Abstract
Purpose
Care provided in the community for dementia patients on an individual basis may be very time consuming. Yet, little is known about the factors affecting caregiving time for community-dwelling dementia patients. Thus, we aimed to investigate the predictors of informal and formal caregiving time for these patients in a longitudinal approach.
Method
Caregiving time for n = 126 community-dwelling dementia patients was assessed by proxy interviews in four assessments at 6-month intervals (1.5 years of longitudinal follow-up; AgeCoDe study). Measurement of informal caregiving time was based on a German adaptation of the Resource Utilization in Dementia questionnaire. Dementia severity was measured by the Clinical Dementia Rating (CDR). We used random effects models to estimate the effects of sociodemographic variables (age, gender, marital status and education), comorbidity and dementia severity on informal and formal caregiving time.
Results
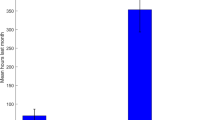
At the first assessment, mean age was 85.0 years (±3.2 years). The majority of patients was female (65.9 %), not married (divorced, single, widowed: 55.6 %) and had primary education (63.5 %). Furthermore, mean GDS was 4.4 (±0.8) and mean MMSE was 20.1 (±5.1). According to CDR, 43 individuals had very mild dementia, 55 individuals had mild dementia and 28 individuals had moderate/severe dementia. Moreover, mean total caregiving time was 3.4 h per day (±4.0). Thereof the main part represents informal caregiving time (2.3 h ± 3.4), whereas formal caregiving time was 1.2 h (±2.4). Dementia severity was associated with total caregiving time, mainly influenced by informal caregiving time. Age was positively associated with total caregiving time, driven by formal caregiving time, while being married was positively associated with total caregiving time, mainly affected by informal caregiving time. All need categories of informal caregiving time were strongly related to dementia severity, whereas none of the categories of formal caregiving time were related to dementia severity.
Conclusions
Our findings extend previous studies that found an association between informal caregiving time and dementia severity. Moreover, our findings highlight the role of informal care for community-dwelling dementia patients in Germany. Informal caregiving time strongly increases with dementia severity. Consequently, as the number of patients suffering from dementia is expected to increase considerably in the next decades, there is a paramount need to strengthen the informal care system to meet patients’ needs.
Similar content being viewed by others
References
Bickel H (2005) Epidemiologie und Gesundheitsökonomie [Epidemiology and Health Economics]. Thieme Verlag, Stuttgart, pp 1–15
Goldsmith M (1996) Hearing the voice of people with dementia: opportunities and obstacles. Readers Digest
Wiles JL, Leibing A, Guberman N et al (2012) (52) The meaning of “aging in place” to older people. Gerontologist 3:357–366. doi:10.1093/geront/gnr098
Federal Ministry of Justice (1994) Social code book XI. Federal Ministry of Justice, Berlin
Jakobsen M, Poulsen PB, Reiche T et al (2011) Costs of informal care for people suffering from dementia: evidence from a Danish survey. Dement Geriatr Cogn Disord Extra 1(1):418–428
Bakker C, de Vugt Marjolein E, van Vliet D et al (2013) The use of formal and informal care in early onset dementia: results from the NeedYD study. Am J Geriatr Psychiatry 21(1):37–45
Zhu CW, Scarmeas N, Torgan R et al (2006) Clinical characteristics and longitudinal changes of informal cost of Alzheimer’s disease in the community. J Am Geriatr Soc 54(10):1596–1602
Leicht H, König H, Stuhldreher N et al (2013) Predictors of costs in dementia in a longitudinal perspective. PLoS One 8(7):e70018
Zhu CW, Leibman C, McLaughlin T et al (2008) Patient dependence and longitudinal changes in costs of care in Alzheimer’s disease. Dement Geriatr Cogn Disord Extra 26(5):416–423
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Blessed G, Tomlinson BE, Roth M (1968) The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry 114(512):797–811
Luck T, Riedel-Heller SG, Luppa M et al (2010) Risk factors for incident mild cognitive impairment—results from the German Study on Ageing, Cognition and Dementia in Primary Care Patients (AgeCoDe). Acta Psychiatr Scand 121(4):260–272
Zaudig M, Mittelhammer J, Hiller W et al (1991) SIDAM: a structured interview for the diagnosis of dementia of the Alzheimer type, multi-infarct dementia and dementias of other aetiology according to ICD-10 and DSM-III-R. Psychol Med 21(01):225–236
Morris JC (1993) The clinical dementia rating (CDR): current version and scoring rules. Neurology 43(11):2412–2414
Reisberg B, Ferris SH, de Leon Mony J et al (1982) The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry 139(9):1136–1139
Mahoney FI (1965) Functional evaluation: the Barthel index. Maryland State Med J 14:61–65
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9(3 Part 1):179–186
Morris JC (1997) Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr 9(S1):173–176
Rikkert MG, Tona KD, Janssen L et al (2011) Validity, reliability, and feasibility of clinical staging scales in dementia: a systematic review. Am J Alzheimer’s Dis Other Dement 26(5):357
Foster JR, Sclan S, Welkowitz J et al (1988) Psychiatric assessment in medical long-term care facilities: reliability of commonly used rating scales. Int J Geriatr Psychiatry 3(3):229–233
Hartmaier SL, Sloane PD, Guess HA et al (1994) The MDS Cognition Scale: a valid instrument for identifying and staging nursing home residents with dementia using the minimum data set. J Am Geriatr Soc 42(11):1173–1179
Neubauer S, Holle R, Menn P et al (2009) A valid instrument for measuring informal care time for people with dementia. Int J Geriatr Psychiatry 24(3):275–282
Wimo A, Nordberg G (2007) Validity and reliability of assessments of time: comparisons of direct observations and estimates of time by the use of the resource utilization in dementia (RUD)-instrument. Arch Gerontol Geriatr 44(1):71–81
Wimo A, Jonsson L, Zbrozek A (2010) The Resource Utilization in Dementia (RUD) instrument is valid for assessing informal care time in community-living patients with dementia. J Nutr Health Aging 14(8):685–690
Cameron AC, Trivedi PK (2005) Microeconometrics: methods and applications. Cambridge University Press, New York
Rothgang H, Müller R, Unger R (2013) Schwerpunktthema: Reha bei Pflege [Barmer GEK Care report 2013]. Asgard-Verl.-Service, Siegburg
Elwert F, Winship C (2014) Endogenous selection bias: the problem of conditioning on a collider variable. Annu Rev Sociol 40:31–53
Statistisches Bundesamt [Federal Statistical Office] (2009) Bevölkerung Deutschlands bis 2060. 12. koordinierte Bevölkerungsvorausberechnung [Germany’s Population by 2060. Results of the 12th Coordinated Population Projection]
Statistisches Bundesamt [Federal Statistical Office] (2011) Bevölkerung und Erwerbstätigkeit. Entwicklung der Privathaushalte bis 2030. Ergebnisse der Haushaltsvorausberechnung [Population and employment. Development of private households until 2030. Results of household projections]
Acknowledgments
The authors thank two anonymous reviewers who provided insightful comments to strengthen the manuscript. Moreover, we want to thank all participating patients and their general practitioners for their good collaboration. This publication is part of the German Research Network on Dementia (KND), the German Research Network on Degenerative Dementia (KNDD), and the Study on Needs, Health Service Use, Costs and Health-related Quality of Life in a large Sample of Oldest-old Primary Care Patients (85+) (AgeQualiDe) and was funded by the German Federal Ministry of Education and Research (Grants KND 01GI0102, 01GI0420, 01GI0422, 01GI0423, 01GI0429, 01GI0431, 01GI0433 and 01GI0434; Grants KNDD 01GI0710, 01GI0711, 01GI0712, 01GI0713, 01GI0714, 01GI0715, 01GI0716 and 01ET1006B; and Grants AgeQualiDe 01GY1322A, 01GY1322B, 01GY1322C, 01GY1322D, 01GY1322E, 01GY1322F, 01GY1322G).
Members of the AgeCoDe Study Group
Principal Investigators [Hendrik van den Bussche (2002–2011)]: Wolfgang Maier, Martin Scherer.
Heinz-Harald Abholz, Cadja Bachmann, Horst Bickel, Wolfgang Blank, Hendrik van den Bussche, Sandra Eifflaender-Gorfer, Marion Eisele, Annette Ernst, Angela Fuchs, Kathrin Heser, Frank Jessen, Hanna Kaduszkiewicz, Teresa Kaufeler, Mirjam Köhler, Hans-Helmut König, Alexander Koppara, Carolin Lange, Hanna Leicht, Tobias Luck, Melanie Luppa, Manfred Mayer, Edelgard Mösch, Julia Olbrich, Michael Pentzek, Jana Prokein, Anna Schumacher, Steffi Riedel-Heller, Janine Stein, Susanne Steinmann, Franziska Tebarth, Michael Wagner, Klaus Weckbecker, Dagmar Weeg, Jochen Werle, Siegfried Weyerer, Birgitt Wiese, Steffen Wolfsgruber, Thomas Zimmermann.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethical statement
The ethics committees of the participating centers approved the study [reference numbers: 050/02 (University of Bonn), 2079 (Faculty of Medicine, University of Düsseldorf), 2817/2007 (Hamburg Medical Association), 309/2007 (Faculty of Medicine, University of Leipzig), 2007-253E-MA (Medical Ethics Commission II, University of Heidelberg at the University Medical Center of Mannheim), 713/02 (Faculty of Medicine, Technical University of Munich)]. The study was conducted according to the principles expressed in the Declaration of Helsinki. All participants gave written informed consent prior to study entry.
Additional information
For the AgeCoDe Study Group.
Rights and permissions
About this article
Cite this article
Hajek, A., Brettschneider, C., Ernst, A. et al. Longitudinal predictors of informal and formal caregiving time in community-dwelling dementia patients. Soc Psychiatry Psychiatr Epidemiol 51, 607–616 (2016). https://doi.org/10.1007/s00127-015-1138-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-015-1138-7