Abstract
Purpose
The multiple inert gas elimination technique (MIGET) is the reference method for evaluating pulmonary gas exchange. MIGET includes a complex experimental method and mathematical model, and has not been used routinely in clinical practice. A simpler mathematical model has been proposed, and was shown previously to fit inert gas data from oleic acid damage. This paper explores the capability of this simple model to describe more complex damage, and to calculate oxygenation data upon changing the inspired oxygen fraction (FIO2), comparing these results with those obtained using MIGET.
Methods
The comparison of oxygenation was done at different ventilator settings and at varying values of FIO2 in order to mimic the clinical conditions that occur in the intensive care unit.
Results
The simple model describes inert gas data from heterogeneous lung damage within measurement noise. Model simulations performed using the MIGET and the simple model are comparable, the MIGET model simulating partial pressure of oxygen (PaO2) values on average 0.22 ± 0.59 kPa (±SD) higher than the simple model. Model simulations are also accurate with a difference between model simulated and measured values of PaO2 of 0.33 ± 1.48 kPa (±SD) for the MIGET model and 0.12 ± 1.33 kPa (±SD) for the simple model. This comparability and accuracy was similar over different ventilator settings.
Conclusions
The simple model provides a description of lung damage and arterial oxygenation which is comparable to the MIGET, calculating PaO2 with acceptable accuracy and precision over the clinically relevant range of PaO2, and for different values of FIO2, positive end-expiratory pressure (PEEP), and inspiratory-to-expiratory ratio (I:E).
Similar content being viewed by others
Introduction
The multiple inert gas elimination technique (MIGET) is the reference method for describing pulmonary gas exchange [1, 2]. MIGET includes a complex experimental method involving infusion and measurement of six inert tracer gases. Data are analyzed using a multicompartmental mathematical model describing the lungs as 50 compartments, each with different ventilation–perfusion (\( \dot{V}/\dot{Q} \)) ratios ranging from 0 (i.e., pulmonary shunt) to infinity (i.e., alveolar dead space). The method is demanding and requires trained staff. Taken together, this is perhaps why the method has not been used routinely in clinical practice.
However, major causes of impaired oxygenation and hypoxemia are limited to shunt and low \( \dot{V}/\dot{Q} \) (with the addition of alveolar hypoventilation and diffusion). Thus, a bedside and simpler technique that enables distinction between shunt and low \( \dot{V}/\dot{Q} \) would be helpful. Causes of shunt can then be separated from causes of low \( \dot{V}/\dot{Q} \), better enabling the clinician to decide on specific therapeutic interventions.
In the clinical setting simpler, single-parameter methods are used to describe disorders in pulmonary gas exchange, these including measurements of arterial oxygen saturation (SaO2), PaO2/FIO2 ratio, and calculation of effective shunt [3]. These single-parameter descriptions are insufficient, being unable to describe shunt and \( \dot{V}/\dot{Q} \) matching or to simulate changes in arterial oxygenation on varying FIO2 [4–7].
Recently, a simpler model has been presented [8, 9]. This represents the lung as four different compartments: anatomical dead space, shunt, and then two gas exchange compartments with different \( \dot{V}/\dot{Q} \) ratios. When assuming a fixed anatomical dead space it is possible to estimate model parameters upon stepwise changes in FIO2 using routinely available clinical measurements of ventilation, circulation, and blood acid–base status. The experiment can be done in only 10–15 min and may be automatized [10].
It is possible, therefore, to hypothesize a role for the simple model in quantifying gas-exchange abnormalities in the clinical setting. This role is dependent upon the simple model being able to represent complex lung abnormalities seen in the ICU, and its ability to accurately describe oxygenation. To do so the model requires comparison with the MIGET technique.
The capability of this simpler model to describe inert gas data obtained from MIGET has, in part, been explored previously [11]. It was shown that the simple model provided a good fit to data describing retention and excretion of inert gases in the lungs of pigs with oleic acid lung damage, the errors in this fit being in line with those expected due to measurement error rather than model limitations. However, further evaluation is required as the clinical role of the simple model is dependent on it being able to represent more complex lung abnormalities; and that it can also describe oxygenation data in a way comparable to MIGET.
This paper explores the capability of this simple model to both describe inert gas data in heterogeneous lung damage and to reproduce oxygenation data in pigs with lung damage caused by oleic acid infusion, comparing these results with those obtained using MIGET’s multicompartmental model. The comparison between the simple and MIGET models’ reproduction of oxygenation data has been performed at different ventilator settings and at varying values of FIO2 to mimic the clinical conditions of the ICU.
Methods
Two data sets have been used. Data set 1 is used to evaluate the capability of the simple model to describe inert gas data in heterogeneous lung damage, and data set 2 to evaluate the ability of the simple model to reproduce oxygenation data when compared to MIGET. For both data sets, studies were performed in the experimental laboratory of the Department of Clinical Physiology, Uppsala University Hospital, Uppsala, Sweden. Approval was granted by the local animal ethics committee, and the study was performed according to the National Research Council guide for “Principles of laboratory animal care”.
Data set 1
Study protocol
Three pigs were anesthetized and mechanically ventilated. Lung injury was subsequently induced by using lung lavage. Subsequently, animals were ventilated at zero end-expiratory pressure (ZEEP), and a determination of ventilation–perfusion distribution was performed by using MIGET. Details of anesthesia, ventilation, monitoring, and lung injury can be found in the “Electronic supplementary material” (ESM).
Data set 2
Study protocol
Seven pigs (median weight 27.5, range 26.4–31.5 kg) were anesthetized and mechanically ventilated and a determination of ventilation–perfusion distribution was performed by using MIGET. Lung injury was subsequently induced by using infusion of oleic acid. After allowing for stabilization of the lung injury for 90 min, a series of experiments involving changing the inspired oxygen fraction (FIO2) were performed at different levels of PEEP and inspiratory-to-expiratory ratio (I:E) (5, 10, 18, and 10 cmH2O at I:E = 2:1). Before each experiment a determination of \( \dot{V}/\dot{Q} \) distributions was performed by using MIGET. Inert gas and ventilation data have been used in a previous publication [11]. Details of anesthesia, ventilation, monitoring, and lung injury can be found in the ESM.
FIO2 variation
FIO2 was changed in 4–5 steps as described previously [8]. After each change an equilibration period of 5 min ensured steady state for oxygenation. After equilibration a number of measurements were taken at each FIO2 and at each ventilator setting. These included: arterial and mixed venous blood gases; ventilation volumes taken from the ventilator; inspired and end-expired oxygen (FIO2 and FEO2) and end-expired carbon dioxide (FECO2); mixed expired O2 and CO2; and cardiac output.
Calculation of \( \dot{V}/\dot{Q} \) distributions
Six inert tracer gases with different solubility in blood (sulfur hexafluoride, ethane, cyclopropane, enflurane, ether, and acetone) were dissolved in isotonic saline and infused in a peripheral vein. The inert gases were removed from blood samples, and the concentrations of inert gases in blood and expired gases were measured by using gas chromatography (5890, series 2, Hewlett-Packard) [1]. These data were used to obtain the “measured” (m) retention (Rm) and excretion (Em) of the inert gases (i), where retention is the ratio of the pressure of the inert gas in the arterial (Pa) to mixed venous (Pv) blood and excretion is the ratio of the pressure of the inert gas in the mixed expired gases (PE) to Pv, i.e.,
Simultaneous samples of mixed venous blood, arterial blood, and mixed expired gas were taken. Standard blood gas analysis of the arterial and mixed venous blood was performed (Radiometer ABL 525, Copenhagen, Denmark).
Modelling methods
For both data sets the multicompartmental MIGET model [1] and the simpler model were used to recover the \( \dot{V}/\dot{Q} \) distributions for each model using the information obtained from inert gas measurements [11].
For data set 2, the recovered \( \dot{V}/\dot{Q} \) distributions of the models were then used to calculate arterial oxygenation data when FIO2 was varied.
The MIGET model
An implementation of the MIGET model similar to that reported by West and Wagner [12] was built for the occasion. The structure of this model is shown in Fig. 1, where each compartment is represented by a gas and blood phase, the latter of which includes a model of acid–base and oxygenation status [13]. The MIGET model describes pulmonary gas exchange by 50 compartments each with unique \( \dot{V}/\dot{Q} \) ratios, i.e., alveolar dead space, shunt, and 48 compartments involved in gas exchange.
The figure shows the structure of the two models. The MIGET model includes 50 compartments all with predefined ventilation/perfusion (\( \dot{V}/\dot{Q} \)) ratios ranging from shunt, i.e., \( \dot{V}/\dot{Q} \)(1) = 0, to alveolar dead space, i.e., \( \dot{V}/\dot{Q} \)(50) = ∞. The simple model includes two alveolar compartments, where the flow to compartment 2, Q(2), is fixed at 90% of the non-shunted blood flow (fpas2), and gas exchange is described by anatomical dead space (V D), the fraction of ventilation to compartment 2 (fA2) and shunt. The insert represents a single compartment of each model. The gas phase is described by the partial pressures of oxygen and carbon dioxide (PaO2, PaCO2) which are equivalent to the partial pressures in the blood. The blood phase is represented by a mathematical model of acid–base and oxygenation status [13], which enables calculation of concentrations (tO2, tCO2) from partial pressures, and hence mixing of blood from the various compartments
The simple model
The structure of this model is illustrated in Fig. 1, where each compartment is represented by a gas and blood phase including a model of acid–base and oxygenation status [13]. The simple model describes pulmonary gas exchange by anatomical dead space volume (V D), pulmonary shunt (shunt), and two compartments receiving both ventilation and perfusion. These two compartments are described by a single parameter (fA2), the fraction of alveolar ventilation going to compartment 2. The fraction of perfusion to the alveolar compartment 2 (fp2) is fixed at 90% of the non-shunted blood flow to enable the two compartments to simulate a variety of disorders by varying only fA2. By fixing fp2 at 90%, the ventilation and \( \dot{V}/\dot{Q} \) ratio of each compartment can be calculated. If the ventilation distribution is also 10 and 90% (i.e., fA2 = 0.9), the model simulates normal gas exchange. The maximal disorder that can be simulated is all ventilation going to 10% of the perfusion (i.e., fA2 = 0). Fixing the perfusion and estimating the ventilation and \( \dot{V}/\dot{Q} \) ratio is similar to MIGET, where the \( \dot{V}/\dot{Q} \) ratios of the compartments are fixed and the ventilation and perfusion estimated.
For both the MIGET and simple model, simulations of changes in FIO2 were performed by providing measured values of mixed venous oxygenation as input to the model and simulating arterial oxygenation for different values of FIO2 (PaO2s). PaO2s was simulated for each value of FIO2 assuming that the gas exchange properties of the lungs, as described by the \( \dot{V}/\dot{Q} \) ratios recovered from the inert gas measurements, remained constant at each value of FIO2.
Data analysis and statistical methods
Analysis was performed to explore the capability of the simple model to describe the heterogeneous lung damage seen in data set 1. To do so the difference between model simulated and measured values of retention and excretion were assessed in relation to measurement error.
To assess the ability of the simple model to simulate clinical changes in oxygenation, data were selected from data set 2 so as to mimic the clinical situation. In the ICU, mechanical ventilation is usually a compromise between ensuring optimal oxygenation and pH and protecting the patients’ lungs from high pressures/volumes and oxygen toxicity. Data were therefore selected where arterial oxygenation was within a clinically relevant range, in this study defined as 7 kPa ≤ PaO2 ≤ 20 kPa, i.e., excluding data taken at very low or high values of PaO2. In this way 62 data sets were included from data set 2, these data coming from 3 ventilator settings (PEEP = 5 cmH2O, PEEP = 10 cmH2O, and PEEP = 10 cmH2O with I:E = 2:1), all from animals following lung damage with oleic acid.
Three questions were asked using this data set, in regards to simulating oxygenation:
-
1.
Did the MIGET and the simple model provide accurate and comparable predictions of arterial oxygenation for the value of FIO2 where the inert gas measurement was taken?
-
2.
Did the MIGET and the simple model give accurate and comparable predictions of PaO2 for all values of FIO2?
-
3.
Did the MIGET and simple model give accurate and comparable predictions of PaO2 across a range of PEEP and I:E settings compatible with clinical treatment of acute lung injury? Changes in PEEP and inverse ratio were selected to be typical of those used to achieve and maintain lung recruitment, and to prevent air trapping.
Questions 1 and 2 were differentiated, as question 1 deals only with the question as to whether the models have sufficient complexity to simulate PaO2. Question 2 deals not only with the necessary complexity of the models, but also as to whether significant physiological effects such as hypoxic vasoconstriction are present on changing FiO2. If so, neither model would be able to simulate correctly PaO2 regardless of the level of complexity. The values of PaO2s simulated by both models were compared to each other and to measured values of PaO2. Results are represented as Bland–Altman plots.
Results
Figure 2 illustrates the results of MIGET analysis and simple model fitting to retention and excretion data for data set 1. Column 1 illustrates the MIGET analysis, showing the heterogeneous nature of the damage as bimodal distributions of ventilation and perfusion, and substantial perfusion within the low V/Q region (0.005 < V/Q < 0.1). Columns 2 and 3 illustrate the simple model’s fit to measured values of retention and excretion. The simple model fitted measurements well, with the difference between the measured and model calculated values having a median and range of 0.009 (0–0.038), in line with percent standard deviation of measurement error of MIGET inert gasses, which range from 1.8 to 5.7% [14].
Measured inert gas data, and MIGET and simple model analysis. Each row represents the data from a single animal. Column 1 illustrates the results of MIGET analysis illustrating the perfusion (solid line) and ventilation (dashed line) distributions. Column 2 illustrates the best fit of the simple model (crosses), and measured values (circles, lines) of the retention of each of the six inert gasses. Column 3 illustrates the best fit of the simple model (crosses), and measured values (circles, lines) of the excretion of each of the six inert gasses
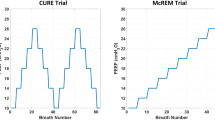
Figure 3 illustrates the comparability (Fig. 3a) and accuracy (Fig. 3b) of simulations performed by using the two models, at the value of FIO2 where the inert gas measurement was performed for data set 2. Fifteen measurements are included for each of these plots, these being selected as those where PaO2 was within the range 7 kPa ≤ PaO2 ≤ 20 kPa. Simulations performed using the MIGET and the simple model are comparable as shown in Fig. 3a, with the MIGET model simulating values of PaO2 on average 0.24 ± 0.51 kPa (±SD) higher than the simple model. Simulations performed by both models are also accurate as shown in Fig. 3b, with only a small difference between model simulated and measured values of PaO2 for the MIGET model [0.22 ± 0.85 kPa (±SD)] and the simple model [−0.02 ± 0.78 kPa (±SD)].
The figure shows the comparability (a) and accuracy (b) of model simulations. In a circles describe the difference between simulations made with the MIGET and simple models, and solid lines represent the mean ± 2SD of these differences. In b stars and squares describe the difference between model simulated and measured values for simulations performed with the MIGET (stars) and simple (squares) models. Solid and dashed lines represent the mean ± 2SD of these differences for simulations made with the MIGET (solid lines) and simple (dashed lines) models
Figure 4 illustrates the comparability (Fig. 4a) and accuracy (Fig. 4b) of simulations performed by using the two models, at all FIO2 values for data set 2, at all ventilator settings. Sixty-two measurements are included in these plots, these being selected as those where PaO2 was within the range 7 kPa ≤ PaO2 ≤ 20 kPa. Simulations performed using the MIGET and the simple model are comparable as shown in Fig. 4a, with the MIGET model simulating values of PaO2 on average 0.22 ± 0.59 kPa (±SD) higher than the simple model. Simulations performed by both models are also accurate as shown in Fig. 4b, with the difference between model predicted and measured values of PaO2 being almost the same for the two models, i.e., 0.33 ± 1.48 kPa (±SD) (MIGET model) and 0.12 ± 1.33 kPa (±SD) (simple model). The ESM illustrates the comparability and accuracy of model predictions for each of the different ventilator settings, showing similar results to the group as a whole.
a The comparability of model simulations at all FIO2 levels for all ventilator settings. Circles are the data from Fig. 3a, i.e., at baseline FIO2. Crosses describe the difference between simulations made with the MIGET and simple models at other FIO2 levels, and solid lines represent the mean ± 2SD of all these differences. b The accuracy of model simulations at all FIO2 levels for all ventilator settings. Stars and squares are the data from Fig. 3b, i.e., at baseline FIO2. Diagonal crosses and inverted triangles represent the difference between model simulated and measured values for simulations performed with the MIGET (diagonal crosses) and simple (inverted triangles) models. Solid and dashed lines represent the mean ± 2SD of these differences for simulations made with the MIGET (solid lines) and simple (dashed lines) models
Discussion
The MIGET is a complex mathematical model and experimental method which has provided insight into pathophysiological changes in pulmonary gas exchange [2, 15, 16]. However, the MIGET has, due to its complexity, not been used routinely in clinical practice. It has been shown that simpler models, such as that presented here, can be identified from routinely available clinical data [9, 10] and may therefore be useful in a clinical setting. In evaluating the role of this simpler model it is necessary to compare it against the reference method, this being the MIGET.
It has previously been shown [11] that the simpler model was capable of giving a good description of inert gas data in lung damage caused by oleic acid, and that the values of parameters of the simple model estimated by fitting to these data [dead space volume (V D), shunt, and the fraction of alveolar ventilation going to compartment 2 (fA2)] compared well with the similar MIGET parameters [dead space volume (V D), shunt, log of the standard deviation of the perfusion (log SDQ), log of the standard deviation of the ventilation (log SDV)]. However, showing that the simple model provides an adequate description of inert gas data following oleic acid damage is not sufficient justification for its clinical application. The simple model should also be able to simulate inert gas data in heterogeneous lung damage and be able to simulate arterial oxygenation in a comparable way to the MIGET model, providing simulations which accurately reflect arterial oxygen measurements. If true then the simple model, along with a computer-controlled variation in FIO2 [10], might provide a simple clinical tool for describing pulmonary gas exchange.
This paper has explored the capability of the simple model to describe inert gas data in selected cases of very heterogeneous lung damage, illustrating the ability of the model to describe such data within measurement error. The paper has also explored the capability of both the MIGET and the simple model to describe oxygenation data obtained at different ventilator settings and at different values of FIO2. The models are able to accurately reproduce the PaO2 at the FIO2 where the inert gas measurement was performed as shown in Fig. 3. Figure 4 shows that the simple model provides a description of arterial oxygenation at different values of FIO2 which is accurate and comparable to the MIGET, across a range of ventilator settings and arterial oxygenation levels consistent with clinical practice. As such, the simple and MIGET models might be interchangeable in a clinical setting where only limited amounts of data are readily accessible.
To perform simulations of arterial oxygen levels at different values of FIO2, previously estimated values of model parameters have been used. This also implies that, in addition to comparing the two models, this study explores the potential physiological changes that might occur upon changing the ventilator setting and the FIO2. Fixing model parameters and accurately simulating PaO2 values across a range of FIO2 levels suggests that there were no significant physiological changes, e.g., hypoxic vasoconstriction, caused by modifying FIO2.
A potential limitation to the findings is that oleic acid induces a quite homogeneous lung damage. However, this paper illustrates that the simple model can reproduce more complex lung damage. The ability of the simple model to simulate changes in oxygenation should be dependent on mechanisms such as hypoxic vasoconstriction or absorption atelectasis, rather than the heterogeneity of the lung damage, and as such oleic acid represents a reasonable lung damage model to address this question. In addition, it is important to recognize that the simpler model is intended to serve as a tool to describe individual patients gas exchange in a clinical setting where only a limited amount of data are readily accessible. In this context using the simple model represents a significant improvement to the usual clinical standard describing oxygenation problems, i.e., calculation of effective shunt, alveolar–arterial oxygen difference, or P/F ratio [6, 7]. The model could therefore have applications in different clinical situations, where more complex experiments such as the MIGET are not practical. In addition it could have application in the experimental setting, replacing single-parameter descriptions of gas exchange such as PaCO2, P/F ratio, or effective shunt, when evaluating the effects on gas exchange of maneuvers such as posture change [17, 18] or variation in lung pressures [18, 19].
In summary, the simple model can describe heterogeneous lung abnormalities. It also provides a description of arterial oxygenation at different values of FIO2 comparable to the MIGET, simulating PaO2 values with acceptable accuracy and precision.
References
Wagner PD, Saltzman HA, West JB (1974) Measurement of continuos distributions of ventilation–perfusion ratios: theory. J Appl Physiol 36:588–599
Melot C (1994) Contribution of the multiple inert elimination technique to pulmonary medicine. 5. Ventilation–perfusion relationships in acute respiratory failure. Thorax 49:1251–1258
Wandrup JH (1995) Quantifying pulmonary oxygen transfer deficits in critically ill patients. Acta Anaesthesiol Scand 39:37–44
Andreassen S, Rees SE, Kjaergaard S, Thorgaard P, Winter SM, Morgan CJ, Alstrup P, Toft E (1999) Hypoxemia after coronary bypass surgery modeled by resistance to oxygen diffusion. Crit Care Med 27:2445–2453
Petros AJ, Doré CJ, Nunn JF (1994) Modification of iso-shunt lines for low inspired oxygen fractions. Br J Anaesth 72:5–15
Karbing DS, Kjærgaard S, Smith BW, Espersen K, Allerød C, Andreassen S, Rees SE (2007) Variation in the PaO2/FiO2 ratio with FiO2: mathematical and experimental description, and clinical relevance. Crit Care 11:R118
Wagner PD (2007) Assessment of gas exchange in lung disease: balancing accuracy against feasibility. Crit Care 11:182
Kjærgaard S, Rees SE, Nielsen JA, Freundlich M, Thorgaard P, Andreassen S (2001) Modelling of hypoxaemia after gynaecological laparotomy. Acta Anaesthesiol Scand 45:349–356
Kjærgaard S, Rees S, Malczynski J, Nielsen JA, Thorgaard P, Toft E, Andreassen S (2003) Noninvasive estimation of shunt and ventilation–perfusion mismatch. Intensive Care Med 29:727–734
Rees SE, Kjærgaard S, Thorgaard P, Malczynski J, Toft E, Andreassen S (2002) The automatic lung parameter estimator (ALPE) system: non-invasive estimation of pulmonary gas exchange parameters in 10–15 minutes. J Clin Monit Comput 17:43–52
Rees SE, Kjærgaard S, Andreassen S, Hedenstierna G (2006) Reproduction of MIGET retention and excretion data using a simple model of gas exchange in lung damage caused by oleic acid infusion. J Appl Physiol 101:826–832
West JB, Wagner PD (1977) Pulmonary gas exchange. In: West JB (ed) Bioengineering aspects of the lung. Marcel Dekker, New York, pp 361–454
Rees SE, Andreassen S (2005) Mathematical models of oxygen and carbon dioxide storage and transport: the acid–base chemistry of blood. Crit Rev Biomed Eng 33:209–264
Wagner PD, Naumann F, Laravuso RB (1974) Simultaneous measurement of eight foreign gases in blood by gas chromatography. J Appl Physiol 36:600–605
Hachenberg T, Tenling A, Nystrom SO, Tyden H, Hedenstierna G (1994) Ventilation–perfusion inequality in patients undergoing cardiac surgery. Anesthesiology 80:509–519
Hedenstierna G, Tokics L, Strandberg A, Lundquist H, Brismar B (1986) Correlation of gas exchange impairment to development of atelectasis during anaesthesia and muscle paralysis. Acta Anaesthesiol Scand 30:183–191
Schellongowski P, Losert H, Locker GJ, Laczika K, Frass M, Holzinger U, Bojic A, Staudinger T (2007) Prolonged lateral steep position impairs respiratory mechanics during continuos lateral rotation therapy in respiratory failure. Intensive Care Med 33:625–631
Protti A, Chiumello D, Cressoni M, Carlesso E, Mietto C, Berto V, Lazzerini M, Quintel M, Gattinoni L (2009) Relationship between gas exchange response to prone position and lung recruitability during acute respiratory failure. Intensive Care Med 35:1011–1017
Caramez MP, Kacmarek RM, Helmy M, Miyoshi E, Malhotra A, Amato MB, Harris RS (2009) A comparison of methods to identify open-lung PEEP. Intensive Care Med 35:740–747
Conflict of interest
SER, SCK, and SA are shareholders and SER is a board member of Mermaid Care A/S, a company which produces equipment for the measurement of pulmonary gas exchange.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rees, S.E., Kjærgaard, S., Andreassen, S. et al. Reproduction of inert gas and oxygenation data: a comparison of the MIGET and a simple model of pulmonary gas exchange. Intensive Care Med 36, 2117–2124 (2010). https://doi.org/10.1007/s00134-010-1981-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1981-7