Abstract
Summary
In a child, bone mineral density (BMD) may differ from an age-expected normal value, not only because of the presence of disease, but also because of deviations of height or weight from population averages. Appropriate adjustment for body size deviations simplifies interpretation of BMD measurements.
Introduction
For children, a bone mineral density (BMD) measurement is normally expressed as a Z score. Interpretation is complicated when weight or height distinctly differ from age-matched children. We develop a procedure to allow for the influence of body size deviations upon measured BMD.
Methods
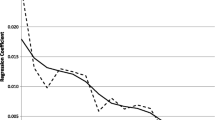
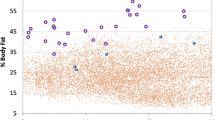
We examined the relation between body size deviation and spine, hip and whole body BMD deviation in 179 normal children (91 girls). Expressions were developed that allowed derivation of an expected BMD based on age, gender and body size deviation. The difference between measured and expected BMD was expressed as a HAW score (Height-, Age-, Weight-adjusted score).
Results
In a second independent sample of 26 normal children (14 girls), measured spine, total femur and whole body BMD all fell within the same single normal range after accounting for age, gender and body size deviations. When traditional Z scores and HAW scores were compared in 154 children, 17.5% showed differences of more than 1 unit and such differences were associated with height and weight deviations.
Conclusion
For almost 1 in 5 children, body size deviations influence BMD to an extent that could alter clinical management.





Similar content being viewed by others
References
Webber CE, Beaumont LF, Morrison J et al (2007) Age predicted values for lumbar spine, proximal femur and whole body bone mineral density; results from a population of normal children aged 3 to 18 years. Can Assoc Radiol J 58:37–45
Jones G, Ma D, Cameron F (2006) Bone density interpretation and relevance in Caucasian children aged 9–17 years of age: insights from a population-based fracture study. J Clin Densit 9:202–209
Goulding A, Jones IE, Taylor RW et al (2000) More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Min Res 15:2011–2018
Ma DQ, Jones G (2002) Clinical risk factors but not bone density are associated with prevalent fractures in prepubertal children. J Paediatr Child Health 38:497–500
Jones IE, Williams SM, Goulding A (2004) Associations of birth weight and length, childhood size and smoking with bone fractures during growth: evidence from a birth cohort study. Am J Epidemiol 159:343–350
Chevalley Y, Rizzoli R, Hans D et al (2005) Interaction between calcium intake and menarcheal age on bone mass gain: an eight year follow-up study from prepuberty to postmenarche. J Clin Endocrinol Metab 90:44–51
Goulding A, Grant AM, Williams SM (2005) Bone and body composition of children and adolescents with repeated forearm fractures. J Bone Min Res 20:2090–2096
Ferrari SL, Chevalley T, Bonjour J-P et al (2006) Childhood fractures are associated with decreased bone mass gain during puberty: an early marker of persistent bone fragility? J Bone Min Res 21:501–507
Rauch F, Neu C, Manz F et al (2001) The development of metaphyseal cortex—implications for distal radius fractures during growth. J Bone Min Res 16:1547–1555
Gafni RI, Baron J (2004) Overdiagnosis of osteoporosis in children due to misinterpretation of dual-energy X-ray absorptiometry (DEXA). J Pediatr 144:253–257
Lu PW, Briody JN, Ogle GD et al (1994) Bone mineral density of total body, spine, and femoral neck in children and young adults: a cross-sectional and longitudinal study. J Bone Min Res 9:1451–1458
Mølgaard C, Thomsen BL, Prentice A et al (1997) Whole body bone mineral content in healthy children and adolescents. Arch Dis Child 76:9–15
Warner JT, Cowan FJ, Dunstan FDJ et al (1998) Measured and predicted bone mineral content in healthy boys and girls aged 6–16 years: adjustment for body size and puberty. Acta Paediatr 87:244–249
Fewtrell MS, Gordon I, Biassoni L et al (2005) Dual X-ray absorptiometry (DXA) of the lumbar spine in a clinical paediatric setting: does the method of size adjustment matter? Bone 37:413–419
Prentice A, Parsons TJ, Cole TJ (1994) Uncritical use of bone mineral density in absorptiometry may lead to size-related artifacts in the identification of bone mineral determinants. Am J Clin Nutr 60:837–842
Horlick M, Wang J, Pierson RN et al (2004) Prediction models for evaluation of total-body bone mass with dual-energy X-ray absorptiometry among children and adolescents. Pediatrics 114:e337–e345
Centers for Disease Control and Prevention. Clinical growth charts. Available at: http://www.cdc.gov/growthcharts, Accessed December 2006
Sala A, Webber CE, Morrison J et al (2007) Whole body mineral mass, lean body mass and fat mass measured by dual photon absorptiometry in a population of normal Canadian children and adolescents. Can Assoc Radiol J 58:46–52
Binkoviyz LA, Henwood MJ (2007) Pediatric DXA: technique and interpretation. Pediatr Radiol 37:21–31
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Webber, C.E., Sala, A. & Barr, R.D. Accounting for body size deviations when reporting bone mineral density variables in children. Osteoporos Int 20, 113–121 (2009). https://doi.org/10.1007/s00198-008-0642-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0642-y