Abstract
Objective
Hospital mortality increases if acutely ill patients are admitted to hospitals on weekends as compared with weekdays. Night discharges may increase mortality in intensive care unit (ICU) patients but the effect of ICU admission time on mortality is not known. We studied the effects of ICU admission and discharge times on mortality and the time of death in critically ill patients.
Design
Cohort study using a national ICU database.
Setting
Eighteen ICUs in university and central hospitals in Finland.
Patients
Consecutive series of all 23,134 emergency admissions in January 1998–June 2001.
Interventions
None.
Measurements and main results
We defined weekend (as opposed to weekday) from 1600 hours Friday to 2400 hours Sunday and “out-of-office” hours (as opposed to “office hours”) from 1600 hours to 0800 hours. Mortality was adjusted for disease severity, intensity of care, and whether restrictions for future care were set. ICU-mortality was 10.9% and hospital mortality 20.7%. Adjusted ICU-mortality was higher for weekend as compared with weekday admissions [odds ratio (OR 1.20) 95% CI 1.01–1.43], but similar for “out-of-office” and “office hour” admissions (OR 0.98, 0.85–1.13). Adjusted risk of ICU death was higher during “out-of-office” hours as compared with office hours (OR 6.89, 5.96–7.96). The time of discharge from ICU to wards was not associated with further hospital mortality.
Conclusions
Weekend ICU admissions are associated with increased mortality, and patients in the ICU are at increased risk of dying in evenings and during nighttime. Our findings may have important implications for organization of ICU services.
Similar content being viewed by others
Introduction
Patients with acute, serious medical conditions are more likely to die, if they are admitted to hospital on weekends as compared with weekdays [1]. In critically ill patients the effect of admission time to intensive care unit (ICU) on mortality is not known, but it is well-known that organizational aspects of care affect outcome [2, 3, 4]. Mortality is lower in ICUs where there is a 24-h cover by intensivists and mortality may increase if staff workload increases [5, 6]. In addition, night discharges from intensive care, e.g., due to lack of beds, may be associated with increased risk of death [7]. It is likely that during weekends and at nighttime most ICUs lack the most experienced staff. A recent report on hospitalized acutely, but non-critically, ill patients suggested that the difference in mortality between weekday and weekend admissions would be most prominent in patients with complex disorders with high associated mortality [1]. Critically ill patients typically fit this criteria but the effect of the time of admission to intensive care on mortality has not been studied. Further, the overall effects of admission and discharge times on outcome, taking into account disease severity and intensity of care, are not known in critically ill patients. In addition, it is not known whether the risk of death in the ICU is the same during daytime as compared with evenings and nighttime or during weekends as compared with weekdays.
We aimed to investigate the effects of ICU admission and discharge times on ICU and hospital mortality in consecutive critically ill patients who underwent emergency admission to intensive care during a period of 3.5 years in Finland. We also studied the potential differences in the risk of death in the ICU comparing weekdays with weekends and daytimes with evenings/nighttime. We also took into account severity of disease, intensity of care while patients were in ICUs, and potentially set restrictions for future care as confounders for mortality.
Materials and methods
Our study was approved by the Ethics committee of Kuopio University Hospital. Several Finnish ICUs started a quality assurance project, “The Finnish Consortium of Intensive Care Data” in 1994. The main aim of this consortium is to measure the quality of care and performance of different ICUs. Detailed data of disease severity, intensity of care, outcome, admission and discharge times, and time of death in the ICU are prospectively collected into a single database. The data collection was handled by Intensium, Finland. We used this data for the purpose of our study.
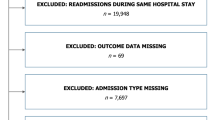
During the period of January 1998–June 2001, 31,840 patients were entered into the database in 18 intensive care units in Finland. These ICUs represent approximately 80% of all adult ICUs in Finland. Sixteen units were ICUs in central hospitals (secondary referral centers) and two ICUs were in university hospitals (tertiary referral center). Each of the ICUs mainly treated adult patients. We did not have any specifically pediatric ICUs in our database. The ICUs that were included in this study were geographically located all over Finland and they do not have uniform criteria for ICU admissions or ICU discharges. In addition, in the database available for us, we did not have data of the organization, staffing or, for example, patient to nurse ratios (P/N-ratio) for the individual ICUs. However, from half of the ICUs we were able to get their P/N-ratios for the different time periods that were studied. The mean P/N-ratio (calculated from the average values for the whole 24-h day) in these ICUs was 1.1 both in weekdays and weekends. During “office-hours” (0800–1600) the mean P/N-ratio was 0.9 and during “out-of-office hours” it was 1.2. In these same ICUs the mean number of beds was 12 (range 8–23) and the mean bed/senior physician ratio was 7.8. (range 5–10). All ICUs included in this study were run by an anesthesiologist and most of the ICUs were closed units. Only one of the ICUs included had a dedicated back-up for intensivist consultation 24 h a day, 7 days a week. In all ICUs, during evenings and nights, physicians on-call may not directly belong to the ICU staff. In most of the ICUs included in this study there is only one physician on-call and he/she has also other responsibilities because he/she is simultaneously on-call also for the operating theatre. From the database we selected all 23,134 patients who had undergone emergency admissions. Emergency admissions were studied because these patients are more likely to have complex disorders with higher associated mortality than elective admissions. A previous study suggested that the effect of admission time on mortality would be most prominent in these patients [1]. The main reasons for ICU admission were classified into pre-specified diagnostic groups. We categorized all patients according to whether they were admitted to or discharged from ICU during weekend or weekday and during “office hours” or “out-of-office” hours. In addition, the time of death in the ICU was recorded accordingly. Weekend was defined as a time period from 1600 hours Friday to 2400 hours Sunday. All other times were considered weekdays. “Office hours” were defined as a time period from 0800 hours to 1600 hours. All other hours were defined as “out of office” hours. Accordingly, some patients were categorized to the group “office hours”, but at the same time to the group “weekend”. Overall, the definitions for weekend and “office hours” using a 24-h clock may be problematic, especially in the ICU setting. However, for the purpose of this investigation some categorization of different time periods was mandatory, and therefore to allow better comparison of our results with existing literature we chose to use these categories because they were used in two previous studies on the same topic [1, 7].
We used Simplified Acute Physiology-II (SAPS II) - scores to assess disease severity [8]. We also assessed the intensity of care the patients received while being treated in the ICU. The Therapeutic Intervention Scoring System (TISS) was used for this purpose. This scoring system was originally developed in 1974 to measure the amount of nursing work required by each critically ill patient and it was updated later [9, 10]. TISS consists of 76 therapeutic and monitoring tasks which are weighted from 1 to 4. The weights are based on the relative intensity of nursing and physician efforts to perform these tasks. Thus, the sum TISS-score increases with increasing intensity in patient care. To take into account the differences in ICU length of stay, we calculated mean TISS-scores (total TISS-score gained during the whole ICU-stay divided by the number of days spent in the ICU) for each patient. Sometimes restrictions for future care (= decisions to withhold or withdraw care) may be set for critically ill patients due to poor prognosis. It is possible that these patients are discharged to the wards particularly after afternoon rounds after 1600 hours and thus the analysis of the effect of discharge time on mortality may be confounded. In the database we had a code on whether care was restricted in the future. We used this code to adjust for the effect of care restrictions on mortality.
Statistical methods
We first did a crude analysis in 23,134 patients, comparing mortality between patients who were admitted to ICU during weekend or weekday and during office hours or “out-of-office” hours. A t-test was used to compare potential explanatory variables between survivors and non-survivors. We then applied logistic regression analysis using the data of 15,978 patients (for whom we had complete data of potential explanatory variables) to test the effect of different admission times on ICU-mortality adjusted for SAPS II-, and mean TISS-scores and whether restrictions were set for future care. With this logistic regression analysis we were also able to study the associations between the risk and the time of death (weekend, weekday, “out-of-office” hour, “office hours”) in the ICU. We used forward likelihood ratio procedure in logistic regression. A probability of 0.05 was used to enter a variable into the model and a probability of 0.1 to remove a variable from the model. In the first analyses we included all patients. In the next analyses, including a separate logistic regression analysis, we studied only ICU survivors to assess the effect of ICU discharge time on hospital mortality. In all logistic regression analyses we adjusted for time (weekend, weekday, “out-of-office hour”, “office-hour”), SAPS II-scores, mean TISS-scores, and whether restrictions were set for future care. Differences in crude mortality rates are expressed as percentages, whereas adjusted mortality rates are presented as odds ratios and 95% confidence intervals. A P-value of <0.05 was used to indicate statistical significance. All P-values are two-sided. Analyses were performed by using SPSS for Windows, version 9.0 (SPSS, Chicago, Ill., USA).
Results
The main underlying reasons or organ system dysfunction causing the need for intensive care are presented in Table 1. Acute circulatory and respiratory failure were the most common reasons for ICU admission. The majority, 18,457 patients, were admitted on weekdays and 14,580 patients on “out-of-office” hours (Table 2). In addition, among patients who survived ICU, 17,691 patients were discharged on weekdays and 16,952 patients in “office hours” (Table 2).
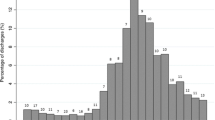
Overall hospital mortality was 20.7%. The mean SAPS II for the entire population was 34±17 (mean±SD). As expected, those who died had higher SAPS II-scores as compared with survivors (52±19 vs 29±14, P<0.001). Non-survivors also had higher mean daily TISS-score, indicating more intense care, as compared with survivors (28±10 vs 20±9, P<0.001). ICU-mortality for all patients was 10.9%. Unadjusted mortality was not different for patients who were admitted on weekends as compared with patients who were admitted on weekdays (Table 3). However, when confounders were considered in logistic regression analysis, weekend admission was associated with increased risk of death [odds ratio 1.20 (1.01–1.43, 95% CI), P=0.036]. Unadjusted ICU-mortality was lower for patients who were admitted during “out-of-office” hours as compared with “office hour” admissions. However, adjusted analysis showed that “out-of-office” hour admission was not associated with lower risk of death (Table 3). When considering the time of death, logistic regression analysis showed that patients who did not survive ICU were more likely to die during evenings and nighttime as compared with daytime [odds ratio 6.89 (5.96–7.96), P< 0.001]. However, there were no differences in this respect when we compared weekdays with weekends. If restrictions for care were set, this was associated with increased risk of death [7.73 (6.58–9.09), P< 0.001] as compared with patients in whom care was not restricted.
Hospital mortality for ICU-survivors (20,636 patients) was 11.5% for patients who were discharged from ICU during evenings and nighttime as compared to 9.8% mortality for patients who were discharged during daytime, P=0.002. However, in the logistic regression analysis (14,308 patients) this difference disappeared (odds ratio for death associated with “out-of-office” hour discharge 1.11, 0.93–1.31, P=0.24). Hospital mortality for ICU-survivors was 9.2% for patients who were discharged during weekends as compared with 10.2% mortality for patients who were discharged in weekdays, P=0.09. No significant differences were found in the adjusted analysis (odds ratio for death associated with weekend discharges was 0.88, 0.73–1.07). If restrictions for future care were set after ICU discharge, this was associated higher odds for death [8.8 (7.04–10.4), P< 0.001] as compared with patients in whom future care was not restricted.
Discussion
We found that weekend ICU admissions are associated with increased ICU mortality (by 20%) in critically ill patients. However, admissions in the evenings and during nighttime were not associated with increased risk of death. Strikingly, the risk of dying in the ICU was higher during “out-of-office” hours as compared with office hours. Our findings were not explained by disease severity, intensity of care given to patients in ICU or by decisions to restrict patient’s care. Finally, when the patients were discharged from the ICU, their risk of hospital death was not associated with the timing of discharge.
Our finding of increased mortality in patients who are admitted to ICU during weekend as compared with weekdays is in agreement with a recent study in acutely ill patients [1]. Patients solely in critical care units were excluded in this prior study, but the authors speculated that the effect of weekend admissions on mortality would be most important in patients with complex disorders with high mortality rates. Critically ill patients typically have complex problems with high associated mortality rates. However, the magnitude of increased mortality for weekend ICU admissions in our study was in the same range, and at least not higher, as it was for acutely ill patients in the study by Bell and Redelmeier [1]. One reason for increased mortality for weekend admissions in our study could be that only one of the ICUs which were included in this analysis, had 24-h intensivist coverage, 7 days a week. Hence, most of the ICUs in our study lacked a dedicated full-time intensivist coverage for the whole time-period from Friday afternoon till Monday morning. The lack of this coverage was recently shown to increase mortality in critically ill patients [6].
On the other hand, we found that mortality was not increased for patients who were admitted to ICU from 1600 hours to 0800 hours. We can only speculate about the potential explanations for this finding. In the ICUs that were included in our study, the physician on-call in hospital for critically ill patients most often does not work on a daily basis in the ICU during normal working hours. Therefore, the physician on-call does not necessarily have in-depth knowledge of the patients who already are in the ICU at the start of her/his shift (1600 hours). New admissions by this physician occur from 1600 hours to 0800 hours and therefore she or he has to know new patients in detail to make plans for examinations and therapeutic interventions. It may be that during the evenings and nighttime the physician is more informed of and involved with newly admitted patients and thus more dedicated to their care. This could translate into equal mortality for “our-of-office” hour and “office hour” admissions.
We also studied the time of death for patients who died in the ICU. To our surprise we found that the risk of death in the ICU was almost sevenfold in evenings and during nighttime as compared with daytime. This was not explained by disease severity, intensity of care given, and potentially set restrictions for care for desperately ill patients. One natural explanation for our finding is that evening and nighttime in our study covered 2/3 of the day, as normal working hours were defined as from 0800 hours to 1600 hours. If ICU-deaths were equally “spread” around the 24-h clock, then the risk of death during “out-of-office” hours would be expected to be approximately double as compared with the risk of death during daytime. One potential explanation for our finding could be that in the database we used, restrictions for care were not correctly classified. Thus, it could be that patients died during nighttime as a consequence of a decision (made during daytime) to withdraw or withhold care, but this was not correctly indicated in the database. However, there was evidence in our study that care restrictions were recorded at least reasonably well. We can only speculate regarding why the risk of death was increased in evenings and during nighttime, and one potential reason could be the lack of dedicated full-time intensivists in the ICUs at this time of day. We do not have detailed data for all ICUs on whether potential differences in staff workload during nighttime vs daytime could also contribute [5].
We did not find an association between the time of discharge from the ICU and further hospital mortality. This in contrast to the findings of Goldfrad and Rowan who showed that the odds ratio for hospital death for ICU survivors was 1.33 (1.06–1.65) for patients who were discharged at night (2200 – 0700) [7]. In our study, the risk of death for ICU survivors who were discharged in evenings and during nighttime was not significantly increased (1.1, 95% CI 0.93–1.3). The reasons for the discrepancy between the findings in these two studies are not obvious. Goldfrad and Rowan adjusted for case-mix by using APACHE II scoring only. In our analysis using logistic regression model, we took into account disease severity (SAPS II-scores), but also intensity of care, and whether restrictions for care were applied. In addition we included patients who were discharged from 1600 hours to 0800 hours to the group “out-of-office” hour discharges, whereas Goldfrad and Rowan included patients who were discharged from 2200 hours to 0700 hours.
We used a large database of prospectively collected data in our analysis. ICUs which were included in our study, cover approximately 80% of all ICUs that treat adult patients in Finland and our included patients represent diverse medical and surgical specialties. Unfortunately, in the database that we used, we did not have data regarding details and organizational characteristics of all different ICUs that were included in our study. For example, we cannot give detailed data of the number of different kind of physicians working in the ICUs or patient to nurse ratios in all individual ICUs. In addition, we are not able to provide data of the organizational aspects in all individual ICUs, particularly during evenings and nighttime and during weekends. Therefore, we do not know to what extent our findings are generalizable to other countries and settings but they are likely to be generalizable to our country. However, there still may be some other limitations to our study. Some of our patients were categorized as being admitted to or discharged from ICU during office hours but during weekend. We acknowledge this potential discrepancy, but we chose to use these categories to better allow comparison between our study and other investigations on the same topic [1, 7]. Further, misclassification of patients to those who had or did not have restrictions for future care could have happened, but we do not believe that this could totally explain our findings. There could also be other factors that we did not recognize. Finally, in our study ICU mortality was 10.9%, but the overall hospital mortality was 20.7%, and thus the post-ICU-mortality was relatively high. Unfortunately, given the stated aim of our study and the data that were available for us in the database, we cannot say or even speculate about what could be the reasons for this.
In conclusion, we found that weekend admissions, as compared with weekday admissions, are associated with increased mortality in critically ill patients. In the ICU, the risk of dying is higher in evenings and during nighttime as compared with daytime. When patients are discharged from the ICU, their risk of hospital death is not associated with the timing of discharge. If our findings can be confirmed elsewhere, they may have important implications for organization of ICU services.
References
Bell CM, Redelmeir DA (2001) Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 345:663–668
Provonost PJ, Jenckes MW, Dorman T, Garret E, Breslow MJ, Rosenfeld BA, Lipsett PA, Bass E (1999) Organizational characteristics of intensive care units related to outcomes of abdominal surgery. JAMA 281:1310–1307
Reynolds HN, Haupt MT, Thill-Baharozian MC, Carlson RW (1988) Impact of critical care physician staffing on patients with septic shock in a university hospital medical intensive care unit. JAMA 260:3446–3450
Multz AS, Chaflin DB, Samson IM, Danztker DR, Fein AM, Steinberg HN, Niederman MS, Scharf SM (1998) A “closed” medical intensive care unit (MICU) improves resource utilization when compared with an “open” MICU. Am J Respir Crit Care Med 157:1468–1473
Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ (2000) Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet 356:185–189
Blunt MC, Burchett KR (2000) Out-of-hours consultant cover and case-mix-adjusted mortality in intensive care. Lancet 356:735–736
Goldfrad C, Rowan K (2000) Consequences of discharges from intensive care at night. Lancet 355:1138–1142
Le Gall JR, Lemeshow S, Saulnier F (1994) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study [published erratum appears in JAMA 1994 271(17):1321]. JAMA 270:2957–2963
Cullen DJ, Civetta JM, Briggs BA, Ferrara LC (1974) Therapeutic intervention scoring system: a method for quantitative comparison of patients care. Crit Care Med 2:57–60
Keene AR, Cullen DJ (1983) Therapeutic scoring system: update 1983. Crit Care Med 11:1–3
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uusaro, A., Kari, A. & Ruokonen, E. The effects of ICU admission and discharge times on mortality in Finland. Intensive Care Med 29, 2144–2148 (2003). https://doi.org/10.1007/s00134-003-2035-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2035-1