Abstract
Objectives:1) Identify demographic, clinical, social support, functional, and psychological factors about which data are available within 24 hours of hospital admission associated with emergent unscheduled readmission for a group of older general medicine patients; 2) develop a model to predict emergent readmission.
Design:Interview- and cbart-based study of emergent admissions that occurred within 60 days of discharge.
Setting:General medicine wards of the Memphis Veterans Affairs Medical Center, an 862-bed university-affiliated tertiary care facility.
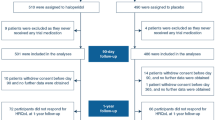
Patients/participants:General medicine patients ≥ 65 years old (n=173). Inclusion criteria were willingness to participate, written consent (patient or family member), and patient interview within 36 hours of admission.
Measurements and main results:The dependent variable was emergent readmission within 60 days of discharge from the hospital. Independent variables included demographic (age, race, income, education), social support (marital status, living arrangements), psychological (cognition, depression), activities of daily living functioning, and clinical (diagnoses, type and source of admission, length of stay, numbers of hospitalizations and days of hospitalizations in the past year, illness severity) parameters. Readmitted patients were emergently admitted and more severely ill, had more diagnoses of chronic obstructive pulmonary disease (COPD) or congestive heart failure (CHF), less ischemic heart disease, and more hospitalizations and hospital days in the past year (all p<0.05). Logistic regression identified diagnostic group (COPD or CHF), emergent admission, and admission severity of illness as predictive of readmission. The likelihood of being readmitted was 5.4. Accuracy of the three-variable model was 76%, predicted value positive, 73%, and predictive value negative, 77%.
Conclusions:Chronically ill patients who are severely ill at index admission and who have had several hospitalizations in the past year tend to be readmitted. Using this model, high-risk patients may be prospectively targeted to reduce readmissions.
Similar content being viewed by others
References
Anderson GF, Steinberg EP. Hospital readmissions in the Medicare population. N Engl J Med. 1984;311:1349–53.
Steel K, Gertman P, Crescenzi C, Anderson J. Iatrogenic illness on a general medical service at a university hospital. N Engl J Med. 1981;304:638–42.
Gooding J, Jette AM. Hospital readmissions among the elderly. J Am Geriatr Soc. 1985;33:595–601.
Graham H, Livesley B. Can readmissions to a geriatric unit be prevented? Lancet. 1983;i:404–6.
Fethke CC, Smith IM, Johnson N. “Risk’ factors affecting readmission of the elderly into the health care system. Med Care. 1986;24:429–37.
Holloway JJ, Medendorp SV, Bromberg J. Risk factors for early readmission among veterans. Health Serv Res. 1990;25:213–37.
Holloway JJ, Thomas JW, Shapiro L. Clinical and sociodemographic risk factors for readmission of Medicare beneficiaries. Health Care Financing Rev. 1988;10:27–36.
Phillips RS, Safran C, Cleary PD, Delbanco TL. Predicting emergency readmissions for patients discharged from the medical service of a teaching hospital. J Gen Intern Med. 1987;2:400–5.
Anderson GF, Steinberg EP. Predicting hospital readmission in the Medicare population. Inquiry. 1985;22:251–8.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Folstein MF, Folstein S, McHugh PR. “Mini-Mental State.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Sherwood SJ, Morris J, Mor V, Gutkin C. Compendium of measures for describing and assessing long term care populations. Boston: Hebrew Rehabilitation Center for the Aged (mimeo), 1977.
Horn SD, Horn RA. Reliability and validity of the Severity of Illness Index. Med Care. 1986;24:159–78.
Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:240–9.
Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. N Engl J Med. 1985;313:793–9.
Gambino R. The misuse of predictive value—or why you must consider the odds. Lab Report. 1989;11:65–71.
Rossner B. Fundamentals of biostatics, 2nd ed. Boston: Duxbury Press, 1986.
Smith DM, Norton JA, McDonald CJ. Nonelective readmissions of medical patients. J Chronic Dis. 1985;38:213–4.
Smith DM, Norton JA, Roberts SD, Maxey WA, McDonald CJ. Unexpected hospital admissions among patients with diabetes mellitus. Arch Intern Med. 1983;143:41–7.
Reed RL, Pearlman RA, Buchner DM. Risk factors for early unplanned hospital readmission in the elderly. J Gen Intern Med. 1991;6:223–8.
Rich MW, Freedland KE. Effect of DRGs on three-month readmission rate of geriatric patients with congestive heart failure. Am J Public Health. 1988;78:680–2.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the Health Services Research and Development Field Program, Little Rock, Arkansas.
Opinions expressed are the authors’ own and do not necessarily reflect those of the Department of Veterans Affairs.
Rights and permissions
About this article
Cite this article
Burns, R., Nichols, L.O. Factors predicting readmission of older general medicine patients. J Gen Intern Med 6, 389–393 (1991). https://doi.org/10.1007/BF02598158
Issue Date:
DOI: https://doi.org/10.1007/BF02598158