Abstract
Background
Adequate indication and duration of administration are central issues of modern antibiotic treatment in intensive care medicine. The biochemical variable procalcitonin (PCT) is known to indicate systemically relevant bacterial infections with high accuracy. In the present study, we aimed to investigate the clinical usefulness of PCT for guiding antibiotic treatment in surgical intensive care patients with severe sepsis.
Patients and methods
Patients were randomly assigned to a PCT-guided or a control group requiring antibiotic treatment. All patients received a calculated antibiotic regimen according to the presumed microbiological spectrum. In the PCT-guided group, antibiotic treatment was discontinued if clinical signs of infection improved and the PCT value was either <1 ng/ml or decreased to <35% of the initial concentration within three consecutive days. In the control group, antibiotic treatment was directed by empirical rules.
Results
The PCT-guided group (n = 14 patients) and the control group (n = 13 patients) did not differ in terms of biological variables, underlying diseases, and overall disease severity. PCT guidance led to a significant reduction of antibiotic treatment from 6.6 ± 1.1 days (mean ± SD) compared with 8.3 ± 0.7 days in control patients (p < 0.001) along with a reduction of antibiotic treatment costs of 17.8% (p < 0.01) without any adverse effects on outcome.
Conclusions
Monitoring of PCT is a helpful tool for guiding antibiotic treatment in surgical intensive care patients with severe sepsis. This may contribute to an optimized antibiotic regimen with beneficial effects on microbial resistances and costs in intensive care medicine.
Similar content being viewed by others
Introduction
Among a large array of laboratory variables, procalcitonin (PCT) has emerged as the leading one to indicate systemic infections with high accuracy. There is extensive clinical evidence that PCT allows reliable differentiation between systemic inflammatory response syndrome (SIRS) and bacterial or fungal sepsis [8, 18] and closely correlates with the systemic severity of infections in various diseases and medical disciplines [2, 9, 19, 20]. Moreover, some recent clinical studies have also shown that PCT is a reliable means to guide antibiotic therapy in community-acquired pneumonia and sepsis [4, 5, 17].
There is still a lack of evidence-based data about the optimum length of treatment with antibiotics in intensive care patients with severe sepsis after abdominal surgery. In clinical practice, antibiotic administration is usually recommended for 10 to 14 days [24]. However, it is well known that unnecessary and extended antibiotic treatment carries the risk of complications and considerably adds costs. Drug-related side effects such as allergic reactions or pseudomembrane colitis are frequently observed and the risk of life-threatening infections with multiresistant bacteria is significantly increased [3, 21, 26]. A causal relationship between antibiotic administration and drug resistances has been well established [7]. In addition, the frequency of multiresistant microorganisms in patients with long-standing antibiotic therapy is markedly increased [3]. In this context, fungal infections have emerged as another problem, even if antibiotic treatment is applied for only 7 days and patients are immunocompetent [13].
In the present study, we therefore aimed to assess the clinical value of daily serum PCT measurements for guiding the length of antibiotic treatment in surgical intensive care patients with severe sepsis.
Patients and methods
Ethics commission approval was obtained from the University of Kiel. Patients after abdominal surgery and after start of antibiotic treatment with the diagnosis of severe sepsis who were admitted to the intensive care unit of the Department of Anesthesiology and Intensive Care Medicine of the Westküstenklinikum Heide between October 2006 and April 2007 were eligible to the study. Severe sepsis was defined according to the ACCP/SSCM consensus conference of 1992 [1].
Thereafter, patients were randomly assigned to either PCT-guided antibiotic treatment or a control group receiving standard antibiotic therapy. For either group, a calculated antibiotic regimen according to the underlying infectious pathology was applied. In the two groups, daily standard routine laboratory analysis including C-reactive protein (CRP) was performed; PCT was measured in the PCT-guided group. The Sequential Organ Failure Assessment (SOFA) score was calculated on a daily basis [22] as well as the Simplified Acute Physiology Score II (SAPS) on study inclusion [12] in all patients to assess the overall systemic disease severity.
In the PCT-guided group, antibiotic therapy was discontinued if clinical signs and symptoms of sepsis improved and PCT values either had decreased to 1 ng/ml or less or had dropped to 25–35% of the initial PCT concentration over three consecutive days. In the control group, antibiotic treatment was discontinued according to clinical signs and empiric rules. Independent from the study protocol, the physician in charge was always free to decide to continue or change the antibiotic regimen upon clinical judgement.
PCT was analyzed with the BRAHMS PCT LIA® assay in serum (B.R.A.H.M.S Aktiengesellschaft, Hennigsdorf, Germany) according to the manufacturer’s instructions. CRP was measured with the Vitros Chemistry System® 5.1 FF assay (Ortho-Clinical Diagnostics GmbH, Neckargemünd, Germany) in the clinical routine laboratory. The upper normal reference range for PCT is <0.5 ng/ml and for CRP <0.7 mg/dl.
In all patients, age, gender, diagnosis, length of hospital and intensive care unit (ICU) stay, outcome, and duration of antibiotic treatment were recorded. In addition, all microorganisms isolated and antibiotic substances applied were documented.
Continuous variables are presented as mean and standard deviation; statistical analysis was performed by using the Mann–Whitney U test. Differences in percentages were analyzed by using the chi-square test. A p < 0.05 was considered statistically significant. All statistics were performed with the Statistica software package (StatSoft Europe GmbH, Hamburg, Germany).
Results
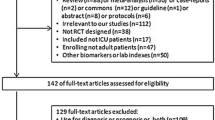
Between October 2006 and April 2007, 27 of 125 screened patients met the inclusion criteria by fulfilling the definition of severe sepsis [1] after abdominal surgery and simultaneous start of antibiotics. Patients were excluded if they did not meet the respective inclusion criteria, refused informed consent, or already had received antibiotic treatment prior to admission to the ICU. Finally, 14 patients were randomly assigned to the PCT-guided treatment group and 13 patients to the control group.
The two study groups were comparable with respect to age, gender, overall systemic disease severity according to SAPS II and SOFA scores, length of ICU treatment, and ultimate outcome (death; Table 1). Correspondingly, no difference was found with regards to underlying diseases–source of sepsis, antibiotic substances applied, and type of microorganisms isolated (Table 2). Besides eight patients with postoperative pneumonia, 19 patients suffered from secondary peritonitis. The underlying pathology for peritonitis was colonic–sigmoid perforation (28%), anastomotic leakage (21%), transmigration peritonitis (15%), small bowel perforation (11%), gastric perforation (15%), gallbladder perforation (5%), and one tubo-ovarian abscess (5%). The length of antibiotic treatment was 6.6 ± 1.1 days in the PCT-guided group, which was significantly shorter than in the control group (p < 0.001) with 8.3 ± 0.7 days (Fig. 4). No negative effects on treatment results and outcome were observed (Tables 1 and 2). The cost of antibiotic treatment was significantly reduced by 17.8% in the PCT-guided group compared to control (p < 0.01).
The course of PCT and CRP concentrations did not reveal a significant difference between the two groups (Figs. 1 and 2). Compared with the initial concentration measured upon study inclusion, PCT levels had significantly decreased after the fourth study day in the PCT-guided group (Fig. 3).
Discussion
Sepsis still represents the major cause of morbidity; severe sepsis and associated multiorgan dysfunction are the leading causes of morbidity in intensive care patients [6]. A central issue according to current sepsis guidelines is early and goal-directed treatment avoiding any delay [24]. Therefore, immediate and accurate diagnosis of infection and sepsis is of high importance for clinicians. Until a decade ago, there was an evident lack of specific biochemical markers for a reliable differentiation of bacterial from viral infections or noninfectious inflammation. Over the past years, PCT has evolved as the first marker that allows a significantly better diagnosis of bacterial infections and sepsis than any clinical sign or routine laboratory variable ever since [8, 18].
It is largely known that well-established acute-phase proteins such as CRP are of little value in diagnosing infections and sepsis because they mainly reflect the degree of the systemic inflammatory response irrespective of the presence or absence of infections [23]. In addition, the typical delay of any CRP increase with peak levels after several days precludes its use for a timely and close monitoring of an inflammatory insult [14]. In the present study, the two groups were comparable with respect to the systemic inflammatory severity. During antibiotic treatment, PCT values decreased stepwise to the reference range, whereas CRP concentrations persisted far above normal levels.
Harbarth and coworkers could show that PCT allows reliable differentiation between patients with SIRS and sepsis and correlates, as observed for interleukin 6, with the systemic severity of the inflammatory response [8]. In the same study, the authors nicely demonstrated that PCT decreased to normal levels in patients with sepsis and successful treatment, whereas patients with SIRS and no infectious focus usually presented with PCT values below 1 ng/ml.
Very recent studies suggest that a PCT-guided algorithm reduces the frequency and length of antibiotic treatment without adverse effects on therapeutic success and outcome [5, 17]. We were able to confirm these observations in the subset of surgical intensive care patients. Antibiotic treatment was significantly shortened (Fig. 4) along with a reduction of costs of 17.8%. Accordingly, no differences as far as success of treatment and outcome were noted.
There is still a lack of evidence-based data as far as the optimum duration of antibiotic treatment in septic patients is concerned. Current guidelines recommend therapeutic intervals of 10 to 14 days [24]. Chastre and coworkers compared an 8-day with a 15-day therapeutic interval in septic patients with ventilator-associated pneumonia and did not observe any outcome difference between both groups. However, the overall incidence of pneumonia recurrences was higher in the 8-day treatment group, whereas the 15-day treatment group revealed a markedly higher incidence of multiresistant bacteria if reinfections occurred [3]. In a subsequent trial of Micek and coworkers [16], the appropriate length of antibiotic treatment in ventilator-associated pneumonia was found to be an interval of 7 to 8 days in case of therapeutic response. Christ-Crain and coworkers [5], in a cluster-randomized study in 300 patients with community-acquired pneumonia, were able to reduce antibiotic treatment from 12 to 5 days with a PCT-guided therapeutic algorithm. Corresponding results have been published by Nobre and coworkers in patients with sepsis. In this study, antibiotics were discontinued after a median of 6 days using PCT guidance compared to 10 days in the control group without affecting clinical outcome [17].
A specific problem of intensive care medicine is the fact that early differentiation between SIRS and sepsis is of central importance for further therapeutic decision making. This usually demands continuous observation of the clinical course and assessment of various laboratory markers of inflammation and infection. However, any delay of mandatory treatment, e.g., start of antibiotics, should be avoided in this setting. A US study in patients with ventilator-associated pneumonia could impressively show that a 24-h delay of adequate antibiotic treatment after established diagnosis led to a sevenfold increase of mortality in contrast to early-onset treatment [10]. Accordingly, Kumar and coworkers [11] found a 7% increase of hospital mortality per each hour delayed antibiotic treatment in patients with septic shock.
The dramatic rise of drug resistances has driven clinicians to a strict monitoring of indications and application of antibiotic agents since epidemiological data have clearly outlined the close relationship between multiresistant bacteria and a large-scale use of specific antibiotics [7, 15, 25]. Recent data from the literature indicate that antibiotic treatment for more than 7 days increases the risk of fungal infections [13]; after more than 10 days of treatment, the incidence of drug-resistant organisms is significantly rising [24]. One of the main reasons for these developments is the poorly controlled use of antibiotics with escalating therapeutic intervals in intensive care units. The development of resistances strongly depends on the antibiotic substance and the microorganism and requires between 1 day and three decades to become manifest. If resistances have once developed, they are hardly subject to change or reversible [7]. Therefore, early therapeutic decision making against or in favor of antibiotic treatment as well as continuous monitoring of antimicrobial therapy is thought to exert beneficial effects in this context. In intensive care patients with pneumonia, Singh and coworkers were able to prove that termination of antibiotics after a 3-day treatment interval in the absence of a suspected infection did not adversely affect outcome. Concomitantly, the development of drug resistances could be reduced [21]. In this setting, PCT-guided algorithms are a helpful approach to reduce the length of antibiotic treatment without negative influence on outcome, which we and other authors [5, 17] could clearly demonstrate.
In summary, monitoring of PCT is a valuable tool for therapeutic decision making concerning the length of antibiotic treatment. However, adequate interpretation of PCT concentrations always requires the background of clinical course and symptoms. This concept contributes to less extensive antibiotic treatment with positive effects on economical factors and the development of drug resistances in intensive care medicine.
References
ACCP/SCCM Consensus Conference Committee (1992) Definition for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Brunkhorst FM, Al-Nawas B, Krummenauer F, Forycki ZF, Shah PM (2002) Procalcitonin, C-reactive protein and APACHE II score for risk evaluation in patients with severe pneumonia. Clin Microbiol Infect 8:93–100
Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, Clementi E, Gonzalez J, Jusserand D, Asfar P, Perrin D, Fieux F, Aubas S, PneumA Trial Group (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA 290:2588–2598
Christ-Crain M, Müller B (2005) Procalcitonin in bacterial infections—hype, hope, more or less? Swiss Medical Weekly 135:451–460
Christ-Crain M, Stolz D, Bingisser R, Müller C, Miedinger D, Huber PR, Zimmerli W, Harbarth S, Tamm M, Müller B (2006) Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia. Am J Respir Crit Care Med 174:84–93
Engel C, Brunkhorst FM, Bone HG, Brunkhorst R, Gerlach H, Grond S, Gruendling M, Huhle G, Jaschinski U, John S, Mayer K, Oppert M, Olthoff D, Quintel M, Ragaller M, Rossaint R, Stuber F, Weiler N, Welte T, Bogatsch H, Hartog C, Loeffler M, Reinhart K (2007) Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med 33:606–618
Harbarth S (2007) Antibiotikatherapie—Einfluss des Antibiotikaverbrauchs auf Resistenzbildung und–selektion. Anästhesiol Intensivmed Schmerzther 2:130–135
Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, Vadas L, Pugin J, Geneva Sepsis Network (2001) Diagnostic value of procalcitonin, interleukin 6 and interleukin 8 in critically ill patients admitted with suspected sepsis. Am J Respirat Crit Care Med 164:396–402
Hedlund J, Hansson LO (2000) Procalcitonin and C-reactive protein levels in community-acquired pneumonia: correlation with etiology and prognosis. Infection 28:68–73
Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH (2002) Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest 122:262–268
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Cheang M (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34:1589–1596
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Marchetti O, Bille J, Fluckiger U, Eggimann P, Ruef C, Garbino J, Caladra T, Glauser MP, Tauber MG, Pittet D (2004) Fungal infection network of Switzerland. Epidemiology of candidemia in Swiss tertiary care hospitals: secular trends, 1991–2000. Clin Infect Dis 38:311–320
Meisner M, Tschaikowsky K, Palmaers T, Schmidt J (1999) Comparison of procalcitonin (PCT) and C-reactive protein (CRP) plasma concentrations at different SOFA scores during the course of sepsis and MODS. Critical Care 3:45–50
Meyer E, Jonas D, Schwab F, Gastmeier P, Rüden H, Daschner FD (2004) SARI: surveillance of antibiotic use and bacterial resistance in German intensive care units. Correlation between antibiotic use and the emergence of resistance. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 47:345–351
Micek S, Heuring TJ, Hollands JM, Shah RA, Kollef MH (2006) Optimizing antibiotic treatment for ventilator-associated pneumonia. Pharmacotherapy 26:204–213
Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J (2008) Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 177:498–505
Oberhoffer M, Vogelsang H, Russwurm S, Hartung T, Reinhart K (1999) Outcome prediction by traditional and new markers of inflammation in patients with sepsis. Clin Chem Lab Med 37:363–368
Rau BM, Frigerio I, Büchler MW, Wegscheider K, Bassi C, Puolakkainen PA, Beger HG, Schilling MK (2007) Evaluation of procalcitonin for predicting septic multiorgan failure and overall prognosis in secondary peritonitis: a prospective, international multicenter study. Arch Surg 142:134–142
Rau B, Krüger CM, Schilling MK (2004) Procalcitonin: improved biochemical severity stratification and postoperative monitoring in severe abdominal inflammation and sepsis. Langenbecks Arch Surg 389:134–144
Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL (2000) Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med 162:505–511
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Wahl HG, Herzum I, Renze H (2003) Sepsis und Sepsismarker—update. J Lab Med 27:431–439
Welte T (2004) Antibiotikatherapie bei Sepsis. Dtsch Med Wochenschr 129:2609–2613
Welte T (2006) Die nosokomiale Pneumonie. Intensivmed 43:301–309
Yu V, Singh N (2004) Excessive antimicrobial usage cause measurable harm to patients with suspected ventilator-associated pneumonia. Intensive Care Med 30:735–738
Conflict of interest statement
The corresponding author declares speaking engagements for BRAHMS AG. All other authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
S. Schroeder and M. Hochreiter equally contributed to the paper.
Rights and permissions
About this article
Cite this article
Schroeder, S., Hochreiter, M., Koehler, T. et al. Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomized study. Langenbecks Arch Surg 394, 221–226 (2009). https://doi.org/10.1007/s00423-008-0432-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0432-1