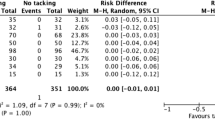
Six RCTs involving 772 patients were included. The nonfixation group had advantages in length of hospital stay [MD =−0.37, 95% CI (−0.57, −0.17), p = 0.0003], operative time [MD = −4.19, 95% CI (−7.77, −0.61), p = 0.02], and costs. However, there was no statistically significant difference in hernia recurrence [OR = 2.01, 95% CI (0.37, 11.03), p = 0.42], time to return to normal activities [MD = −0.13, 95% CI (−0.45, 0.19), p = 0.43], seroma [OR = 1.25, 95% CI (0.30, 5.18), p = 0.75], and postoperative pain on postoperative day 1 [MD = −0.21, 95% CI (−0.52, 0.10), p = 0.18] and day 7 [MD = −0.11, 95% CI (−0.42, 0.20), p = 0.47].
Conclusions
Without increasing the risk of early hernia recurrence, the nonfixation of mesh in TEP appears to be a safe alternative that is associated with less costs, shorter operative time, and hospital stay for the selected patients. Further adequately powered RCTs are required to clarify whether mesh fixation is necessary for the patients with different types of hernias and larger hernia defects.







Similar content being viewed by others
References
Zib M, Gani J (2002) Inguinal hernia repair: where to next? ANZ J Surg 72:573–579
Jacobs DO (2004) Mesh repair of inguinal hernias–redux. N Engl J Med 350:1895–1897
Kingsnorth AN, Gray MR, Nott DM (1992) Prospective randomized trial comparing the Shouldice technique and plication darn for inguinal hernia. Br J Surg 79:1068–1070
Levard H, Boudet MJ, Hennet H, Hay BM (1996) Inguinal hernia repair: a prospective multicentre trial on 1706 hernias. Br J Surg 83(Suppl 2):72
Fitzgibbons RJ Jr, Camps J, Cornet DA, Nguyen NX, Litke BS, Annibali R, Salerno GM (1995) Laparoscopic inguinal herniorrhaphy. Results of a multicenter trial. Ann Surg 221:3–13
Cheah WK, So JB, Lomanto D (2004) Endoscopic extraperitoneal inguinal hernia repair: a series of 182 repairs. Singapore Med J 45:267–270
Felix EL, Michas CA, Gonzalez MH Jr (1995) Laparoscopic hernioplasty. TAPP vs TEP. Surg Endosc 9:984–989
Read RC (2003) Recent advances in the repair of groin herniation. Curr Probl Surg 40:13–79
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD004703
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Deans GT, Wilson MS, Royston CM, Brough WA (1995) Recurrent inguinal hernia after laparoscopic repair: possible cause and prevention. Br J Surg 82:539–541
Lowham AS, Filipi CJ, Fitzgibbons RJ Jr, Stoppa R, Wantz GE, Felix EL, Crafton WB (1997) Mechanisms of hernia recurrence after preperitoneal mesh repair. Traditional and laparoscopic. Ann Surg 225:422–431
Felix E, Scott S, Crafton B, Geis P, Duncan T, Sewell R, McKernan B (1998) Causes of recurrence after laparoscopic hernioplasty. A multicenter study. Surg Endosc 12:226–231
Inaki N, Waseda M, Schurr MO, Braun M, Buess GF (2007) Experimental results of mesh fixation by a manual manipulator in a laparoscopic inguinal hernia repair model. Surg Endosc 21:197–201
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc 19:724–727
Kapiris S, Mavromatis T, Andrikopoulos S, Georgiades C, Floros D, Diamantopoulos G (2009) Laparoscopic transabdominal preperitoneal hernia repair (TAPP): stapling the mesh is not mandatory. J Laparoendosc Adv Surg Tech A 19:419–422
Katkhouda N (2004) A new technique for laparoscopic hernia repair using fibrin sealant. Surg Technol Int 12:120–126
Macintyre IM (1998) Does the mesh require fixation? Semin Laparosc Surg 5:224–226
Ferzli GS, Frezza EE, Pecoraro AM Jr, Ahern KD (1999) Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg 188:461–465
Beattie GC, Kumar S, Nixon SJ (2000) Laparoscopic total extraperitoneal hernia repair: mesh fixation is unnecessary. J Laparoendosc Adv Surg Tech A 10:71–73
Khajanchee YS, Urbach DR, Swanstrom LL, Hansen PD (2001) Outcomes of laparoscopic herniorrhaphy without fixation of mesh to the abdominal wall. Surg Endosc 15:1102–1107
Moreno-Egea A, Torralba Martinez JA, Morales Cuenca G, Aguayo Albasini JL (2004) Randomized clinical trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg 139:1376–1379
Parshad R, Kumar R, Hazrah P, Bal S (2005) A randomized comparison of the early outcome of stapled and unstapled techniques of laparoscopic total extraperitoneal inguinal hernia repair. JSLS 9:403–407
Koch CA, Greenlee SM, Larson DR, Harrington JR, Farley DR (2006) Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. JSLS 10:457–460
Li JW, Zheng MH, Li HQ, Zhang H, Hu WG, Wang ML (2007) A randomized controlled clinical trial comparing stapling with non-stapling of mesh in laparoscopic total extraperitoneal inguinal hernioplasty. Chin J Gen Surg 22:440–442
Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S (2008) Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc 22:757–762
Higgins JPT, Green S (eds) (2008) Cochrane Handbook for Systematic Reviews of Interventions, version 5.0.1 [updated September 2008]. The Cochrane Collaboration. http://www.cochrane-handbook.org. Accessed 19 February 2010
Higgins JP, Altman DG (2008) Assessing risk of bias in included studies. In: Julian P, Higgins SG (eds) Cochrane handbook for systematic reviews of interventions. John Wiley and Sons, Chichester, UK, pp 187–241
Chinn S (2000) A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 19:3127–3131
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Liem MS, van Duyn EB, van der Graaf Y, van Vroonhoven TJ (2003) Recurrences after conventional anterior and laparoscopic inguinal hernia repair: a randomized comparison. Ann Surg 237:136–141
Spitz JD, Arregui ME (2000) Sutureless laparoscopic extraperitoneal inguinal herniorrhaphy using reusable instruments: two hundred three repairs without recurrence. Surg Laparosc Endosc Percutan Tech 10:24–29
Garg P, Rajagopal M, Varghese V, Ismail M (2009) Laparoscopic total extraperitoneal inguinal hernia repair with nonfixation of the mesh for 1, 692 hernias. Surg Endosc 23:1241–1245
Lau H, Patil NG (2003) Selective non-stapling of mesh during unilateral endoscopic total extraperitoneal inguinal hernioplasty: a case-control study. Arch Surg 138:1352–1355
Ismail M, Garg P (2009) Laparoscopic inguinal total extraperitoneal hernia repair under spinal anesthesia without mesh fixation in 1, 220 hernia repairs. Hernia 13:115–119
Smith AI, Royston CM, Sedman PC (1999) Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. A prospective randomized trial. Surg Endosc 13:804–806
Choy C, Shapiro K, Patel S, Graham A, Ferzli G (2004) Investigating a possible cause of mesh migration during totally extraperitoneal (TEP) repair. Surg Endosc 18:523–525
Irving SO, Deans G, Sedman P, Royston CM, Brough WA (1995) Does the mesh move after TAPP hernia repair? An X-ray study. Minim Invasive Ther (suppl 1) 4:54
Arvidsson D, Smedberg S (2000) Laparoscopic compared with open hernia surgery: complications, recurrences and current trends. Eur J Surg Suppl:40–47
Knook MT, van Rosmalen AC, Yoder BE, Kleinrensink GJ, Snijders CJ, Looman CW, van Steensel CJ (2001) Optimal mesh size for endoscopic inguinal hernia repair: a study in a porcine model. Surg Endosc 15:1471–1477
Awad SS, Fagan SP (2004) Current approaches to inguinal hernia repair. Am J Surg 188:9–16
Lomanto D, Katara AN (2006) Managing intra-operative complications during totally extraperitoneal repair of inguinal hernia. J Minim Access Surg 2:165–170
Acknowledgments
The authors are grateful to Sandi Robinson (USA) and Xubin Liu (China) for the assistance in the writing and editing of the manuscript.
Disclosures
Drs. Yuan Jun Teng, Shu Mei Pan, Ya Li Liu, Ke Hu Yang, You Cheng Zhang, Jin Hui Tian, and Jian Xu Han have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teng, Y.J., Pan, S.M., Liu, Y.L. et al. A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25, 2849–2858 (2011). https://doi.org/10.1007/s00464-011-1668-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1668-3