Abstract
Aims/hypothesis
We investigated whether objectively measured sedentary time and interruptions in sedentary time are associated with metabolic factors in people with type 2 diabetes.
Methods
We studied 528 adults (30–80 years) with newly diagnosed type 2 diabetes, who were participants in a diet and physical activity intervention. Waist circumference (WC), fasting HDL-cholesterol, insulin and glucose levels, HOMA of insulin resistance (HOMA-IR) and physical activity (accelerometer) were measured at baseline and at 6 months follow-up. Linear regression models were used to investigate cross-sectional and longitudinal associations of accelerometer-derived sedentary time and breaks in sedentary time (BST) with metabolic variables.
Results
In cross-sectional analyses each hour of sedentary time was associated with larger WC (unstandardised regression coefficient [B] [95% CI] 1.89 cm [0.94, 2.83]; p < 0.001), higher insulin (B = 8.22 pmol/l [2.80, 13.65]; p = 0.003) and HOMA-IR (B = 0.42 [0.14, 0.70]; p = 0.004), and lower HDL-cholesterol (B = −0.04 mmol/l [−0.06, −0.01]; p = 0.005). Adjustment for WC attenuated all associations. Each BST was associated with lower WC (B = −0.15 cm [− 0.24, −0.05]; p = 0.003) and there was evidence of a weak linear association with HDL-cholesterol, but no association with insulin levels or HOMA-IR. Volume of sedentary time at baseline predicted HDL-cholesterol (B = −0.05 mmol/l [−0.08, −0.01]; p = 0.007), insulin levels (B = 8.14 pmol/l [0.1.51, 14.78]; p = 0.016) and HOMA-IR (B = 0.49 [0.08, 0.90]; p = 0.020) at 6 months, though not WC. Baseline BST did not substantially predict any metabolic variables at follow-up. No change was seen in sedentary time or BST between baseline and 6 months follow-up.
Conclusions/interpretation
Higher sedentary time is associated with a poorer metabolic profile in people with type 2 diabetes.
Similar content being viewed by others
Introduction
Physical activity is considered to be central to the prevention and management of type 2 diabetes because of its potential to improve glycaemic control, lipid profile and blood pressure, and (in combination with dietary change) to aid weight loss and maintenance [1]. In the general population, exercise reduces the risk of developing diabetes by 33% to 50%; and, indeed, several major trials have shown that lifestyle changes focusing on improved diet and increased physical activity are able to delay or possibly prevent the development of type 2 diabetes in participants with impaired glucose tolerance [1, 2]. In people who have type 2 diabetes, meta-analyses have shown that structured aerobic exercise, resistance training and both in combination reduce HbA1c by approximately 0.7% (−15.8 mmol/mol) [3, 4]. The effect of physical activity advice (in contrast to structured training) is less clear, but recent studies have suggested that physical activity advice in the absence of dietary intervention may be insufficient to substantially lower HbA1c [4–6].
Despite the potential health benefits, people with diabetes generally record low levels of physical activity and fewer meet physical activity recommendations (aerobic exercise of at least moderate intensity on five or more weekdays,) than in the general population [1, 7–9]. In the 2003 Behavioural Risk Factor Surveillance Survey only 23% to 37% of people with diabetes met activity guidelines [7] and participants in the Look AHEAD Study recorded less than one bout of moderate to vigorous physical activity (MVPA) per day [8]. These relatively low levels of physical activity and the apparent difficulty of increasing and maintaining higher physical activity in people with diabetes suggest that alternative lifestyle strategies for improving metabolic health may be required.
Recent interest has focussed on the potential role of sedentary behaviour in the development of chronic disease [10, 11]. People spend a large proportion of their day in sedentary pursuits such as using a computer, watching TV or sitting in a car. Data from the 2003–2004 National Health and Nutrition Examination Survey (NHANES) found that participants spent 7.7 h per day (54.9% of waking time) in sedentary behaviours, with sedentary time increasing by about 2 h per day between the ages of 30 to 39 and 70 to 85 years [12]. Evidence is accumulating that the cellular and molecular responses to inactivity are different from the beneficial responses to physical activity, and that sedentary behaviour may be an important factor in determining metabolic health independently of levels of physical activity [10, 11, 13]. Recent observational studies have described a substantial health risk associated with sedentary behaviours. Time spent watching TV or using a computer has been associated with greater clustered metabolic risk [14] and increased risk of cardiovascular disease, type 2 diabetes, and all-cause and CVD death [15–17]; moreover, in longitudinal studies a dose–response relationship has been described between sitting time and all-cause and CVD mortality rates [18].
In contrast to relatively imprecise self-report of sedentary behaviours such as sitting or TV watching, accelerometers are increasingly being used to provide an objective measurement of time spent doing sedentary activities. A recent analysis of data from the 2003/2004 and 2005/2006 NHANES surveys showed that higher levels of objectively measured sedentary time is associated with greater waist circumference (WC), elevated C-reactive protein, triacylglycerol and insulin levels, insulin resistance and lower HDL-cholesterol independently of potential confounders including MVPA [19]. Indeed, similar findings have been reported from other studies in the UK and Australia [20, 21]. However, these associations are not consistently reported, with other studies finding no relationship between objectively measured sedentary time and insulin resistance or 2 h glucose [22, 23]. Emerging evidence suggests that not only the volume of sedentary time, but also the pattern of sedentary time may be independently associated with health outcomes. The frequency with which sedentary time is interrupted by non-sedentary behaviour (breaks) has been associated with lower WC, BMI, 2 h plasma glucose and C-reactive protein levels [19, 24].
There is a growing consensus that sedentary behaviour represents a unique aspect of human behaviour and is not synonymous with the absence of physical activity [13]. To date, no studies have investigated the association between sedentary time and metabolic outcomes in people with type 2 diabetes. Given the low levels of physical activity in people with type 2 diabetes, targeting reductions in sedentary behaviour could be an alternative approach to disease management. However, before such interventions are developed, it is important to clarify the association between sedentary time and metabolic outcomes in people with type 2 diabetes. The aim of the present study was therefore to investigate the association between sedentary time, breaks in sedentary time (BST) and selected metabolic factors in a population of people with newly diagnosed type 2 diabetes.
Methods
Participants
This was a secondary analysis of data from participants in Early Activity in Diabetes (Early-ACTID), a randomised controlled trial of diet and physical activity early in the management of type 2 diabetes [5]. Participants were recruited from 217 general practices in the South West of England between December 2005 and September 2008. They were identified by practice database searches, from community-based education programmes and by direct advertising. Individuals were eligible for inclusion if aged 30 to 80 years and with a clinical diagnosis of type 2 diabetes within the previous 6 months. Exclusion criteria included uncontrolled diabetes (HbA1c >10% [85.8 mmol/mol]), blood pressure >180/100 mmHg, LDL-cholesterol >4 mmol/l, and BMI <25 kg/m2 or body weight >180 kg. Of 1,634 patients initially screened by telephone, 712 were eligible for face-to-face screening and 593 were enrolled in the study. Ethical approval was obtained from the Bath Hospital Research Ethics Committee and each participant provided written informed consent [5].
Measures
Measures were taken at baseline (5 to 8 months after a clinical diagnosis of type 2 diabetes) and repeated 6 and 12 months later. Baseline and 6 month data were used in the current analysis, since outcomes at 6 months were defined as the primary endpoint of the study [5]. Fasted blood samples were taken for the measurement of HDL-cholesterol, glucose and insulin levels, and HOMA of insulin resistance (HOMA-IR) was calculated using the HOMA-2 computer model [25]. Weight was measured on a digital scale with participants wearing light indoor clothes without shoes, height was measured to the nearest centimetre with shoes off using a freestanding height measure (Seca 220; Hamburg, Germany) and WC was measured at the midpoint between the lowest rib and anterior iliac. Physical activity was measured for 7 days using an accelerometer (GT1M; ActiGraph LLC, Pensacola, FL, USA) worn on a belt around the waist, except when swimming, bathing and sleeping. Smoking habits and family history of diabetes were assessed by a research nurse. The UK Index of Multiple Deprivation (IMD) 2007 score based on full home post-code was used as an indicator of socioeconomic status [26].
Accelerometer data reduction
Accelerometers were set to record data every minute. Raw accelerometer files were processed using KineSoft (version 3.3.62; KineSoft, Saskatoon, SK, Canada). A valid day was defined as recording at least 10 h of measurement, excluding periods of ≥20 min with continuous zero values (considered to be non-wear time). Total physical activity was computed as the mean accelerometer cpm over the full period of valid recording. The average number of min of MVPA and sedentary time per valid day were computed using thresholds of ≥1,952 and <100 cpm respectively for comparison with other studies [19, 24]. Each minute where ≥100 counts were recorded immediately following ≥1 min <100 counts was defined as a BST. For inclusion in analyses, participants were required to record at least three valid days of accelerometer data.
Statistical analysis
Data were treated as a cohort and not analysed by trial arm since the intervention used in the Early-ACTID Study was not designed to influence sedentary behaviour. Descriptive characteristics are summarised as mean and SD, unless otherwise stated. Analysis of variance was used to investigate sex differences in demographic and physical activity variables, and paired samples t tests were used to describe differences in mean values of continuous variables between baseline and 6 months. Linear regression models were first used to investigate the cross-sectional associations of sedentary time and BST with metabolic variables at baseline and 6 months. Bivariate correlations between MVPA, sedentary time and BST at baseline were low (MVPA vs sedentary time, R = −0.20; MVPA vs BST, R = −0.06; sedentary time vs BST, R = 0.13) and were all therefore entered into each model. Models were run for each metabolic variable in turn as the outcome, and with the physical activity variable (sedentary time or BST) under investigation as the exposure. All models were adjusted for age, sex, current smoking (yes/no), family history of diabetes, deprivation score, relevant lipid-lowering or diabetes medication (each dichotomised as medication yes/no), and the remaining physical activity variable (model 1). Next, models were additionally adjusted for WC (model 2). All models were run with and without MVPA to test whether associations were independent of MVPA. Subsequently linear regression was used to investigate whether baseline sedentary time or BST, or change in sedentary time or BST between baseline and 6 months predicted the values of metabolic variables at follow-up. Models were adjusted as before, but also including baseline values of the metabolic variable under investigation. Finally, to explore the direction of association, models were run with sedentary time and BST at 6 months respectively as the outcome, and with baseline WC as the exposure, adjusted for sex, family history of diabetes, deprivation score and baseline values for age, smoking, MVPA, sedentary time and BST.
Results
A total of 593 patients met the Early-ACTID Study criteria. The accelerometer inclusion criteria were met by 528 (89.0%) participants at baseline, with 36.9% recording seven valid days of data, 28.8% 6 days, 15.9% 5 days, 11.0% 4 days and 7.4% 3 days. At 6 months, 411 (69.3%) participants met the accelerometer criteria, with 380 (64.1%) providing valid data at baseline and 6 months. Demographic, metabolic and physical activity characteristics of the baseline sample (n = 528) are shown in Table 1. Participants were predominantly white and from areas of higher deprivation, with a majority (51.8%) being obese. Participants spent 61.5% of the recorded time in sedentary positions and only 3.2% of recorded time in MVPA. Sedentary time was interrupted on average 84 times per day. Men were more physically active than women, recording higher total physical activity and MVPA, but sedentary time did not differ between the sexes. Women recorded more interruptions of sedentary time than men, but when adjusted for volume of sedentary time, breaks per hour were higher in men.
There were no differences in key demographics (age, BMI, WC), in metabolic variables (HDL-cholesterol, insulin, HOMA-IR) or physical activity (cpm, MVPA, sedentary time) between participants included and those not included in the longitudinal sample. Participants in the longitudinal sample recorded slightly more BST than those excluded (85.2 ± 14.4 versus 82.5 ± 13.8 interruptions per day, p = 0.051).
The results of cross-sectional linear regression analyses with sedentary predictor variables in the full baseline sample (n = 528) are shown in Table 2. Higher sedentary time was associated with a larger WC, with an approximately 2 cm greater WC being associated with each extra hour of sedentary time. Higher sedentary time was also associated with lower HDL-cholesterol, and higher insulin and HOMA-IR values, although adjustment for WC attenuated all associations, with 95% CIs including zero for insulin and HOMA-IR. A greater number of BST was associated with lower WC, with each additional break being associated with a 0.15 cm lower WC. Associations with HDL-cholesterol, insulin and HOMA-IR were weak, with 95% CIs including zero. MVPA was inversely associated with WC, with each minute of MVPA being associated with a 0.11 cm lower WC (unstandardised regression coefficient [B] [95% CI] −0.11 [−0.17, −0.06]; p < 0.001). MVPA was also weakly inversely associated with insulin levels (B = −0.55 pmol/l [−0.87, −0.23]; p = 0.001) and HOMA-IR (B = −0.02 [−0.04, −0.01]; p = 0.003), but only in models unadjusted for WC. Associations between MVPA and HDL-cholesterol were extremely small, with 95% CIs including zero. Associations between sedentary variables and all outcomes were unchanged when MVPA was removed from models. There was no association between any sedentary variable or MVPA and glucose.
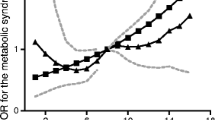
Figure 1 shows the linear associations of quartiles of sedentary time and BST with the metabolic variables. Waist circumference was approximately 6 cm smaller in patients recording the least sedentary time (quartile 1) than in those in the highest quartile (adjusted mean difference [95% CI] 6.5 cm [5.3, 7.6]; p < 0.001), and almost 2 cm smaller in patients in the highest than in those in the lowest quartile of BST (1.9 cm [0.6, 3.1]; p = 0.003). HDL-cholesterol was approximately 7% (0.10 mmol/l [0.07, 0.14]; p < 0.001) lower in patients recording the highest sedentary time (quartile 4) and 4% (0.05 mmol/l [0.02, 0.09]; p = 0.001) higher in those recording the most BST (quartile 4), both relative to the first quartile. Patients in the highest quartile of sedentary time had insulin values 25% greater (28.48 pmol/l [11.70, 45.25]; p < 0.001) than the lowest quartile; similarly HOMA-IR was 26% greater (1.34 [0.88, 1.79]; p < 0.001) in the highest than in the lowest quartile of sedentary time. There was no difference in insulin levels or HOMA-IR across quartiles of BST.
Quartiles of sedentary time and BST. Trends across quartiles of sedentary time and BST for WC (a, b), HDL-cholesterol (c, d), insulin (e, f) and HOMA-IR (g, h). Data are mean values adjusted for age, sex, smoking, family history of diabetes, deprivation score, accelerometer wear time, MVPA, WC, and either BST or sedentary time as appropriate. Quartiles are adjusted for accelerometer wear time. Cut points for quartiles of sedentary time were 437 (7.3 h), 486 (8.1 h) and 529 min (8.8 h) per day; cut points for BST were 74, 84 and 94 breaks per day. n = 528; p < 0.001 for trend (a, c, e, g); p = 0.025 for trend (b); p = 0.005 for trend (d); p = 0.930 for trend (f); p = 0.931 for trend (h)
Changes in metabolic outcomes, physical activity and sedentary variables between baseline and 6 months are shown in Table 3. Mean WC, insulin levels and HOMA-IR values were lower at 6 months than baseline, whereas HDL-cholesterol was higher, although 95% CIs just included the null values. Physical activity was higher at 6 months than baseline, with MVPA increasing from 3.2% to 9.4% of recorded time. However, there was no change in sedentary time, with participants spending 61.7% of their time in sedentary positions at both time points. Similarly, although BST declined between baseline and 6 months, the number of interruptions per h of sedentary time was unchanged.
In the smaller longitudinal sample, cross-sectional associations at baseline were similar to those in the main sample (Table 4). At 6 month follow-up, sedentary time was less strongly associated with WC than at baseline, while associations with HDL-cholesterol were similar. Cross-sectional associations between sedentary time and both insulin levels and HOMA-IR were weaker at 6 months than at baseline, with 95% CIs including zero. In contrast, BST were more strongly associated with WC at 6 months than at baseline.
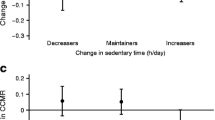
The results of longitudinal regression analyses with sedentary predictors are shown in Table 5. Volume of sedentary time at baseline predicted HDL-cholesterol and insulin levels, and HOMA-IR at 6 months, but not WC. Baseline BST did not substantially predict any metabolic variables at follow-up. When models were run with sedentary time and BST at 6 months as the outcome variables and baseline WC as the exposure, there was very little association between WC and sedentary time (B = 0.09 [−0.50, 0.67]; p = 0.773), but WC was predictive of BST (B = −0.14 [−0.24, −0.03]; p = 0.011), with people with higher baseline WC having fewer BST at 6 months. All associations of change in sedentary time and BST with metabolic variables were weak and 95% CIs included zero (Table 5), possibly due to negligible change in the sedentary variables over this period.
Models were also run to explore the longitudinal associations between MVPA and metabolic outcomes. Baseline MVPA did not predict the level of any metabolic variable at 6 months, while change in MVPA was weakly associated with these variables, with each additional min of MVPA being associated with lower WC (B = −0.02 cm [−0.05, 0.003]; p = 0.089), insulin levels (B = −0.42 pmol/l [−0.70, −0.07]; p = 0.022) and HOMA-IR (B = −0.02 [−0.05, 0.00]; p = 0.019), but not with HDL-cholesterol.
Discussion
This study investigated the cross-sectional and longitudinal associations of objectively measured sedentary time and BST with metabolic variables in a sample of people with newly diagnosed type 2 diabetes. In cross-sectional analyses we found that higher sedentary time was consistently associated with a larger WC and lower HDL-cholesterol, and more weakly associated with higher insulin and HOMA-IR values. In longitudinal analyses the amount of sedentary time at baseline was not associated with WC, but was predictive of HDL-cholesterol and insulin levels, and of HOMA-IR at 6 months. Associations between interruptions of sedentary time and metabolic outcomes were substantially weaker than with sedentary time. More BST were associated with lower WC cross-sectionally, and there was evidence of a linear association between BST and HDL-cholesterol, with more breaks being associated with higher HDL-cholesterol. There was no consistent evidence of association between BST and both insulin or HOMA-IR in cross-sectional models, and BST did not substantially predict any metabolic variables in longitudinal analyses. However, baseline WC was predictive of BST at 6 months. All associations were independent of levels of MVPA. Associations between change in sedentary time or BST and all outcomes were extremely weak.
Participants in the present study had similar levels of physical activity [19, 24, 27] and number of BST [19, 24] to healthy participants in other studies at baseline, despite being older, and having higher BMI and WC, as well as a diagnosis of diabetes. Activity, however, was higher than in a recent study of obese adults [23]. The cross-sectional associations of sedentary time and BST with WC were similar to those reported in other studies [21, 24]. The difference of approximately 6 cm in WC between patients in the high and low quartiles of sedentary time in this study was greater than reported in white participants in NHANES (<4 cm) [19], whereas differences in WC between those in the highest and lowest quartiles of BST (1.9 cm) was lower than in the white participants in NHANES (3.7 cm) and in the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) (5.9 cm) [19, 24]. The association between sedentary time and HDL-cholesterol was larger in this study than in the NHANES population, with differences between the highest and lowest quartiles being almost twice those of the NHANES population, despite the fact that patients with diabetes have lower overall levels of HDL-cholesterol. Inclusion of WC in the models slightly attenuated the association between HDL-cholesterol and sedentary time, but it remained substantial. We found little association between BST and HDL-cholesterol in regression models; this finding was similar to those of the AusDiab Study, where no association was reported [24], although in the current study there was a trend for higher levels of breaks (>84 per day) to be associated with higher HDL-cholesterol. Sedentary time was associated with higher insulin levels and HOMA-IR, with patients in the highest quartile of sedentary time having approximately 25% greater insulin and HOMA-IR values. No association was found between BST and these variables. Although these data are in contrast to several other studies [22, 23, 27] where no association with HOMA-IR was reported, they are broadly consistent with results from the white participants in NHANES [19]. Few other studies have looked at insulin levels to help clarify these observations. An association between sedentary time and 2 h plasma glucose has been reported [28], but in contrast to results from healthy adults, no association was found between sedentary time and insulin resistance in adults with a family history of diabetes [22].
To our knowledge, this is the first study to investigate the longitudinal associations of sedentary time and BST with metabolic outcomes in people with type 2 diabetes. While cross-sectional analyses suggested that a 60 min reduction in sedentary time was associated with an approximately 2 cm smaller WC, the amount of sedentary time at baseline was not predictive of WC at 6 months. The reason for this is unclear, but may result from the diet and physical activity intervention that participants were engaged in and in which WC was reduced and physical activity increased at 6 months. In contrast, the amount of sedentary time at baseline predicted HDL-cholesterol, insulin levels and HOMA-IR at follow-up to a similar magnitude to that seen in the cross-sectional analyses. The number of BST was weakly associated with metabolic outcomes. While each additional BST was associated with an approximately 0.1 cm smaller WC in cross-sectional analyses, there was no association between BST and HDL-cholesterol, insulin or HOMA-IR in cross-sectional or longitudinal analyses. Despite a successful intervention that produced a net increase in physical activity in this sample, there was no concomitant decrease in sedentary time, limiting our ability to investigate whether changes in these behaviours were predictive of changes in the metabolic outcomes.
The present study included a relatively large sample of people with type 2 diabetes who had been recruited to take part in a 52 week, multi-centre parallel-group randomised controlled trial (Early-ACTID) [5]. Patients were randomly assigned to usual care (initial dietary consultation and follow-up every 6 months; control group), or an intensive diet intervention (dietary consultation every 3 months with monthly nurse support) alone or combined with physical activity consultation in a 2:5:5 ratio. Participants in the diet plus exercise arm of the trial received an intervention programme aiming to achieve at least 30 min of brisk walking on at least 5 days per week in addition to current levels of physical activity, with pedometers used to motivate higher physical activity. The intervention increased MVPA by approximately 10 min per day and a reduction in WC was seen in both intervention arms [5]. Despite these changes, mean values of sedentary time and the number of BST were unchanged at 6 month follow-up. Thus it appears that to fully explore longitudinal associations between changes in sedentary time or BST and metabolic outcomes, interventions are required that specifically aim to reduce the amount of time spent sitting and to break up prolonged sedentary time. However, to date there is a lack of evidence of the implementation or effectiveness of such interventions [29].
Nonetheless, these preliminary results suggest that targeting sedentary behaviours, and in particular reducing time spent in sedentary positions, may improve health in people with type 2 diabetes. The findings from the present study may inform lifestyle approaches geared to improving health in people with diabetes, since although HDL-cholesterol may be increased by endurance exercise, there is evidence that these improvements occur only when threshold intensities or duration of exercise are achieved [30]. Such levels may not be feasible for people with diabetes. In common with Early-ACTID, most lifestyle intervention studies in people with impaired glucose tolerance have aimed to achieve 150 min per week of MVPA [31]. However, in interventions where change in physical activity has been reported, participants in the exercise arm increased by substantially less than this, with activity totalling between 60 and 70 min per week [32–35]. Thus it may be unrealistic to expect substantial increases in physical activity in people at risk of or with type 2 diabetes, particularly when it comes to reaching the levels suggested to confer improvements in metabolic outcomes [31]. Targeting sedentary behaviour may help increase HDL-cholesterol independently of levels of physical activity, although the physiological mechanisms remain to be clarified [11, 36].
There are some limitations to the present study. Participants had volunteered to take part in a physical activity and diet intervention study, and may therefore have been more motivated to make changes between the point of diagnosis and measurements, thus not being representative of the general population of patients with newly diagnosed diabetes. It is also likely that many also made substantial lifestyle changes that attenuated the associations studied. Finally, the cross-sectional analyses cannot explore the direction of causation between both sedentary time and BST, and WC. Our preliminary analyses did not find any longitudinal association between WC and sedentary time, and suggest that WC is predictive of BST rather than the other way round. Further intervention studies and longitudinal mediation analyses are required to investigate the direction of association of these variables and the potential mediating role of WC in these associations with metabolic outcomes.
Our data suggest that in overweight/obese people with newly diagnosed type 2 diabetes, interventions to reduce sedentary time and to interrupt sedentary time more frequently should be explored as potential ways to improve metabolic variables, particularly HDL-cholesterol. The development of such interventions could be driven by the incorporation of recommendations for sedentary behaviour into national guidelines.
Abbreviations
- AusDiab:
-
Australian Diabetes, Obesity and Lifestyle Study
- BST:
-
Break(s) in sedentary time
- Early ACTID:
-
Early Activity in Diabetes
- HOMA-IR:
-
HOMA of insulin resistance
- MVPA:
-
Moderate to vigorous physical activity
- NHANES:
-
National Health and Nutrition Examination Survey
- WC:
-
Waist circumference
References
Colberg SR, Sigal RJ, Fernhall B et al (2010) Exercise and type 2 diabetes. The American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care 33:e147–e167
Gill JMR, Cooper AR (2008) Physical activity and prevention of type 2 diabetes. Sports Med 38:807–882
Snowling NJ, Hopkins WG (2006) Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care 29:2518–2527
Umpierre D, Ribeiro PAB, Kramer CK et al (2011) Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes. A systematic review and meta-analysis. JAMA 305:1790–1799
Andrews RA, Cooper AR, Montgomery AA et al (2011) Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. Lancet 378:129–139
Balducci S, Zanuso S, Nicolucci A et al (2010) Effect of an intensive exercise intervention strategy on modifiable cardiovascular risk factors in subjects with type 2 diabetes mellitus. Arch Intern Med 170:1794–1803
Nwasuruba CK, Khan M, Egede LE (2007) Racial/ethnic differences in multiple self-care behaviours in adults with diabetes. J Gen Intern Med 22:115–120
Jakicic JM, Gregg E, Knowler W et al (2010) Activity patterns of obese adults with type 2 diabetes in the Look AHEAD Study. Med Sci Sports Exerc 42:1995–2005
Morrato EH, Hill JO, Wyatt HR, Ghushchyan V, Sullivan PW (2007) Physical activity in U.S. adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care 30:203–209
Owen N, Healy GN, Matthews CE, Dunstan DW (2010) Too much sitting: the population health science of sedentary behaviour. Exerc Sport Sci Rev 38:105–113
Katzmarzyk PT (2010) Physical activity, sedentary behavior, and health: paradigm paralysis or paradigm shift? Diabetes 59:2717–2725
Matthews CE, Chen KY, Freedson PS et al (2008) Amount of time spent in sedentary behaviours in the United States, 2003–2004. Am J Epidemiol 167:875–881
Hamilton MT, Hamilton DG, Zderic W (2007) Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 56:2655–2667
Wijndaele K, Duvigneaud N, Matton L et al (2009) Sedentary behaviour, physical activity and a continuous metabolic syndrome risk score in adults. Eur J Clin Nutr 63:421–429
Wijndaele K, Brage S, Besson H et al (2011) Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk Study. Int J Epidemiol 40:150–159
Dunstan DW, Barr ELM, Healy GN et al (2010) Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Circulation 121:384–391
Grontved A, Hu FB (2011) Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality. A meta-analysis. JAMA 305:2448–2455
Katzmarzyk PT, Church TS, Craig CL, Bouchard C (2009) Sitting time and mortality from all causes, cardiovascular disease and cancer. Med Sci Sports Exerc 41:998–1005
Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N (2011) Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J 32:590–597
Helmerhorst HJF, Wijndaele K, Brage S, Wareham NJ, Ekelund U (2009) Objectively measured sedentary time may predict insulin resistance independent of moderate- and vigorous-intensity physical activity. Diabetes 58:1776–1779
Healy GN, Wijndaele K, Dunstan DW et al (2008) Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care 31:369–371
Ekelund U, Brage S, Griffin SJ, Wareham NJ (2009) Objectively measured moderate- and vigorous-intensity physical activity but not sedentary time predicts insulin resistance in high-risk individuals. Diabetes Care 32:1081–1086
McGuire KA, Ross R (2011) Sedentary behaviour is not associated with cardiometabolic risk in adults with abdominal obesity. PLoS One 6:e20503
Healy GN, Dunstan DW, Salmon J et al (2008) Breaks in sedentary time. Beneficial associations with metabolic risk. Diabetes Care 31:661–666
Levy JC, Matthews DR, Hermans MP (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21:2191–2192
Social Disadvantage Research Centre (2004) The English Indices of Deprivation 2004. Department of Social Policy and Social Research, Communities and Local Government, Oxford, pp 14–42
Balkau B, Mhamdi L, Oppert J-M et al (2008) Physical activity and insulin sensitivity: the RISC Study. Diabetes 57:2613–2618
Healy GN, Dunstan DW, Salmon J et al (2007) Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care 30:1384–1389
Chau JY, van der Ploeg HP, van Uffelen JGZ et al (2010) Are workplace interventions to reduce sitting effective? A systematic review. Prev Med 51:352–356
Rashid S, Genest J (2007) Effect of obesity on high-density lipoprotein metabolism. Obesity 15:2875–2888
Yates T, Khunti K, Bull F, Gorely T, Davies MJ (2007) The role of physical activity in the management of impaired glucose tolerance: a systematic review. Diabetologia 50:1116–1126
Pan X-R, Li GW, Hu YH et al (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. Diabetes Care 20:537–544
Lindstrom J, Louheranta A, Mannelin M et al (2003) The Finnish Diabetes Prevention Study (DPS). Diabetes Care 26:3230–3236
Knowler WC, Barrett-Connor E, Fowler SE et al (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403
Laaksonen DE, Lindstrom J, Lakka TA et al (2005) Physical activity in the prevention of type 2 diabetes: the Finnish Diabetes Prevention Study. Diabetes 54:158–165
Zderic TW, Hamilton MT (2006) Physical inactivity amplifies the sensitivity of skeletal muscle to the lipid-induced downregulation of lipoprotein lipase activity. J Appl Physiol 100:249–257
Funding
The Early ACTID trial was supported by Diabetes UK, the UK Department of Health and Western Comprehensive Local Research Network.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
ARC, RCA and CMD conceived the project. ARC, RCA, AAM, TJP, DJS, NJ, KF and CMD participated in the design and coordination of the project. ARC processed the raw accelerometer data to produce the outcome variables, and ARC, AAM and SS conducted the analyses. ARC drafted the manuscript and all authors reviewed/edited the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooper, A.R., Sebire, S., Montgomery, A.A. et al. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia 55, 589–599 (2012). https://doi.org/10.1007/s00125-011-2408-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-011-2408-x