Abstract
Purpose
Different suture techniques and various suture materials are in use to close midline incisions after primary laparotomy. The ISSAAC study aimed to assess the safety and efficacy of the new ultra-long-term absorbable, elastic monofilament suture material MonoMax® for abdominal wall closure.
Methods
This is a single-arm, multicentre prospective study that included 150 patients undergoing a primary elective midline incision. The control group consists of 141 patients from the INSECT study who received MonoPlus® or PDS® for abdominal wall closure. The incidences of burst abdomen and wound infection until the day of discharge were defined as the primary composite endpoints. The rate of incisional hernias 1 year after surgery, the length of postoperative hospital stay and safety parameters served as secondary endpoints. The study has been registered under www.clinicaltrials.gov [NCT005725079].
Results
Eleven patients in the ISSAAC study [7.3%; 95% CI = (3.9; 13.1%)] experienced wound infection or burst abdomen until the day of discharge as compared to 16 [11.3%; 95% CI = (6.6; 17.8%)] patients in the INSECT control group (p = 0.31). The length of postoperative hospital stay was comparable in both study groups. One year after surgery, incisional hernias were observed in 21 ISSAAC patients (14.0%) in contrast to 30 hernias (21.3%) in the INSECT control group.
Conclusions
The ultra-long-term absorbable, elastic monofilament suture material MonoMax® is safe and efficient for abdominal wall closure.
Similar content being viewed by others
Introduction
Complications related to midline laparotomy are frequent and sometimes serious. The rate of incisional hernias 1 year postoperatively is estimated to be 9–20% [1–4], the frequency of reoperation due to burst abdomen 1–3% [5–8] and the rate of wound infections 3–19% [9–12]. The optimal technique and suture material for abdominal wall closure have, therefore, long been a matter of debate [13–19]. A recent meta-analysis (‘INLINE’) [20] that includes data from the recent INSECT study [1] found a significantly lower hernia rate following elective abdominal wall closure using a running suture technique rather than an interrupted suture. Furthermore, slowly absorbable suture materials produced significantly fewer hernias than rapidly absorbable sutures [20]. In contrast to previous meta-analyses [13, 15, 16], the INLINE meta-analysis found absorbable suture materials to be superior to non-absorbable sutures regarding the rate of incisional hernias in the elective situation with slowly absorbable sutures producing significantly less hernias than rapidly absorbable sutures [20].
Several synthetic absorbable suture materials with different tensile strengths and absorption rates have been developed in the past. These suture materials are absorbed by the body within 70 to 180 days, but they also lose 50% of their tensile strength during the first 14 to 30 days [21]. However, it has been shown that the abdominal fascia regains only 70% of its original strength within 1 year after a primary midline laparotomy [8]. The absorption rate of currently used suture materials might, therefore, be too fast and prolonged suture support would be needed for adequate abdominal wall closure [8]. In conclusion, an ultra-long-term monofilament absorbable suture material may help to reduce incisional hernia. First, because of its smooth, monofilament structure this suture material might reduce wound infections in comparison to rough multifilament sutures which promote bacterial adherence and migration by their capillary action [22]. Second, due to its high elasticity and flexibility it might support the mechanics of the abdominal wall and, therefore, might reduce the risk of tear of the suture from the tissue [23]. Finally, as a result of its ultra-long absorption profile and its high tensile strength, it would give the fascia more time to heal and to regain a higher strength which might reduce the development of incisional hernias compared to conventional long-term and short-term absorbable sutures [23].
MonoMax® is an ultra-long-term absorbable monofilament suture material with high elasticity and flexibility. It consists of poly-4-hydroxybutyrate and possesses an initial strength and a constant degradation rate. The suture is characterised by high knot tensile strength retention and long-lasting linear tensile strength retention, indicating that MonoMax® might be suitable for abdominal wall closure (Table 1). The ISSAAC study was, therefore, designed as a historically controlled, single-arm, multicentre, prospective study to evaluate the safety and efficacy of B. Braun Aesculap MonoMax® suture material for abdominal wall closure after primary median laparotomy.
Methods
The study protocol has been published previously to ensure the transparency of this study [24]. The final study protocol was approved by the ethics committee of the University of Heidelberg. Secondary approval was obtained from all local ethics committees responsible for the participating centres. The ISSAAC study was initiated and sponsored by Aesculap AG and conducted in cooperation with the Coordination Centre for Clinical Trials (KKS) Heidelberg. KKS was responsible for monitoring, database maintenance and biostatistics. Aesculap AG has registered the study under www.clinicaltrial.gov. During a first investigator meeting, all participating centres were trained in the required suture technique using abdominal wall model mini-pigs as mentioned in the study protocol [24].
Study design
ISSAAC was designed as a historically controlled, single-arm, multicentre prospective study to evaluate the safety of the MonoMax® suture material for abdominal wall closure following primary midline laparotomy. Patients treated with PDS® or MonoPlus® suture materials in the preceding INSECT study [1] served as historical controls. Both study cohorts were treated in the same centres, and the same documentation standards and case report forms, where applicable, were used.
Participants
The inclusion and exclusion criteria as well as the surgical procedures have been described in the study protocol [24]. The study included patients undergoing primary elective midline laparotomy with an expected length of skin incision of at least 15 cm. [Patients with prior laparoscopy or abdominal operation via a paramedian incision (e.g. appendectomy) were also included in the study.] Patients had to be at least 18 years of age; their BMI had to be inferior to 35 kg/m2 and their expected survival after surgery more than 12 months.
Exclusion criteria were peritonitis, emergency surgery, known coagulopathy, severe psychiatric or neurologic disease, participation in another intervention with a presumed interference of the intervention or outcome of this study, drug or alcohol abuse, current immunosuppressive therapy (more than 40 mg of a corticoid per day or azathioprine), chemotherapy within 2 months before the operation, radiotherapy of the abdomen completed less than 8 weeks before the operation and lack of informed consent. The study, furthermore, excluded patients not able to understand and to follow the instructions given by the investigator, pregnant or breast-feeding women and patients who had been committed to an institution.
The study was conducted at four centres in Germany: Heidelberg, Munich, Lingen and Marburg. These centres were selected as the four most successfully recruiting centres of the INSECT study. To ensure optimal comparability, in the control group, only INSECT patients from these four centres were included into analysis. Data from INSECT patients reported here may therefore differ from the original study publication that included patients from all INSECT study centres [1].
Interventions
The surgical procedure for closing the midline incision was standardised and the same as used in the INSECT study [1, 18]. Starting either from the cranial end or from the caudal end of the wound, the abdominal wall was closed by placing four Mikulicz or equivalent clamps at the edges of the abdominal fascia and a continuous all-layer suture using two MonoMax® loops (USP1/Aesculap AG, Tuttlingen, Germany). Before use, in order to avoid breakage of the material, the monofilament suture MonoMax® was stretched once by the assisting nurse/operation technician. The first stitch was anchored cranially and caudally of the incision. The distance to the edge of the fascia and the distance between two stitches did not exceed 2 cm to 2.5 cm. After having closed half of the wound, the surgeon cut one end of the loop immediately below the needle, passed it from the opposite edge of the fascia and tied both ends with at least four knots. He proceeded in the same manner with the loop from the other end of the wound which intersects the first loop at the middle of the incision, both sutures lines overlapping at least 2 cm. For every patient, two loops were used, irrespective of the length of the wound. No subcutaneous drainage was inserted. The skin was closed using clips or interrupted monofilament non-absorbable sutures.
The control group included INSECT patients from the same four centres that had participated in the ISSAAC study, whose midline incision was closed with either PDS® (180 cm loop, USP 1, HRT 48 needle; Ethicon GmbH, Norderstedt, Germany) or MonoPlus® (150 cm loop, USP 1, HRT 48 needle; Aesculap AG). The characteristics of the different suture materials are shown in Table 1.
Outcomes
The frequency of reoperation due to burst abdomen or wound infection until the day of discharge was chosen as a primary combined endpoint for safety.
The secondary endpoints, to study efficacy, were the frequency of abdominal hernias at 12 ± 1 months after surgery, the frequency of wound infections and complicated wound healing at 30 days after surgery, and the length of hospital stay.
A hernia was diagnosed if the ultrasound showed a fascial gap or a protruding sac confirmed by physical examination. The assessment and documentation were conducted by a physician who was familiar with the examination of the abdominal wall but who was not involved in the surgical procedure. The ultrasound exam had to be carried out by an investigator who had at least 6 months training in this method.
Wound infection was defined as redness, wound dehiscence with secretion (putrid or caliginous fluid) and/or microbiological evidence of bacterial contamination. A burst abdomen was diagnosed if postoperatively the continuity of the abdominal fascia was interrupted in combination with wound dehiscence and a consecutive relapse operation. A complicated wound healing was recorded if the incision did not close completely, necrosis of the wound edge or primary or secondary dehiscence occurred or if the formation of a seroma, fistula or bleeding was seen.
Study objectives
The primary hypothesis of the study was that the combined frequency of wound infection and of re-operation due to burst abdomen until day of discharge was equal or lower in the ISSAAC study group than in patients enrolled in the INSECT control group.
The incidence of incisional hernias 12 ± 1 months after surgery and the length of postoperative hospital stay were evaluated as secondary endpoints. In addition, the wound infection rate and complicated wound healing were assessed 30 days postoperatively and were compared to the INSECT control group.
Sample size
The aim of the study was to reject the null hypothesis that the rate of events such as wound infections and burst abdomen is at least 25% at the 5% level. If the true rate of composite endpoints is 15%, it was aimed to have a power of 90% for this test. With 140 patients, the power was estimated to be 90%. It had been expected that the historical control group would comprise about 130 patients who had been enrolled into the INSECT study. To make the comparison with the historical control group as meaningful as possible, the size of the MonoMax® group should not exceed the size of the control group by too much and had been accordingly established at 150 patients, including expected 10 dropouts.
Statistical methods
Patients were analysed using the intention to treat (ITT) principle. A patient belonged to the ITT population after confirmed completion of the surgical intervention by an enrolment fax form. One patient was excluded from the retrospective INSECT cohort because no postoperative data were recorded for him.
The primary endpoint was a composite event comprising wound infection and burst abdomen until day of discharge after surgical intervention. The event rate was assessed by calculating the exact 95% and 90% confidence intervals based on Clopper and Pearson method [25]. Additionally and as a secondary analysis, a confidence interval for the odds ratio of wound infections and burst abdomen was calculated using likelihood ratio methods in a logistic regression model. The event rates of wound infection and reoperation due to burst abdomen until the day of discharge was compared between the two study groups with Fisher’s exact test at the 5% level.
The frequency of wound infections and complicated wound healing 30 days after surgery, the incidence of abdominal hernias after 12 ± 1 months and length of postoperative hospital stay were used as secondary endpoints. The incidence of abdominal hernias up to 1 year were estimated by Kaplan–Meier methods and 95% and 90% confidence intervals were given based on Greenwood’s formula for the standard error and using the normal approximation of the distribution of the estimate for the hazard rate. The length of postoperative hospital stay was compared between study cohorts using a Cox regression model. These endpoints were analysed within the ISSAAC study population as well as in comparison to the historical INSECT control group.
With respect to the other endpoints, Fisher’s exact test was used for comparison between treatment cohorts.
The analysis was performed after closing the ISSAAC database by using the SAS System (SAS Inc., Cary, NC, USA) according to a previously specified statistical analysis plan [24].
Results
Recruitment
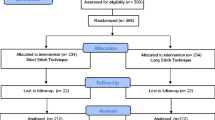
Four study centres included 150 patients between December 5, 2007 and June 30, 2008 in the ISSAAC study (Fig. 1, Table 2). One-year follow-up was completed in July 2009. The historical INSECT control group had been recruited between July 11, 2004 and September 26, 2006, and consisted of 142 patients allocated either to MonoPlus® or to PDS® suture materials for abdominal wall closure (Table 2). INSECT patients concluded their 1-year follow-up until October 2007.
Demography and baseline characteristics
Demography and baseline characteristics are shown in Table 3. There was no significant difference between the two study groups regarding gender, age, BMI, smoking status and the percentage of patients with rectus diastasis or umbilical hernias. More patients with prior abdominal incisions (other than median laparotomy) were seen in the INSECT cohort (p = 0.025). This was in line with the higher number of patients in the INSECT study with previous surgical history (data not shown).
Colorectal surgery was more often performed in the historical control group than in the ISSAAC group. More surgical interventions regarding the pancreas, stomach and the oesophagus were conducted in the ISSAAC study compared to the control group (Table 3).
The patients’ median length of abdominal wound was 24.1 ± 4.6 cm for the ISSAAC and 23.5 ± 5.3 cm for the INSECT control group (Table 3).
Surgeons’ experience
All except one surgical intervention in the ISSAAC study were performed by a board certified surgeon while in the INSECT study all but 10 surgeries were conducted by a board certified surgeon. In Munich, one surgeon accomplished more than half of the 50 interventions, while in Lingen all abdominal wall closures were executed by the same surgeon. In Heidelberg, no surgeon carried out more than eight surgical procedures.
Primary endpoint
The combined primary endpoint was reoperation due to burst abdomen and/or wound infection until day of discharge. Eleven patients in the ISSAAC study group [7.3%; 95% CI = (3.9; 13.1%)] had a wound infection and/or a burst abdomen up to day of discharge. In the INSECT control group, 16 out of 141 patients [11.3%; 95% CI = (6.6, 17.8%)] experienced a wound infection and/or a reoperation due to burst abdomen. No significant difference between treatment groups was found (p = 0.31).
Secondary endpoints
For further evaluation of secondary endpoints, both complications of the combined primary endpoint have been analysed separately.
Burst abdomen
The rate of burst abdomen until the day of discharge in the ISSAAC study group (2.0%; Table 4) was equal to the INSECT control group (2.8%; p = 1.0).
Wound infections
The wound infection rate until the day of discharge in the ISSAAC study group (6.7%; Table 4) was comparable to the INSECT control group (9.2%; p = 0.52). Twenty-three (15.3%) patients of the ISSAAC study group developed a wound infection during the first 30 days after surgery. In the control group, 18 (12.7%) wound infections were recorded until 6 months after surgery. For comparison, wound infections occurring until 1 year postoperatively were also analysed in the ISSAAC study cohort. One additional wound infection was seen during this period in the ISSAAC group. Therefore, most of the wound infections occurred within the first month and no difference was observed between the two study groups (Table 4).
The 10 patients with wound infection were by 2.5 (−0.1; 5.2) kg/m2 more overweight than the patients without wound infections, while only two wound infection patients had a BMI above 30 kg/m2. Five of the 10 wound infection patients were smokers while 42% of the patients not infected were smokers (not significant). Eight of the patients with wound infections underwent colon surgery; one patient was operated on for rectal carcinoma and one for a tumour in the lower left abdomen.
Complicated wound healing
Complicated wound healing as defined above were not documented in the INSECT study. Therefore, this parameter is only recorded for MonoMax® patients. In total, 30 complicated wound healings were reported in 147 patients until 30 days postoperatively.
Length of hospital stay
Patients of both study groups stayed in hospital for a median duration of 11 days after surgery (Table 4).
Incisional hernia rate
In the ISSAAC cohort, 21 hernias were observed in 150 patients within 1 year after surgery. Thirty hernias were present in the INSECT control group (Table 4). A Kaplan–Meier analysis rendered a 1-year hernia risk of 18.6% [95% CI (11.4%; 25.8%)] in ISSAAC patients and 25.4% [95% CI (17.6%; 33.3%)] for INSECT patients. A proportional hazard test for difference between the two study cohorts with respect to the risk of incisional hernia with centre included as fixed effects rendered a p value of 0.22, the point estimate of relative risk being at 69%. More hernias in the INSECT group were recorded as fascial gaps in comparison to the ISSAAC group [N = 28 (19.9%) vs. N = 17 (11.3%)]. The number of bulging sacs was N = 16 (10.7%) in the ISSAAC study vs. N = 15 (10.6%) for INSECT.
Among the 21 hernias, there were five obese (BMI > 30 kg/m2) patients, which was not significantly more than 16 among the non-hernia patients, but the mean BMI was higher by 2.3 (0.6; 4.1) kg/m2 in hernia patients compared to patients without hernia. As for smoking status, there was no difference seen between hernia and non-hernia patients (43% vs. 42%).
Adverse events
The reported adverse events occurred mainly in the gastrointestinal tract or due to general disorder, injury and procedural complications. Forty-six per cent of the documented adverse events were estimated as mild, 30% as moderate and 24% as severe within 1 year. In total, 51 of the adverse events were assessed as severe in 150 patients. Twenty five patients deceased within 1 year after surgery mainly due to the malignant underlying disease. Of the other serious adverse events documented, four (one impaired wound healing, two burst abdomen and one wound infection) were recorded with a presumed possibility of association with the suture material.
Discussion
Abdominal wall closure following primary midline laparotomy is still complicated by a relevant number of incisional hernias that ranges between 9% and 20% [1–4] and, therefore, remains a clinical challenge in the daily practice of surgery. A current systematic review analysing surgical techniques for abdominal wall closure (INLINE) revealed a significantly lower incisional hernia rate using a continuous (instead of an interrupted ) suture technique (p = 0.001) with a slowly absorbable (instead of a rapidly absorbable) suture material (p = 0.009) for elective, primary abdominal wall closure [20]. Furthermore, comparison of absorbable vs. non-absorbable sutures irrespectively of the suture technique showed a significantly lower incisional hernia rate for absorbable sutures compared to non-absorbable ones. These findings, that for the first time incorporated data from the INSECT study, were in contrast to some existing meta-analyses favouring non-absorbable sutures as the ideal suture material for the closure of midline incisions [15, 16].
MonoMax® is a monofilament suture material with high elasticity and long-lasting tensile strength. It, therefore, posses the criteria of a good suture material for abdominal wall closure as discussed in the INLINE meta-analysis [20]. MonoMax® may, additionally, facilitate abdominal wall closure through its high elasticity, as experimental data indicate an important role of increased suture tension for the development of incisional hernias [26].
The primary objective of this clinical study was to demonstrate the safety of MonoMax® suture material. The safety parameters “rate of burst abdomen” and “wound infections until the day of discharge” were therefore chosen as a combined primary endpoint as opposed to incisional hernia development which was the primary endpoint in the INSECT study. It was expected that the combined frequency of these parameters should be equal or lower than in the INSECT control group.
A lower number of ISSAAC patients experienced a burst abdomen and/or a wound infection compared to INSECT control patients (7.3% vs. 11.3%), but this difference was not significant. We therefore conclude that MonoMax® suture material is as safe as current sutures for abdominal wall closure.
From our experience, one should, however, avoid a too forced elongation of the elastic filament, as this—when the suture retracts to its normal length—may increase the risk of tissue ischemia on the wound edges. This recommendation is in line with experimental data on the importance of suture tension [26].
Wound infections remain the most important early postoperative complication as within the first 30 days postoperatively they develop in 3–21% of patients undergoing a midline laparotomy [4–9]. In the current study, wound infections were observed in 6.7% of ISSAAC patients compared to 9.2% in the INSECT control group until the day of discharge. An increase to 15.3% was seen in ISSAAC patients after 1 month and to 12.4% in INSECT patients after 6 months postoperatively. Seiler et al. [1] concluded that a wound infection rate of 16% (for all study centres) found in the INSECT study despite the antibiotic prophylaxis which was received by nearly all included patients (98%) was higher than expected. Our results confirm the high wound infection rate observed in the INSECT and other studies.
The development of wound infections depends on a number of factors; suture material is one of them, suture technique another, and all need to be put at stake. While the present study focused on a specific innovative suture material, a recent study from Millbourn et al. showed that the wound infection rate after primary midline incision may be decreased with a monofilament suture material by simply placing stitches less than 10 mm from the wound edge [27]. Further efforts are required to reduce this burden of complication.
The frequency of burst abdomen until the day of discharge in the current study was 2.0% for the ISSAAC study group and 2.8% for the INSECT control group. This lies within the range of 1–3% reported in the literature [5–8]. In sum, early postoperative complications following abdominal wall closure with MonoMax® did not differ significantly from data for other suture materials.
The absence of incisional hernia is the most important long-term criterion of successful abdominal wall closure. In the literature, the incidence of postoperative hernia varies between 9% and 20% depending on the suture technique and material [1–4]. The INSECT study, covering overall 625 patients in 25 participating centres, analysed if the continuous suture technique was better than the interrupted suture technique for abdominal wall closure [1] and found an overall incisional hernia rate of 11.2% for the continuous suture technique and 15.9% for the interrupted suture technique. In contrast, the observed incisional hernia rate was 14.0% in the ISSAAC study group and lower than in the historical INSECT control group (21.3%) comprising only the same four ISSAAC study centres (Heidelberg, Munich, Lingen and Marburg) and only monofilament suture materials. Therefore, the hernia rate which was seen with MonoMax® ranked around the mean of published hernia rates, whereas the hernia rate of the INSECT control group was found at the upper limit of the reported range.
Concerning the difference in hernia rates between the two cohorts (11.2% vs. 21.3%) it must, nonetheless, be conceded, that although the four centres had been picked on merit of their recruitment performance in the INSECT study and not for their high rate of hernias, some of the difference may be explained by a regression-to-the-mean effect (i.e. the phenomenon that if a variable is extreme on its first measurement, it will tend to be closer to the average on a second measurement). In addition, the study was not powered for this secondary endpoint. An analysis comparing MonoMax® to the entire INSECT population—which would increase the power of the statistical test—was not performed because centre was too important a factor not to control for in a historical control approach.
Given the significant number of patients showing a fascial gap and the corresponding risk of hernia development [28], the originally published study protocol has been amended to include a 3-year follow-up in order to investigate the long-term incisional hernia rate.
Regarding the adverse events recorded in this study, in 47 of 51 cases a causal connection with the suture material MonoMax® was excluded. These events were known complications of the patients’ underlying disease or the main surgical procedure but not abdominal wall closure. In 150 patients, four serious adverse events (2.6% of patients) were recorded with a possible association with the suture material. This rate is within the range of what can be expected in this patient population.
As this was a historically controlled study, changes have been noticed in the current study in comparison to the control group which enrolled patients 3 years before the ISSAAC study. Differences with respect to the population, the underlying diseases for which the patients were operated on, as well as to the surgical procedures performed, have been observed and are most likely caused by the centre selection. Therefore, and because the present study was not powered for this parameter, a randomised controlled trial recruiting a larger patient number is needed in order to adequately assess the frequency of incisional hernia and the importance of wound infections for their development after abdominal wall closure using MonoMax®. Given the relative similarity of current sutures and the novel characteristics of MonoMax® suture material, this trial should also assess parameters like surgeon satisfaction and handling.
In conclusion, the results provided by the ISSAAC study confirmed that MonoMax® suture material is safe as current sutures for abdominal wall closure after primary midline laparotomy. The rate of wound infections in this study was high but comparable to previous examinations, suggesting that factors other than the suture material itself might play a crucial role. A randomised controlled trial including a larger number of patients will be necessary to evaluate the efficiency of MonoMax® suture material in terms of hernia development.
References
Seiler CM, Bruckner T, Diener MK, Papyan A, Golcher H, Seidlmayer C, Franck A, Kieser M, Buchler MW, Knaebel HP (2009) Interrupted or continuous slowly absorbable sutures for closure of primary elective midline abdominal incisions: a multicenter randomized trial (INSECT: ISRCTN24023541). Ann Surg 249(4):576–582
Conze J, Klinge U, Schumpelick V (2005) Narbenhernien. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 76(9):897–909, quiz 910
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171(1):80–84
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72(1):70–71
Luijendijk RW, Lemmen MH, Hop WC, Wereldsma JC (1997) Incisional hernia recurrence following "vest-over-pants" or vertical Mayo repair of primary hernias of the midline. World J Surg 21(1):62–65, discussion 66
Paul A, Lefering R, Kohler L, Eypasch E (1997) Current practice of incisional hernia reconstruction in Germany. Zentralblatt fur Chirurgie 122(10):859–861
Manninen MJ, Lavonius M, Perhoniemi VJ (1991) Results of incisional hernia repair. A retrospective study of 172 unselected hernioplasties. Eur J Surg 157(1):29–31
Hoer J, Lawong G, Klinge U, Schumpelick V (2002) [Factors influencing the development of incisional hernia. A retrospective study of 2,983 laparotomy patients over a period of 10 years]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 73(5):474–480
Israelsson LA, Jonsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80(10):1284–1286
Irvin TT, Stoddard CJ, Greaney MG, Duthie HL (1977) Abdominal wound healing: a prospective clinical study. Br Med J 2(6083):351–352
Gys T, Hubens A (1989) A prospective comparative clinical study between monofilament absorbable and non-absorbable sutures for abdominal wall closure. Acta Chir Belg 89(5):265–270
Osther PJ, Gjode P, Mortensen BB, Mortensen PB, Bartholin J, Gottrup F (1995) Randomized comparison of polyglycolic acid and polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Br J Surg 82(8):1080–1082
van’t Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J (2002) Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg 89(11):1350–1356
Weiland DE, Bay RC, Del Sordi S (1998) Choosing the best abdominal closure by meta-analysis. Am J Surg 176(6):666–670
Hodgson NC, Malthaner RA, Ostbye T (2000) The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg 231(3):436–442
Rucinski J, Margolis M, Panagopoulos G, Wise L (2001) Closure of the abdominal midline fascia: meta-analysis delineates the optimal technique. Am Surg 67(5):421–426
Wissing J, van Vroonhoven TJ, Schattenkerk ME, Veen HF, Ponsen RJ, Jeekel J (1987) Fascia closure after midline laparotomy: results of a randomized trial. Br J Surg 74(8):738–741
Knaebel H-P, Koch M, Sauerland S, Diener MK, Büchler MW, Seiler CM (2005) Interrupted or continuous slowly absorbable sutures—design of a multi-centre randomised trial to evaluate abdominal closure techniques INSECT-Trial [ISRCTN24023541]. BMC Surg 5:3
Hsiao WC, Young KC, Wang ST, Lin PW (2000) Incisional hernia after laparotomy: prospective randomized comparison between early-absorbable and late-absorbable suture materials. World J Surg 24(6):747–751, discussion 752
Diener MK, Voss S, Jensen K, Buchler MW, Seiler CM (2010) Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg 251(5):843–856
Miles JS (1986) Use of polydioxanone absorbable monofilament sutures in orthopedic surgery. Orthopedics 9(11):1533–1536
Choi H-J, Chae H-D (2009) Comparison of E. coli infiltration between new synthetic absorbable sutures. J Korean Surg Soc 77(1):1–6
Fackeldey V, Hoer J, Klinge U (2004) [Fascial healing and wound failure]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 75(5):477–483
Fischer L, Baumann P, Husing J, Seidlmayer C, Albertsmeier M, Franck A, Luntz S, Seiler CM, Knaebel HP (2008) A historically controlled, single-arm, multi-centre, prospective trial to evaluate the safety and efficacy of MonoMax(R) suture material for abdominal wall closure after primary midline laparotomy. ISSAAC-Trial [NCT005725079]. BMC Surg 8(1):12
Clopper CJ, Pearson ES (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. vol 26. First published. doi:10.1093/biomet/26.4.404
Hoer J, Klinge U, Schachtrupp A, Tons C, Schumpelick V (2001) Influence of suture technique on laparotomy wound healing: an experimental study in the rat. Langenbecks Arch Surg 386(3):218–223
Millbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144(11):1056–1059
Pollock AV, Evans M (1989) Early prediction of late incisional hernias. Br J Surg 76(9):953–954
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Albertsmeier, M., Seiler, C.M., Fischer, L. et al. Evaluation of the safety and efficacy of MonoMax® suture material for abdominal wall closure after primary midline laparotomy—a controlled prospective multicentre trial: ISSAAC [NCT005725079]. Langenbecks Arch Surg 397, 363–371 (2012). https://doi.org/10.1007/s00423-011-0884-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0884-6