Abstract
Purpose
Due to the juvenility of research in the field of periprosthetic joint infection (PJI), approaches employed for diagnosis of PJI vary amongst surgeons in different geographic regions. The aim of this study was to determine common diagnostic approaches utilized by European knee arthroplasty surgeons for the diagnosis of PJI.
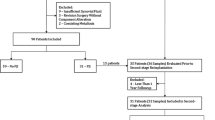
Methods
A task force was established for questionnaire development, consisting of surgeons and clinical researchers who each had a record of publishing in the field of PJI. A pool of items was initially generated from a Medline literature search. These were organized into a file and independently sent to each task force member for evaluation and additional supplementation. After reaching a consensus, a final online version was generated and administered to all 4865 members of the “European Society of Sports Traumatology Knee Surgery & Arthroscopy”.
Results
There were 262 respondents between August 2015 and March 2016. Most European surgeons (41.1 %) diagnose between 2 and 5 PJIs yearly, and only 5.8 % diagnose >30 PJIs per year. Serum tests to rule out infection were commonly CRP (97.7 %), leucocyte count (73.6 %) and microbiology cultures (45.3 %), while serum interleukins were least common (<5 %). Synovial fluid exams most commonly included microbiology (97.7 %), leucocyte count (74.8 %), percentage polymorphonuclear cells (65.8 %), synovial fluid CRP (26.4 %) and α-defensin (19.4 %). Conventional radiographs represent the most common radiographic exam (87.6 %) followed by SPECT-CT scans (41.7 %). The majority (93.6 %) take biopsies at the time of surgery, 62.0 % take 1–5 biopsies, and 34.9 % take >5. Most biopsies (98.8 %) are sent for culture exams and 72.5 % for histology, and 36.4 % of surgeons send the implants for sonication.
Conclusion
Microbiology and cell count remain the most commonly applied synovial fluid tests in Europe, while α-defensin and leucocyte esterase are currently less common. Serum interleukins have not gained widespread use. Implant sonication, despite evidence of diagnostic effectiveness, was only applied by one-third of survey respondents, highlighting the problematic issues of cost and accessibility of some tools. The results highlight the current state of European diagnostic practice, emphasizing the areas of divergence from state of evidence and demonstrating the need for development of standard diagnostic algorithms.
Level of evidence
Cross-sectional survey, Level IV.




Similar content being viewed by others
References
Ahmad SS, Shaker A, Saffarini M, Chen AF, Hirschmann MT, Kohl S (2016) Accuracy of diagnostic tests for prosthetic joint infection: a systematic review. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4230-y
Begg CB, Cramer LD, Hoskins WJ, Brennan MF (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280(20):1747–1751
Berbari E, Mabry T, Tsaras G, Spangehl M, Erwin PJ, Murad MH, Steckelberg J, Osmon D (2010) Inflammatory blood laboratory levels as markers of prosthetic joint infection. J Bone Joint Surg Am 92(11):2102–2109
Bilgen O, Atici T, Durak K, Karaeminogullari Bilgen MS (2001) C-reactive protein values and erythrocyte sedimentation rates after total hip and total knee arthroplasty. J Int Med Res 29(1):7–12
Bottner F, Wegner A, Winkelmann W, Becker K, Erren M, Gotze C (2007) Interleukin-6, procalcitonin and TNF-alpha: markers of periprosthetic infection following total joint replacement. J Bone Joint Surg Br 89(1):94–99
Font-Vizcarra L, García S, Martínez-Pastor JC, Sierra JM, Soriano A (2010) Blood culture flasks for culturing synovial fluid in prosthetic joint infections. Clin Orthop Relat Res 468(8):2238–2243
Gbejuade HO, Lovering AM, Webb JC (2015) The role of microbial biofilms in prosthetic joint infections. Acta 86(2):147–158
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Kwee TC, Kwee RM, Alavi A (2008) FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur J Nucl Med Mol Imaging 35(11):2122–2132
Ouyang Z, Li H, Liu X, Zhai Z, Li X (2014) Prosthesis infection: diagnosis after total joint arthroplasty with three-phase bone scintigraphy. Ann Nucl Med 28(10):994–1003
Pakos EE, Trikalinos TA, Fotopoulos AD, Ioannidis JP (2007) Prosthesis infection: diagnosis after total joint arthroplasty with antigranulocyte scintigraphy with 99mTc-labeled monoclonal antibodies—a meta-analysis. Radiology 242(1):101–108
Parvizi J, Gehrke T, Chen A (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J 95(11):1450–1452
Qu X, Zhai Z, Wu C, Jin F, Li H, Wang L, Liu G, Liu X, Wang W, Li H (2013) Preoperative aspiration culture for preoperative diagnosis of infection in total hip or knee arthroplasty. J Clin Microbiol 51(11):3830–3834
Sadiq S, Wootton JR, Morris CA, Northmore-Ball MD (2005) Application of core biopsy in revision arthroplasty for deep infection. J Arthroplasty 20(2):196–201
Zhai Z, Li H, Qin A, Liu G, Liu X, Wu C, Li H, Zhu Z, Qu X, Dai K (2014) Meta-analysis of sonication fluid samples from prosthetic components for diagnosis of infection after total joint arthroplasty. J Clin Microbiol 52(5):1730–1736
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding was received for the conduction of this study.
Ethical approval
For this type of study, formal consent is not required.
Informed consent
None.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Ahmad, S.S., Becker, R., Chen, A.F. et al. EKA survey: diagnosis of prosthetic knee joint infection. Knee Surg Sports Traumatol Arthrosc 24, 3050–3055 (2016). https://doi.org/10.1007/s00167-016-4303-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4303-y