Abstract
Purpose
Indigenous people have high rates of suicide and self-harm compared to other population groups.
Aim
The aim of this trial was to see if a package of interventions delivered in a culturally appropriate way improved outcomes at one year in Maori who presented with intentional self-harm to emergency departments.
Methods
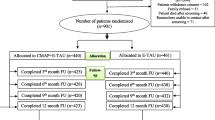
Participants were Maori who presented with intentional self-harm to emergency departments in New Zealand. The study design was a double consent Zelen randomised controlled trial. The intervention included regular postcards, problem solving therapy, patient support, risk management, improved access to primary care and cultural assessment in addition to usual care. The control group received usual care. The main outcome measure was the self-rated change in scores on the Beck Hopelessness Scale at one year.
Results
182 people were randomized to the intervention group 95 of whom consented to take part in the study. 183 people were randomized to the control group 72 of whom consented to take part in the study. For those who consented comparing the intervention group with the control group there was a statistically significant greater change in hopelessness scores at 3 months (difference −1.7 95 % CI −3.4 to −0.01, p = 0.05) but not at one year (difference −1.6 95 % CI −3.4 to 0.3, p = 0.11). Maori who consented and received the intervention were also significantly less likely to present to hospital for non-self-harm reasons in the year after the index episode (44.2 vs. 61.1 %, p = 0.03). Those participants randomised to the intervention were less likely to re-present with self-harm at 3 months (10.4 vs. 18 %, p = 0.04) but not at 12 months compared to the control group.
Conclusions
In Maori who presented to hospital with intentional self-harm a culturally informed intervention had an effect on hopelessness and re-presentation with self-harm in the short term but not at 12 months. There was a significant decrease in hospital presentations for non-self harm over the next year.
Trial registration
Australian and New Zealand Clinical Trials Registry ACTRN12609000952246.

Similar content being viewed by others
References
Statistics Canada (2012) Mortality rates among children and teenagers living in Inuit Nunangat, 1994 to 2008. http://www.statcan.gc.ca/pub/82-003-x/2012003/article/11695-eng.htm
Australian Government Department of Health (2013) National Aboriginal and Torres Strait Islander Suicide Prevention Strategy. http://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-natsisps-strat-toc~mental-natsisps-strat-1~mental-natsisps-strat-1-ab
National Institute for Health and Clinical Excellence (2011) Longer-term care and treatment of self-harm. vol CG133
Hatcher S, Sharon C, Parag V, Collins N (2011) Problem solving therapy for people who present to hospital with self-harm: zelen randomised controlled trial. Br J Psychiatry 199:310–316
Beautrais AL, Wells JE, McGee MA, Oakley Browne MA (2006) Suicidal behaviour in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry 40(10):896–904
Ministry of Health (2014) Suicide facts: deaths and intentional self-harm hospitalisations 2011. Wellington
Coupe N, Hatcher S (2007) Whakamomori: maori deliberate self-harm presentations to three Auckland public hospitals. He Pukenga Korero 8(2):5–9
Hatcher S, Coupe N, Durie M, Elder H, Tapsell R, Wikiriwhi K, Parag V (2011) Te Ira Tangata: a Zelen randomised controlled trial of a treatment package including problem solving therapy compared to treatment as usual in Maori who present to hospital after self harm. Trials. doi:10.1186/1745-6215-12-117
Hatcher S, Sharon C, Coggan C (2009) Beyond randomized controlled trials in attempted suicide research. Suicide Life Threat Behav 39(4):396–407
Hawton K, Bergen H, Casey D, Simkin S, Palmer B, Cooper J, Kapur N, Horrocks J, House A, Lilley R, Noble R, Owens D (2007) Self-harm in England: a tale of three cities. Multicentre study of self-harm. Soc Psychiatry Psychiatr Epidemiol 42(7):513–521
Beck AT, Weissman A, Lester D, Trexler L (1974) The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol 42(6):861–865
Zigmond A, Snaith R (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Beck AT, Kovacs M, Weissman A (1979) Assessment of suicide intention: the scale for suicide ideation. J Consult Clin Psychol 47:343–352
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Hagerty BM, Patusky K (1995) Developing a measure of sense of belonging. Nurs Res 44(1):9–13
Phinney JS (1992) The multigroup ethnic identity measure. J Adolesc Res 7(2):156–176
Durie MH, Black TE, Christensen IS, Durie AE, Fitzgerald ED, Taiapa JT (1995) Te Hoe Nuku Roa framework: A Maori identity measure. Journal of Polynesian Society 104 (4)
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, Moore L, O’Cathain A, Tinati T, Wight D, Baird J (2015) Process evaluation of complex interventions: medical research council guidance. BMJ. doi:10.1136/bmj.h1258
Acknowledgments
We would like to thank Rees Tapsell and Hinemoa Elder for their support and encouragement in the early stages of this project. We would also like to extend our thanks to the Maori advisory board who offered wise advice throughout the trial. Kapai.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Hatcher, S., Coupe, N., Wikiriwhi, K. et al. Te Ira Tangata: a Zelen randomised controlled trial of a culturally informed treatment compared to treatment as usual in Māori who present to hospital after self-harm. Soc Psychiatry Psychiatr Epidemiol 51, 885–894 (2016). https://doi.org/10.1007/s00127-016-1194-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-016-1194-7