Abstract
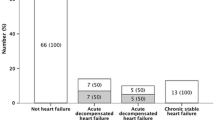
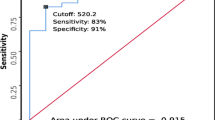
This study aimed to evaluate the effectiveness of digoxin in children with heart failure secondary to left-to-right shunt lesions and normal left ventricular systolic function. The study registered 37 such patients (ages 10 days to 24 months, groups 1 and 2) and used 20 healthy children as a control group (group 3). Left ventricular systolic function, as assessed by conventional echocardiography, was normal in all the subjects. Congestive heart failure was diagnosed by clinical evaluation and modified Ross scoring. Plasma N-terminal prohormone of brain natriuretic peptide (NT-proBNP) concentrations and complete blood counts were assessed in all the children. Group 1 was treated with digoxin, enalapril, and furosemide and group 2 with enalapril and furosemide. Approximately 1 month after starting treatment, the patients were reevaluated by physical and echocardiographic examinations, modified Ross scoring, plasma NT-proBNP concentrations, and complete blood counts. The pre- and posttreatment Ross scores of group 1 (p = 0.377) and group 2 (p = 0.616) did not differ significantly. The NT-proBNP values in both groups decreased after treatment (p = 0.0001). The pre- and posttreatment NT-proBNP values did not differ significantly in group 1 (p = 0.094)) and group 2 (p = 0.372). The pretreatment NT-proBNP values in groups 1 and 2 (p = 0.0001) were significantly higher than in the control group (p = 0.003). A smaller difference was observed between posttreatment NT-proBNP values in group 1 and the control group (p = 0.045). We found no significant difference between the posttreatment NT-proBNP values of group 2 and those of the control group (p = 0.271). The study showed that both treatments currently used to treat heart failure secondary to congenital heart disease with left-to-right shunts and preserved left ventricular systolic function are effective and do not differ significantly. Thus, digoxin does not provide any extra benefit in the treatment of such patients.
Similar content being viewed by others
References
Penny DJ, Vick GW III (2010) Novel therapies in childhood heart failure: today and tomorrow. Heart Fail Clin 6:591–621 x
O’Connor MJ, Rosenthal DN, Shaddy RE (2010) Outpatient management of pediatric heart failure. Heart Fail Clin 6:515–529 ix
Barnes S, Shields B, Bonney W, Hardin J, Abdulla R (2004) The pediatric cardiology pharmacopoeia: 2004 update. Pediatr Cardiol 25:623–646
Kantor PF, Mertens LL (2010) Clinical practice: heart failure in children. Part I: clinical evaluation, diagnostic testing, and initial medical management. Eur J Pediatr 169:269–279
Timberlake K, Kantor PF (2011) Pharmacologic therapy of heart failure in children: part of a special series on paediatric pharmacology, guest edited by Gianvincenzo Zuccotti, Emilio Clementi, and Massimo Molteni. Pharmacol Res 64:427–430
Ross RD (2012) The Ross classification for heart failure in children after 25 years: a review and an age-stratified revision. Pediatr Cardiol 33:1295–1300
Johnstone DE, Abdulla A, Arnold JM, Bernstein V, Bourassa M, Brophy J, Davies R, Gardner M, Hoeschen R, Mickleborough L et al (1994) Diagnosis and management of heart failure. Canadian Cardiovascular Society. Can J Cardiol 10(613–631):635–654
Nir A, Lindinger A, Rauh M, Bar-Oz B, Laer S, Schwachtgen L, Koch A, Falkenberg J, Mir TS (2009) NT-pro-B-type natriuretic peptide in infants and children: reference values based on combined data from four studies. Pediatr Cardiol 30:3–8
Koch A, Zink S, Singer H (2006) B-type natriuretic peptide in paediatric patients with congenital heart disease. Eur Heart J 27:861–866
Cantinotti M, Giovannini S, Murzi B, Clerico A (2011) Diagnostic, prognostic, and therapeutic relevance of B-type natriuretic hormone and related peptides in children with congenital heart diseases. Clin Chem Lab Med 49:567–580
Gessler P, Knirsch W, Schmitt B, Rousson V, von Eckardstein A (2006) Prognostic value of plasma N-terminal pro-brain natriuretic peptide in children with congenital heart defects and open-heart surgery. J Pediatr 148:372–376
Price JF, Thomas AK, Grenier M, Eidem BW, O’Brian Smith E, Denfield SW, Towbin JA, Dreyer WJ (2006) B-type natriuretic peptide predicts adverse cardiovascular events in pediatric outpatients with chronic left ventricular systolic dysfunction. Circulation 114:1063–1069
Tan LH, Jefferies JL, Liang JF, Denfield SW, Dreyer WJ, Mott AR, Grenier MA, Dickerson HA, Price JF, Towbin JA, Ou CN, Chang AC (2007) Concentrations of brain natriuretic peptide in the plasma predicts outcomes of treatment of children with decompensated heart failure admitted to the intensive care unit. Cardiol Young 17:397–406
Puddy VF, Amirmansour C, Williams AF, Singer DR (2002) Plasma brain natriuretic peptide as a predictor of haemodynamically significant patent ductus arteriosus in preterm infants. Clin Sci Lond 103:75–77
Mir TS, Marohn S, Laer S, Eiselt M, Grollmus O, Weil J (2002) Plasma concentrations of N-terminal pro-brain natriuretic peptide in control children from the neonatal to adolescent period and in children with congestive heart failure. Pediatrics 110:e76
Kunii Y, Kamada M, Ohtsuki S, Araki T, Kataoka K, Kageyama M, Nakagawa N, Seino Y (2003) Plasma brain natriuretic peptide and the evaluation of volume overload in infants and children with congenital heart disease. Acta Med Okayama 57:191–197
Shaddy RE (2001) Optimizing treatment for chronic congestive heart failure in children. Crit Care Med 29:S237–S240
Bautista-Hernandez V, Sanchez-Andres A, Portela F, Fynn-Thompson F (2011) Current pharmacologic management of pediatric heart failure in congenital heart disease. Curr Vasc Pharmacol 9:619–628
Berman W Jr, Yabek SM, Dillon T, Niland C, Corlew S, Christensen D (1983) Effects of digoxin in infants with congested circulatory state due to a ventricular septal defect. N Engl J Med 308:363–366
Kimball TR, Daniels SR, Meyer RA, Hannon DW, Tian J, Shukla R, Schwartz DC (1991) Effect of digoxin on contractility and symptoms in infants with a large ventricular septal defect. Am J Cardiol 68:1377–1382
Kothari SS (1997) Does digoxin still have a role in congestive heart failure? Indian J Pediatr 64:833–837
Redington AN, Carvalho JS, Shinebourne EA (1989) Does digoxin have a place in the treatment of the child with congenital heart disease? Cardiovasc Drugs Ther 3:21–24
Nir A, Bar-Oz B, Perles Z, Brooks R, Korach A, Rein AJ (2004) N-terminal pro-B-type natriuretic peptide: reference plasma levels from birth to adolescence: elevated levels at birth and in infants and children with heart diseases. Acta Paediatr 93:603–607
Koch A, Singer H (2003) Normal values of B type natriuretic peptide in infants, children, and adolescents. Heart 89:875–878
Ross RD, Bollinger RO, Pinsky WW (1992) Grading the severity of congestive heart failure in infants. Pediatr Cardiol 13:72–75
Reithmann C, Reber D, Kozlik-Feldmann R, Netz H, Pilz G, Welz A, Werdan K (1997) A post-receptor defect of adenylyl cyclase in severely failing myocardium from children with congenital heart disease. Eur J Pharmacol 330:79–86
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I et al (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2:358–367
Jain S, Vaidyanathan B (2009) Digoxin in management of heart failure in children: should it be continued or relegated to the history books? Ann Pediatr Cardiol 2:149–152
Yoshibayashi M, Kamiya T, Saito Y, Nakao K, Nishioka K, Temma S, Itoh H, Shirakami G, Matsuo H (1995) Plasma brain natriuretic peptide concentrations in healthy children from birth to adolescence: marked and rapid increase after birth. Eur J Endocrinol 133:207–209
Mir TS, Flato M, Falkenberg J, Haddad M, Budden R, Weil J, Albers S, Laer S (2006) Plasma concentrations of N-terminal brain natriuretic peptide in healthy children, adolescents, and young adults: effect of age and gender. Pediatr Cardiol 27:73–77
Cardoso J, Brito MI, Ochiai ME, Novaes M, Berganin F, Thicon T, Ferreira EC, Regina K, Reis CM, Barretto AC (2010) Anemia in patients with advanced heart failure. Arq Bras Cardiol 95:524–528
Ralli S, Horwich TB, Fonarow GC (2005) Relationship between anemia, cardiac troponin I, and B-type natriuretic peptide levels and mortality in patients with advanced heart failure. Am Heart J 150:1220–1227
Wu YR, Chen SB, Huang MR, Zhang YQ, Sun K, Chen S (2005) Diagnostic value of plasma concentration of pro-brain natriuretic peptide in congestive heart failure in pediatric patients with ventricular septal defects. Zhonghua Er Ke Za Zhi 43:161–164
Zhang SR, Zhang YH, Xu Q, Qiu HX, Chen Q (2009) Values of brain natriuretic peptide and N-terminal pro-brain natriuretic peptide in evaluation of cardiac function in children with congenital heart disease. Zhongguo Dang Dai Er Ke Za Zhi 11:429–432
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elkiran, O., Sandikkaya, A., Kocak, G. et al. Evaluation by N-terminal Prohormone of Brain Natriuretic Peptide Concentrations and Ross Scoring of the Efficacy of Digoxin in the Treatment of Heart Failure Secondary to Congenital Heart Disease With Left-to-Right Shunts. Pediatr Cardiol 34, 1583–1589 (2013). https://doi.org/10.1007/s00246-013-0683-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-013-0683-7