Abstract
Objective
To investigate the factor structure of the Rivermead Post Concussion Symptoms Questionnaire (RPQ) among individuals seen as part of routine follow-up following traumatic brain injury.
Methods
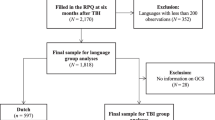
RPQ data from 168 participants was examined (mean age 35.2, SD 14.3; 89% with post traumatic amnesia duration < 24 hours) six months after admission to an Accident & Emergency Department following TBI. Structural equation modelling was carried out to evaluate proposed models of the underlying structure of post-concussion symptoms (PCS).
Results
The results support the existence of separate cognitive, emotional and somatic factors, although there was a high degree of covariation between the three factors. A two-factor model that collapsed the emotional and somatic factors together showed a similar goodness-of-fit to the data, whilst a one-factor model proved a poor fit.
Conclusion
The results support the notion of post-concussion symptoms as a collection of associated but at least partially separable cognitive, emotional and somatic symptoms, although questions persist regarding symptom specificity. The use of the RPQ is discussed, and classification bands for use in clinical practice are suggested.
Similar content being viewed by others
Introduction
Post-concussion symptoms (PCS) are a constellation of cognitive, emotional and physical complaints [57] typically characterised as occurring after mild traumatic brain injury (MTBI), defined according to criteria such as Glasgow Coma Scale (GCS) [67], posttraumatic amnesia [66] or combinations of these [3]. However, similar symptoms can be reported by individuals with more severe brain injuries [49, 61], by those who have sustained physical injuries without Traumatic Brain Injury (TBI) [7, 25, 50, 53] and by members of the general population [14, 73]. Symptom reports may also be influenced by a range of factors such as symptom expectations [13, 21, 29, 57], medicolegal status [8, 46, 53], pain [34, 59, 68], depression [29, 35, 63, 70] and stress [27, 33, 36].
Whilst these symptoms will usually improve spontaneously over the first three to six months after MTBI [2, 38, 43], they may persist for some [2, 12, 50, 56, 67]. As PCS may be associated with significant psychosocial problems and poorer quality of life [17, 19, 23, 64, 76], considerable debate has focussed on the question of persisting symptoms: a range of factors directly, indirectly and independently related to the brain injury have been suggested as causal and maintaining factors where symptoms persist [40, 48, 74].
A number of questionnaires have been developed to measure PCS, including checklists reporting the presence or absence of symptoms [45, 60], absolute or relative changes in symptoms following trauma in terms of severity, frequency or duration [27, 41] and the extent to which symptoms are problems [29] or impact on everyday life [16, 20]. Such questionnaires, usually relying on self-report, provide scope for tracking change over time of PCS, either as part of natural recovery or in response to treatment. In addition they provide an opportunity to explore those mechanisms involved in PCS by allowing comparison with other clinical groups or identifying base-rates in the general population.
Various factor structures have been proposed and examined for many of these instruments, using factor and cluster analyses in both TBI and non-TBI populations [5, 15, 62]. These studies and their results, summarised in Table 1, generally point to the existence of cognitive, affective and somatic factors of PCS, mirroring the range of symptoms in the diagnostic criteria for postconcusional disorder in ICD-10 (F.07.2) [75] and the research criteria in DSM-IV [4]. Such factors have been used more broadly to examine and contrast symptoms reported by individuals following (typically mild) TBI with other clinical groups such as individuals with chronic pain and those with orthopaedic but not brain injuries. These approaches have led to some interesting findings: for example, cognitive rather than somatic or emotional symptoms were reported as more severe by individuals who were experiencing persistent difficulties at work 6 months after MTBI when compared with individuals who reported full recovery [25].
The Rivermead PCS Questionnaire (RPQ) is another self-report measure of PCS, originally developed as a measure of severity of symptoms following MTBI [4]. It consists of 16 post-concussion symptoms including headaches, dizziness, nausea/vomiting, noise sensitivity, sleep disturbance, fatigue, irritability, feeling depressed/tearful, feeling frustrated/impatient, forgetfulness, poor concentration, taking longer to think, blurred vision, light sensitivity, double vision and restlessnesss. For each symptom, individuals are asked to rate the degree (on a scale of 0 to 4) to which it has been absent or a mild, moderate or severe problem over the previous 24 hours compared with premorbid levels. Ratings of “no more of a problem” compared with pre-injury levels are also available (corresponding to item values of 1), but are not typically added when calculating the overall total score.
Whilst the RPQ is a popular measure commonly used to evaluate PCS, with citations in over 40 papers, there has been a lack of experimental work evaluating the underlying structure of the instrument. Whilst no explicit factor structure was proposed or examined in the original study, a three-factor structure for the RPQ has been suggested by Smith-Seemiller and colleagues [68], comprising cognitive (forgetfulness, poor concentration, taking longer to think), somatic (headaches, double or blurred vision, sensitivity to noise, dizziness, nausea, sleep disturbance, fatigue) and emotional (irritability, depression, frustration, restlessness) symptoms (see Table 1). Using these proposed factors, they compared the scores of 32 individuals with MTBI with 63 individuals with chronic pain. Individuals with MTBI were recruited from referrals for assessment or treatment in private practice or the outpatient department of a teaching hospital, and were seen on average at 12 months post-injury. In terms of injury severity, all had posttraumatic amnesias of less than 24 hours, GCS’s of 13–15 (where this information was available) and no neuroimaging abnormalities. Individuals with chronic pain were being seen for treatment either in private practice or in a multidisciplinary programme at a rehabilitation hospital, and had a mean chronicity of 39 months: individuals with histories of loss or alteration of consciousness were excluded from this group. Whilst both groups reported similar overall totals and somatic symptoms on the RPQ, individuals with MTBI reported higher levels of cognitive symptoms, with a trend emerging for individuals with chronic pain to report slightly more severe emotional symptoms.
These findings also reflect results of other studies suggesting that individuals with persisting PCS may tend to report higher levels of subjective cognitive difficulties when compared with other clinical samples, at least when comparing between groups [25, 26]. Possible clusters of symptoms might assist in differentiating PCS from other clinical conditions with overlapping symptoms or help in identifying the factors that may play a role when PCS persists. However, the proposed factor structure for the RPQ remains to be experimentally investigated or validated.
Conversely, it might be argued that PCS represents a unitary construct, particularly when considering some of the mechanisms that have been proposed as contributing towards persistent symptoms. For example, symptom expectations or the tendency to attribute difficulties after a negative event to the negative event have been cited as playing a role [29, 57]: if these mechanisms applied at a global level on symptom reporting, a single factor might be expected to emerge on questionnaire measures. A single factor model might also be consistent with the possibility that elevated symptoms are described by individuals due to a more general tendency to report or complain of symptoms.
The purpose of this study was therefore to examine the factor structure of the RPQ, using a group of individuals seen as part of routine follow-up around six months after a (typically mild) TBI; this complements previous studies that have looked at PCS instruments in a non-TBI, non-clinical group [62], a non-TBI clinical group [5] and a MTBI group with persisting difficulties referred for clinical assessment [15]. There were two specific aims. Firstly using confirmatory factor analysis, we examined a possible single-factor model that would reflect PCS as a unitary syndrome. Secondly, we set out to examine the three-factor structure of cognitive, somatic and emotional symptoms proposed by Smith-Seemiller et al. [68] and implicit to an extent in the diagnostic criteria for PCS [4, 75].
Methods
The data used in this study were collected as part of the Oxford Head Injury Service (OXHIS) [71, 72], which ran from 1993 to 1996.
The study aimed to include all individuals 16–65 years of age resident in Oxfordshire (total population 560 000) admitted to hospital (the accident and emergency or the admitting wards under the Trauma Service at the John Radcliffe Hospital in Oxford and the Horton Hospital in Banbury) with a head injury of any severity and regardless of additional injuries. The definition of head injury used was “any blow to the head causing a clinical diagnosis of head injury to be made, even if insufficient to cause a definite loss of consciousness”. Patients were registered with the service by a member of the OXHIS who visited the wards two or three times a week. A total of 1186 individuals were initially registered with the service.
At 6 months after injury all eligible (e.g. still resident in Oxfordshire, had not refused further contact) patients (n = 1099) were contacted, initially by letter and then by telephone, to ask whether they were willing to be followed up. The assessors at follow-up were independent of the initial service provision. Patients were seen in person at home or as outpatients wherever possible, but by telephone if necessary. At this point, the RPQ was completed by the patients. Demographic details were also noted. Trauma details were recorded including length of posttraumatic amnesia (PTA). This was measured retrospectively by the interviewing clinicians using established criteria [66] and the Rivermead Post Traumatic Amnesia Protocol [42].
The procedure has been outlined more fully in the work of Wade and colleagues [71, 72].
Results
Participants
A full dataset of RPQ, demographic and injury details was available for 168 participants. The mean age of the patients was 35.2 years (standard deviation [SD] = 14.3) and 58% were male. Participants’ demographic and premorbid details are shown in Table 2 below. Participants in the current sample were comparable to those reported in the published studies [71, 72] in terms of gender (chi-square), age (t-test) and PTA duration (chi-square).
The majority of the participants lived with their partner (44.8%), or with their parents (25.1%). Prior to the head injury, over half the sample was employed full-time (54.6%) and the large majority (almost 80%) was involved in some form of productive activity (full-time/part-time/housework/student). There was some variation in the injury aetiology, with the commonest causes of injury stemming from road traffic accidents (20%) or “other” causes (22.4%). Most individuals seen had sustained a mild injury: 150 (89%) reported PTA durations of less than one day, consistent with the American Congress of Rehabilitation Medicine’s criteria for MTBI [3], which stipulate a PTA of less than 24 hours. Only 39 (23%) required an overnight stay in hospital.
To provide some comparison with other TBI populations, distributions of types of accident by gender were investigated, with significant variations being noted overall (Pearson χ2 (5) = 24.8, p = 0.00). Men were over-represented amongst individuals sustaining their injuries either due to assault (Pearson χ2 (1) = 6.13, p = 0.013) or at work (Pearson χ2 (1) = 5.62, p = 0.018), whilst relatively more women sustained theirs in domestic settings (Pearson χ2 (1) = 8.40, p = 0.004) or whilst horse riding (p = 0.017, two-tailed Fisher’s Exact Test). However, no significantly uneven distributions for gender were noted for injuries occurring in traffic accidents or due to other causes (Pearson χ2’s (1) < 1.5, p > 0.2).
Descriptive statistics
The weighted medians (due to positive skew) and range of each item on the RPQ are shown in Table 3. The most reported RPQ symptom at 6 months post injury was forgetfulness (weighted median = 0.75); followed by fatigue (0.64); then irritability (0.47), impatience and frustration (0.47), taking longer to think (0.47), and feeling depressed (0.47).
Whilst 42% (n = 70) of individuals report no PCS at all, some individuals are reporting symptoms to a significant degree at 6 months post-injury, with the range for all items (except double vision) extending to the maximal score. Mean RPQ totals were 9.6 (SD = 11.6, median = 4, range 0–51) when including item values of one, and 8.4 (SD = 11.9, median = 2, range 0–51) using the routine scoring method of ignoring item values of one: both distributions showed high levels of positive skew. The cumulative percentage of total scores on the RPQ among the participants is shown in Figure 1.
Correlational analysis
In order to examine the intercorrelations between the variables, nonparametric Spearman’s rank correlations were performed and these are presented in Table 4. A high degree of association between the 16 items of the RPQ was noted, with the exception of the item assessing double vision. This item also showed the greatest problems with floor effects (the weighted median and the range were the smallest for this item, at 0.02 and 0–2 respectively). Due to the extreme skew and kurtosis evident in the variable corresponding to double vision, this item was removed from all further analysis.
Structural equation modeling
Structural equation modeling (SEM) using AMOS 5.0 software was carried out in order to explore the underlying structure of the RPQ. SEM is theory- rather than data-driven, and tests models constructed on the basis of existing literature and previous empirical findings. Theorized pathways are stipulated and latent (unobserved) variables can be created from measured (observed) variables.
Normality and the bootstrap
A central assumption in structural equation modeling is that the data are normally distributed. Significant problems with univariate skew and kurtosis (skew and kurtosis z values) and multivariate skew and kurtosis (Mardia coefficient = 202.23, CR = 58.03) were identified. To correct for this, the Bollen-Stine procedure of bootstrapping was employed. Rather than calculating a single χ2 value, this procedure involves taking multiple samples (2000 in the current analysis, using sampling with replacement) from the study population. The χ2 value is calculated for each of these bootstrapped samples, and then the mean χ2 value is estimated across all of these.
Fit indices
A Bollen-Stine probability value is also calculated on the basis of the adjusted χ2 value; if this value is not significant (i.e. ≥ 0.05), it indicates that the model fits the data well.
Comparison of bootstrap and maximum likelihood estimation methods
The standard error of the bootstrapped standard error estimates (which should be very small), and the bias (i.e. the difference between the maximum likelihood estimates and the bootstrap estimates) for each parameter were examined.
Significance of parameters
Finally the regression weights and the bias-corrected confidence intervals of the bootstrap maximum likelihood estimation were compared with the original maximum likelihood estimates. If zero does not lie in the confidence interval, this indicates that the estimate is significantly different from zero and justifies retaining the parameter in the model. In addition, a visual inspection was conducted in order to identify any anomalous results e.g. Heywood cases (i.e. standardized coefficients greater than 1 or negative variances).
Models have been shown diagrammatically, values in brackets after observed variable headings refer to standardized variances and values next to pathways indicate the standardized regression coefficients.
One-Factor Solution
To evaluate whether the post-concussion symptoms measured by the RPQ reflect a single-factor syndrome, a unitary model was tested. The mean χ2 (90) = 175.13 and Bollen-Stine p = 0.000, suggesting the model should be rejected (see Table 5).
Three-Factor Solution
The logically derived factor structure of the RPQ proposed by Smith-Seemiller et al. [67] outlines three factors that underlie the symptoms: somatic, emotional and cognitive. It was decided that the three factors were likely to be related constructs and therefore were allowed to covary. The mean χ2 (87) = 168.32 and Bollen-Stine p = 0.493, indicating that the model is a satisfactory fit to the data. The standard errors of the bootstrapped standard error estimates were assessed and all were found to be very small (≤ 0.02). The bias was reasonably small for all parameters, suggesting that there were no sizeable differences with the outcome from the Maximum Likelihood Estimation (MLE), the usual method employed, when conducted without the bootstrap. For all of the parameters, zero did not lie in the confidence intervals when either the bias-corrected percentile or the percentile methods were assessed, and no Heywood cases were identified, suggesting that all pathways stipulated should be retained.
Figure 2 shows the model and the corresponding standardized weights. All of the observed variables load moderately or strongly onto the latent variables indicating that the latent variables are well defined.
Structural equation model of the RPQ reflecting the factor structure suggested by Smith-Seemiller et al. [59]
This model appears to be a reasonable fit to the data.
Two-Factor Solution
While the three-factor solution appears to fit the data acceptably, there is a very high covariance between the somatic and emotional latent variables (1.02). It is therefore possible that these two are not distinct variables, but would be more suitably conceptualised as a single Emotional-Somatic factor. The resulting model is shown in Figure 3. As shown in Table 5, the mean χ2 value and the associated Bollen-Stine p value indicate that the two-factor solution also fits the data reasonably. Standard errors of the bootstrapped standard error estimates were all ≤ 0.02, and the bias values were low, suggesting that there are similar parameters calculated using the bootstrap and the MLE method. Zero did not lie in the confidence intervals for any of the standardized parameters, indicating that all were significantly different from zero.
This model appears to be a reasonable fit to the data.
Comparison of Three-Factor and Two-Factor Solutions
This comparison cannot be conducted using a nested models approach, as the two models are structurally different. The fit of the data is very similar in terms of the Bollen-Stine p values. The three-factor solution shows a marginal improvement over the two-factor model, although this does not represent significant gains.
It is therefore not possible, using statistical means, to differentiate between the two models.
Discussion
Confirmatory factor analyses were performed on data from the RPQ of individuals with (predominantly mild) traumatic brain injuries at around six months post-injury. There was poor evidence of a single factor solution for the data, and good support for the cognitive, emotional and somatic factors proposed by Smith-Seemiller et al. [68]. However, a high degree of covariation was noted between these factors: an additional two-factor model that collapsed the emotional and somatic factors together showed a similar goodness-of-fit to the data. These models excluded the item concerning double vision.
These results support the notion implicit in the various diagnostic criteria [4, 75] of a collection of associated but at least partially separable cognitive, somatic and emotional symptoms associated with PCS. The poor single factor model suggests that reports of post-concussion symptoms cannot be viewed in simple terms as a tendency to report symptoms in general. As such, aetiological accounts of the development and maintenance of PCS may need to incorporate mechanisms explaining why some symptoms seem to cluster together in this way, albeit with similar factors to non-TBI samples [5, 62].
For example, “expectation as aetiology” or nocebo effects [29, 57] may potentially have difficulty in accounting for multiple factors if they function at a more global or general level. Further specification might be necessary: expectations of symptoms may be more specific, or be differentially affected by different precipitating events. Indeed in one study [30] undergraduate students predicted that they would experience more total symptoms if they had had a head injury, posttraumatic stress or depression compared with an orthopaedic injury, but fewer emotional symptoms after head injury compared with depression and posttraumatic stress vignettes. Whilst expectations of cognitive symptoms were not relatively elevated by a prospective head injury compared with the depression and posttraumatic stress vignettes, expectations regarding increased need to use compensatory memory strategies were elevated for the head injury vignette in that study. More generally, reactions to symptoms themselves (in terms of attributions and coping strategies) are cited as playing an important role in their persistence or resolution over time [e.g. 40, 74], although experimental evidence examining their associations with or predictions of symptoms and disability after (M)TBI continues to be relatively limited.
In contrast, models from health psychology have suggested a role for “illness coherence” as a construct that may reflect individuals’ understanding of symptoms and their response to health-related threats [32, 58]. This may contribute to certain symptom reports tending to cluster together. Cognitive symptoms in particular may be more coherent with ideas about the consequences of head injuries and therefore be reported relatively more often by individuals with PCS [25, 26, 68], at least when compared between different clinical groups.
The results also reinforce the approach in some studies [25, 68] of considering group differences in the relative emphasis of different clusters of symptoms, potentially assisting with identifying similarities and differences between clinical populations (at least at a group level), although some have argued [18] that further differentiation may be appropriate at the level of individual symptoms such as headache. The current results suggest that subjective cognitive symptoms may show some degree of separability from emotional and somatic ones, whilst still being related to them. The significance of this with respect to performance on neuropsychological tests or more general (e.g. occupational) functioning remains to be fully investigated, although links between subjective cognitive symptoms and vocational disability have been noted [25]. However, whilst persistent subjective symptoms have been associated with cognitive impairments in tests of attention at six months after MTBI [12], persisting impairments may be relatively isolated and small when studies are appropriately controlled [10]. Indeed, meta-analyses of the cognitive sequelae of MTBI typically fail to indicate significant neuropsychological impairments beyond 3 months post-injury [9, 24]. More generally, the association between subjective cognitive difficulties and objective neuropsychological impairments is typically weak in both clinical and non-clinical samples [14, 44]: the interpretation of neuropsychological assessments themselves, especially after MTBI, is often open to a range of potentially confounding variables [77].
Questions also persist as how best to characterise scores on the RPQ: due to the issues regarding the specificity of PCS, use and whether interpretation of the RPQ should be tempered by the extent to which it overlaps with broader symptomatologies of pain, fatigue and psychiatric disorders such as depression. “PCS” as measured by the RPQ might therefore be viewed as an overarching umbrella term that describes a range of different symptoms that arise for different reasons subsequent to (although not necessarily directly because of) a traumatic brain injury, notwithstanding the possible roles of expectations and attribution bias [29, 57]. Caution should always be exercised in attributing persistent symptoms directly to milder injuries, bearing in mind the various indirect mechanisms proposed in the development and maintenance of post-concussion symptoms [36, 37, 48, 57, 74].
With these points in mind, the cumulative frequencies of RPQ scores in the present sample (shown in Figure 1) might provide some means of classification. Taking the 75%, 90% and 95% limits as relatively arbitrary cut-offs, bands corresponding to minimal (less than 75%), mild (75–90%), moderate (90–95%) and severe (above 95%) levels of self-reported symptoms would be 0–12, 13–24, 25–32, and 33 or more respectively. For comparison, the mean RPQ total for a non-clinical sample of adults in the general population [14] was 5.8 (when recalculated using the recommended original scoring method), whilst the mean total for the clinical MTBI sample in the Smith-Seemiller et al. [68] study was 36.3. However, these bands are provisional and await further research to examine their sensitivity and specificity against general and clinical populations, as well as their correspondence to quality of life and general functioning.
A number of methodological criticisms of the current study may be noted. Firstly, as the current sample constituted a relatively small proportion (15%) of individuals contacted as part of routine follow-up after TBI, this might raise questions regarding the representativeness of the sample. However, the individuals in the current study did not significantly differ from follow-up studies from which the sample was drawn (in terms of variables such as gender, cause of injury and duration of posttraumatic amnesia). The male:female ratio of 58:42 % in the current study is also broadly comparable to the 57:43 ratio in an analysis of a recent national survey of Emergency Department attendees in the USA after MTBI [6], although that study also included young children and older adults.
Issues around generalisability also include the extent to which individuals seen as part of routine follow-up six months post-injury may not be representative of those populations of particular interest to clinicians, such as individuals with PCS who may be referred to secondary or tertiary services for assessment and treatment. Recruitment bias has been demonstrated [52] in follow-up studies, where individuals with more significant injuries (in terms of initial loss of consciousness, GCS, PTA, other non-TBI injuries etc.) are more likely to enrol in follow-up. One consequence is that the suggested classification bands may be on the conservative side. Litigation may reflect a further source of bias: we would advise against use of the provisional classification bands when using the RPQ in a medicolegal context.
In addition, different groups may conceivably show different factor structures on questionnaires. The possibility exists that the factor structure of an instrument may be influenced by a combination of factors including the clinical group (e.g. TBI versus non-TBI), the severity of TBI and length of time since injury. The latter may be particularly important given the possibility that different symptoms may improve at different rates [11]. However, the similarities between the cognitive, emotional and somatic factors across different populations with different measures [15] and even in non-TBI populations [5, 62] is notable, particularly given the differences between the measures and statistical methods used in these various studies. These similarities suggest a relatively robust factor structure (albeit with some variation on some items between different studies), potentially reducing the impact of possible sampling bias on the modelling of factors in the current study.
There are also possible cross-cultural issues relating to generalisability. Whilst similarities in PCS across different countries have been cited [36], we are unaware of explicit experimental comparisons in the literature. Anecdotally there may be some significant differences at least in prevalence between countries, with lower rates of persistent symptoms reported in Greece [21] and Lithuania [22] compared with other countries in Western Europe and North America: the existing factor analyses reviewed have so far been confined to populations in the USA and UK. However, comparative experimental studies of PCS across national boundaries have tended to focus on expectations of symptoms rather than those actually reported after TBI. Appropriately matched longitudinal cross-cultural studies are needed to compare the structure of post-concussion complaints and their resolution (or persistence) over time.
In summary, the results of a confirmatory factor analysis of the RPQ for a number of individuals seen six months after predominantly mild TBI’s support Smith-Seemiller et al.’s [68] suggestion of cognitive, emotional and somatic groups of post-concussion symptoms. However, a high degree of covariation was noted between the different symptom groups, particularly emotional and somatic symptoms. These results reflect similar findings for other PCS instruments in different TBI and non-TBI populations.
References
Alexander MP (1995) Mild traumatic brain injury: Pathophysiology natural history and clinical management. Neurology 45:1253–1260
Alves W, Macciocchi SN, Barth JT (1993) Postconcussive symptoms after uncomplicated mild head injury. J Head Trauma Rehab 8:48–59
American Congress of Rehabilitation Medicine (1993) Definition of mild traumatic brain injury. J Head Trauma Rehab 8:86–87
American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV). APA, Washington D.C
Axelrod BN, Fox DD, Lees-Haley PR, Earnest K, Dolezal-Wood S (1998) Application of the Postconcussive Syndrome Questionnaire with medical and psychiatric outpatients. Arch Clin Neuropsych 13:543–548
Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J (2005). Mild traumatic brain injury in the United States, 1998–2000. Brain Inj 19:85–91
Bazarian JJ, Wong T, Harris M, Leahy N, Mookerjee S, Dumbovy M (1999) Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Inj 13:173–189
Binder LM, Rohling ML (1996) Money matters: metaanalytic review of the effects of financial incentives on recovery after closed head injury. Am J Psychiat 153:7–10
Binder L, Rohling M, Larrabee G (1997) A review of mild head trauma. Part I: Meta-analytic review of neuropsychological studies. J Clin Exp Neuropsychol 19:421–431
Bohnen N, Jolles J, Twijnstra A, Mellink R, et al. (1995) Late neurobehavioural symptoms after mild head injury. Brain Inj 9:27–33
Bohnen N, Twijnstra A, Jolles J (1992) Post-traumatic and emotional symptoms in different subgroups of patients with mild head injury. Brain Inj 6:481–487
Bohnen N, Twijnstra A, Jolles J (1993) Persistence of postconcussional symptoms in uncomplicated mildly headinjured patients: A prospective cohort study Neuropsychiatry Neuropsych Behav Neural 6: 193-200
Bouchard M-E, Fortier M, Beland C, Belanger N, Cantin J-F, Pepin M (2003) Persistent concussion symptoms after mild head injury: Expectations as etiology. Brain Cognition 53:111
Chan RCK (2001) Base rate of post-concussion symptoms among normal people and its neuropsychological correlates. Clin Rehabil 15: 266–273
Cicerone KD, Kalmar K (1995) Persistent postconcussion syndrome: The structure of subjective complaints after mild traumatic brain injury. J Head Trauma Rehab 10:1–17
Crawford S, Wenden FJ, Wade DT (1996) The Rivermead head injury follow up questionnaire: a study of a new rating scale and other measures to evaluate outcome after head injury. J Neurol Neuros Psychiatry 60:510–514
Dikmen S, McLean A, Temkin N (1986) Neuropsychological and psychosocial consequences of minor head injury. J Neurol Neuros Psychiatry 49:1227–1232
Eames PG (2001) Distinguishing the neuropsychiatric, psychiatric, and psychological consequences of acquired brain injury. In: Wood RL, McMillan TH (eds) Neurobehavioural Disability and Social Handicap Following Brain Injury. Psychology Press, Hove, pp. 29–45
Emanuelson I, Andersson Holmkvist E, Björklund R, Stålhammar D (2003) Quality of life and post-concussion symptoms in adults after mild traumatic brain injury: a population-based study in western Sweden. Acta Neurol Scand 108:332–338
Englander J, Hall K, Stimpson T, Chaffin S (1992) Mild traumatic brain injury in an insured population: subjective complaints and return to employment. Brain Inj 6:161–166
Ferrari R, Constantoyannis C, Papadakis N (2001) Cross-cultural study of symptom expectation following minor head injury in Canada and Greece. Clin Neurol Neurosur 103:254–259
Ferrari R, Obelieniene D, Russell A, Darlington P, Gervais R, Green P (2001) Symptom expectation after minor head injury A comparative study between Canada and Lithuania. Clin Neurol Neurosur 103:184–190
Findler M, Cantor J, Haddad L, Gordon W, Ashman T (2001) The reliability and validity of the SF-36 Health Questionnaire for use with individuals with traumatic brain injury. Brain Inj 15:715–723
Frencham KR, Fox AM, Mayberry MT (2005) Neuropsychological studies of mild traumatic brain injury: A meta-analytic review of research since 1995. J Clin Exp Neuropsychol 27:334–351
Gerber DJ, Schraa JC (1995) Mild traumatic brain injury: Searching for a syndrome. J Head Trauma Rehab 10:28–40
Gordon WA, Haddad L, Brown M, Hibbard MR, Sliwinski M (2000) The sensitivity and specificity of self-reported symptoms in individuals with traumatic brain injury. Brain Inj 14:21–33
Gouvier WD, Cubic B, Jones G, Brantley P, Cutlip Q (1992) Postconcussion symptoms and daily stress in normal and head-injured college populations. Arch Clin Neuropsych 7:193–211
Gronwall D (1976) Performance changes during recovery from closed head injury. P Aust Neurol 13:143–147
Gunstad J, Suhr JA (2001) “Expectation as etiology” versus “the good old days”: Postconcussion syndrome symptom reporting in athletes, headache sufferers and depressed individuals. J Int Neuropsych Soc 7:323–333
Gunstad J, Suhr JA (2002) Perception of illness: Nonspecificity of postconcussion syndrome symptom expectation. J Int Neuropsych Soc 8:37–47
Haldorsen T, Waterloo K, Dahl A, Mellgren SI, Davidsen PE, Molin PK (2003) Symptoms and cognitive dysfunction in patients with the late whiplash syndrome. Appl Neuropsych 10:170–175
Hall S, Weinman J, Marteau TM (2004). The motivating impact of informing women smokers of a link between smoking and cervical cancer: The role of coherence. Health Psychol 23:419–424
Hanna-Pladdy B, Berry ZM, Bennett T, Phillips HL, Gouvier WD (2001) Stress as a diagnostic challenge for postconcussive symptoms: Sequelae of mild traumatic brain injury or physiological stress response. Clin Neuropsychol 15:289–304
Iverson GL, McCracken LM (1997) ‘Postconcussive’ symptoms in persons with chronic pain. Brain Inj 11:783–790
Iverson GL, Lange RT (2003) Examination of “postconcussion-like” symptoms in a healthy sample. Appl Neuropsych 10:137–144
Jacobson RR (1995) The post-concussional syndrome: physiogenesis psychogenesis and malingering, an integrative model. J Psychosom Res 39:675–693
Kay T (1993) Neuropsychological treatment of mild traumatic brain injury. J Head Trauma Rehab 8:74–85
King NS (1996) Emotional neuropsychological and organic factors: their use in the prediction of persisting postconcussion symptoms after moderate to mild head injury. J Neurol Neurosurg Psychiatry 61:75–81
King NS (1997) Mild head injury: Neuropathology sequelae measurement and recovery. Brit J Clin Psychol 36:161–184
King NS (2003) Postconcussion syndrome: Clarity amid the controversy. Br J Psychiat 183:276–278
King NS, Crawford S, Wenden FJ, Moss NEG, Wade DT (1995) The Rivermead Post Concussion Symptoms Questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. J Neurol 242:587–592
King NS, Crawford S, Wenden FJ, Moss NEG, Wade DT, Caldwell FE (1997) Measurement of post-traumatic amnesia: How reliable is it? J Neurol Neuros Psychiatry 62:38–42
King NS, Crawford S, Wenden FJ, Caldwell FE, Wade DT (1999) Early prediction of persisting post-concussion symptoms following mild and moderate head injuries. Br J Clin Psychol 38:15–25
Lannoo E, Colardyn F, Vandekerckhove T, Deyne CD, Soete GD, Jannes C (1998) Subjective complaints versus neuropsychological test performance after moderate to severe head injury. Acta Neurochir (Wien) 140:245–253
Lees-Haley PR (1992) Neuropsychological complaint base rates of personal injury claimants. Forensic Reports 5:385–391
Lees-Haley PR, Fox DD, Courtney JC (2001) A comparison of complaints by mild brain injury claimants and other claimants describing subjective experience immediately following their injury. Arch Clin Neuropsych 16:689–695
Levin H, Mattis S, Ruff R, Eisenberg H, Marshall L, Tabaddor K, et al. (1987) Neurobehavioral outcome following minor head injury: a three-center study. J Neurosurg 66:234–243
Lishman WA (1988) Physiogenesis and psychogenesis in the post-concussional syndrome. Br J Psychiatry 153:460–469
Masson F, Maurette P, Salmi LR, Dartigues J-F, Vecsey J, Destaillats J-M, Erny P (1996) Prevalence of impairments 5 years after a head injury and their relationship with disabilities and outcome. Brain Inj 10:487–497
Mazaux JM, Masson F, Levin HS, Alaoui P, Maurette P, Barat M (1997) Long-term neuropsychological outcome and loss of social autonomy after traumatic brain injury. Arch Phys Med Rehab 78:1316–1320
McCauley SR, Boake C, Levin HS, Contant CF, Song JX (2001) Postconcussional disorder following mild to moderate traumatic brain injury: Anxiety depression and social support as risk factors and comorbidities. J Clin Exp Neuropsychol 23:792–808
McCullagh S, Feinstein A (2003) Outcome after mild traumatic brain injury: an examination of recruitment bias. J Neurol Neurosurg Psychiatry 74:39–43
McKinlay WW, Kilfedder C (1992) Financial compensation and head injury. Brain Inj 6:401–410
Mickeviciene D, Schrader H, Nestvold K, Surkiene D, Kunickas R, Stovner LJ, Sand T (2002) A controlled historical cohort study on the post-concussion syndrome. Eur J Neurol 9:581–587
Mickeviciene D, Schrader H, Obelieniene D, Surkiene D, Kunickas R, Stovner LJ, et al. (2004) A controlled prospective inception cohort study on post-concussion syndrome outside the medicolegal context. Eur J Neurol 11:411–419
Middelboe T, Andersen HS, Birket-Smith M, Friis ML (1992) Psychiatric sequelae of minor head injury a prospective follow-up study. Eur Psychiat 7:183–189
Mittenberg W, DiGiulio DV, Perrin S, Bass AE (1992) Symptoms following mild head injury: Expectation as aetiology. J Neurol Neurossurg Psychiatry 55:200–204
Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron LD, Buick D (2002) The Revised Illness Perception Questionnaire (IPQ-R). Psychol Health 17:1–16
Nicholson K, Martelli MF, Zasler ND (2001) Does pain confound interpretation of neuropsychological test results? Neurorehabilitation 16:225–230
Oddy M, Humphrey M, Uttley D (1978) Subjective impairment and social recovery after closed head injury. J Neurol Neurosurg Psychiatry 41:611–616
Oddy M, Coughlan T, Tyerman A, Jenkins D (1985) Social adjustment after closed head injury: a further follow-up seven years after injury. J Neurol Neurosurg Psychiatry 48:564–568
Piland SG, Motl RW, Ferrara MS, Peterson CL (2003) Evidence for the factorial and construct validity of a self-report concussion symptoms questionnaire. J Athl Training 38:104–112
Rapoport MJ, McCullagh S, Streiner D, Feinstein A (2003) The clinical significance of major depression following mild traumatic brain injury. Psychosomatics 44:31–37
Rimel RW, Giordani B, Barth JT, Boll TJ, Jane JA (1981) Disability caused by minor head injury. Neurosurgery 9:221–228
Ruff RM, Camenzuli L, Mueller J (1996) Miserable minority: emotional risk factors that influence the outcome of mild traumatic brain injury. Brain Inj 10:551–565
Russell WR, Smith A (1961) Post traumatic amnesia in closed head injury. Arch Neurol 5:16–29
Rutherford WH, Merrett JD, McDonald JR (1979) Symptoms at one year following concussion from minor head injuries. Injury 10:225–230
Smith-Seemiller L, Fow NR, Kant R, Franzen MD (2003) Presence of post-concussion syndrome symptoms in patients with chronic pain vs mild traumatic brain injury. Brain Inj 17:199–206
Teasdale GM, Jennett B (1974) Assessment of coma and impaired consciousness. Lancet 304:81–84
Trahan DE, Ross CE, Trahan SL (2001) Relationships among postconcussional-like symptoms depression and anxiety in young adults and victims of mild head injury. Arch Clin Neuropsychiatry 16:435–445
Wade DT, Crawford S, Wenden FJ, King NS, Moss NEG (1997) Does routine follow-up after head injury help? A randomised controlled trial. J Neurol Neuros Psychiatry 62:478–484
Wade DT, King NS, Wenden FJ, Crawford S, Caldwell FE (1998) Routine follow up after head injury: A second randomised controlled trial. J Neurol Neurosurg Psychiatry 65:177–183
Wong JL, Regernitter RP, Barrios F (1994) Base rate and simulated symptoms of mild head injury among normals. Arch Clin Neuropsyc 9:411–425
Wood RL (2004) Understanding the ‘miserable minority’: a diasthesis-stress paradigm for post-concussional syndrome. Brain Inj 18:1135–1153
World Health Organization (1992) The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. WHO, Geneva
Wrightson P, Gronwall D (1981) Time off work and symptoms after minor head injury. Injury 12:245–254
Zasler ND, Martelli MF (2003) Mild traumatic brain injury: Impairment and disability assessment caveats. Neuropsychol Rehabil 13:31–41
Acknowledgements
The authors thank the Oxford Head Injury Service (F Caldwell, S Crawford, N King, N Moss & F Wenden) for their work in collecting the original data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Received in revised form: 1 March 2006
Rights and permissions
About this article
Cite this article
Potter, S., Leigh, E., Wade, D. et al. The Rivermead Post Concussion Symptoms Questionnaire. J Neurol 253, 1603–1614 (2006). https://doi.org/10.1007/s00415-006-0275-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0275-z