Abstract
Biphasic insulin aspart 30 (BIAsp 30) includes 30% soluble rapid-acting insulin aspart (IAsp) along with an intermediate-acting 70% protaminated IAsp that provides coverage of prandial and basal insulin in a single injection. As BIAsp 30 has been available internationally for 10 years, this review provides a comprehensive overview of the discovery of BIAsp 30, its pharmacokinetic and pharmacodynamic profile, safety and efficacy outcomes from the clinical trial programme, ‘real-life’ clinical insights provided by observational study data, and cost effectiveness and quality-of-life information. These studies have demonstrated that BIAsp 30 once or twice daily is an appropriate option for insulin initiation. BIAsp 30 also provides a switch option in patients on biphasic human insulin (BHI). Switching from BHI to BIAsp 30 is associated with improved postprandial glucose (PPG) and reduced nocturnal and major hypoglycaemia, although daytime hypoglycaemia is higher with BIAsp 30. Intensification of BIAsp 30 can be achieved by increasing the number of daily doses up to three times daily with meals. Therefore, BIAsp 30 provides an intensification option for individuals who are not achieving control with basal insulin and would prefer the simplicity of a single biphasic insulin instead of progressing to a basal-bolus approach. BIAsp 30 has a simple dose-titration algorithm, which enables patients to effectively self-titrate their insulin dose. Cost-effectiveness analyses have demonstrated that BIAsp 30 is cost effective or dominant compared with BHI 30 or insulin glargine in a number of healthcare settings. In conclusion, BIAsp 30 offers a simple and flexible option for insulin initiation and intensification that provides coverage of both fasting and prandial glucose.
Similar content being viewed by others
1. Introduction
Biphasic insulin aspart 30 (BIAsp 30) was launched on the international market in 2002, and over the past 10 years it has been used by millions of patients to provide effective control of their diabetes. Given the fact that BIAsp 30 has been used in patients for 10 years, there is a wealth of information available to document its efficacy and safety.
An important goal of diabetes treatment is to achieve target glycated haemoglobin (HbA1c) as early in the course of the disease as possible and to maintain HbA1c as the diabetes progresses. Landmark trials such as DCCT (Diabetes Control and Complications Trial) and the UKPDS (United Kingdom Prospective Diabetes Study) have demonstrated the importance of achieving glycaemic targets in order to reduce the long-term risk of diabetes-related complications.[1,2] For example, in the UKPDS, newly diagnosed patients were randomized to conventional therapy primarily with diet, or intensive therapy with a sulphonylurea or metformin plus insulin.[2] Over a 10-year intervention period there was an 11% reduction in mean HbA1c in the intensive-therapy group compared with the conventional group (7.0% and 7.9%, respectively).[2] The improvement in glycaemic control in the intensively treated group resulted in a 25% reduction in the risk of microvascular endpoints (p < 0.001) and a 12% lower risk for any diabetes-related endpoint (p = 0.029). In a 10-year follow-up, patients returned to normal clinical care and no attempt was made to continue the interventions. Despite the fact that HbA1c difference was lost after 1 year of the interventions finishing, a ‘legacy effect’ was observed in the intensively treated group, with risk reductions in microvascular disease, myocardial infarction, any diabetes-related endpoint and death by any cause, which persisted at the 10-year follow-up.[3]
Both fasting plasma glucose (FPG) and postprandial glucose (PPG) contribute to overall HbA1c control and, at lower HbA1c values, the relative contribution of PPG becomes more important.[4] It is therefore logical, in order to achieve glycaemic targets, that diabetes therapies addressing both FPG and PPG should be initiated from as early as possible in the disease process.[5] The need to target both FPG and PPG is supported by evidence suggesting that uncontrolled PPG is associated with an increased risk of cardiovascular disease, which is an important cause of morbidity and the major cause of death in patients with diabetes.[6,7]
While achieving and maintaining good glycaemic control is important to minimize long-term diabetic complications, the risk of hypoglycaemia increases with more intensive diabetes therapy, which can have a major impact on the health and well-being of patients. Epidemiological associations between hypoglycaemia and cardiovascular morbidity and mortality have been reported, although proof of causality has not been demonstrated.[8] In addition, the health economic benefits of improving HbA1c, measured in quality-adjusted life-years, is counteracted in those patients who experience adverse outcomes such as hypoglycaemia and weight gain.[9] Even non-serious hypoglycaemic events have an important impact on patients, and can result in 1–2 days of lost productivity a month.[10] Therefore, the balance between achieving appropriate glycaemic control and avoiding excessive adverse outcomes needs to be found.
This review will provide a comprehensive summary of BIAsp 30, including information on drug development, pharmacokinetics and pharmacodynamics, clinical trials, observational studies, database studies, meta-analyses, and health economic and quality-of-life research.
1.1 Literature Search
A literature search carried out on 6 June 2011 using the terms ‘biphasic insulin aspart’ identified 162 English-language articles, 52 of which were excluded (25 because BIAsp 30 was not the focus of the article or similar results were reported in other references included in this review and 27 because they were review articles). A separate search was carried out for the ‘Discovery of the Molecule’ section, using the terms ‘Brange J’ and ‘insulin’, ‘phenol B28 Pro Asp’ and ‘bioactivity insulin analogues’, ‘receptor’ and ‘in vivo glucose’. These searches identified 44 publications, of which six were directly relevant to the development of BIAsp 30. Therefore, a total of 116 articles were included in this review.
2. Discovery of Biphasic Insulin Aspart (BIAsp)
The amino acid structure of the human insulin monomer consists of an A-chain with 21 amino acids and a B-chain of 30 amino acids linked covalently by two interchain disulphide bonds.[11] The A-chain includes two antiparallel alpha-helices while the B-chain includes one alpha-helix and a beta-strand (reviewed by Brange and Langkjoer[11]). Insulin has a tendency to self-associate so the monomer exists only at concentrations <10−7 M. At higher concentrations in the pH range 4–8, the molecule dimerises and in the presence of zinc ions the three dimers come together to form hexamers at concentrations >10−5 M.[11]
Human soluble insulin exists in a hexameric form in pharmaceutical preparations, which delays its absorption into the bloodstream following subcutaneous injection as the size of the hexamer impedes diffusion through the capillary membrane into the bloodstream. The dissociation into the dimer and monomer forms, which are more readily absorbed into the bloodstream, requires the molar concentration of insulin to decrease to <10−7 M and the absence of zinc ions.[12] These conditions are achieved as the insulin slowly diffuses away from the injection depot (figure 1).[12]
Dissociation of insulin hexamers following subcutaneous injection. Reproduced from Brange et al.,[12] with permission from the American Diabetes Association. © 1990 American Diabetes Association.
The delay in absorption into the bloodstream means that patients injecting human soluble insulin to control PPG excursions need to inject their insulin at least 30 minutes before a meal. This can be inconvenient and is an issue for those patients with erratic eating habits. In consequence, many patients inject their human soluble insulin much closer to mealtimes, which means that they do not adequately control their PPG excursions and may be exposed to a greater risk of hypoglycaemia. Therefore, there was a need to develop a more rapidly absorbed insulin to address these issues.
2.1 Development of Insulin Aspart
Insulin aspart (IAsp) is a biosynthetically modified analogue of human insulin, in which the only change is the replacement of a single proline amino acid at position 28 in the insulin B-chain with an aspartic acid residue (figure 2).[12] The B28 position was one of the sites chosen for amino acid substitution because it is involved in the formation of dimers but lies outside the receptor-binding region.[13] Substitution of proline with aspartic acid at B28 impairs dimerisation through a charge-repulsion effect in the vicinity of the dimer-forming site, which disrupts the normal van der Waals interaction between the B28 proline and B23 glycine (figure S1 in the Supplemental Digital Content [SDC], available from URL: http://links.adisonline.com/DGZ/A12).[13] This means that IAsp is essentially monomeric at pharmacological concentrations, allowing faster absorption into the bloodstream.[13] The biological activity of IAsp is not affected by the substitution at the B28 position as this area of the molecule is not involved in receptor binding.[14]
Insulin aspart differs from human insulin by the single amino-acid substitution of a proline by an aspartic acid residue at B28. Reproduced from Brange et al.,[12] with permission from the American Diabetes Association. © 1990 American Diabetes Association.
2.2 Formulation of BIAsp 30
With the discovery of neutral protamine Hagedorn (NPH)-like crystals of IAsp,[15] it became possible to develop a biphasic formulation of IAsp. BIAsp 30 includes a mixture of 30% soluble rapid-acting IAsp, along with 70% intermediate-acting crystallised protamine-complexed IAsp. BIAsp 50 (50% soluble and 50% protaminated IAsp) and BIAsp 70 (70% soluble IAsp and 30% protaminated IAsp) are also available for patients who require more prandial insulin to provide effective glycaemic control; however, this review focuses on BIAsp 30. When administered with meals, the rapid-acting soluble IAsp provides coverage for prandial glucose excursions, while the intermediate-acting protaminated IAsp crystals provide coverage of basal glucose, respectively. Protaminated IAsp was preferred to NPH human insulin because mixtures of IAsp and protaminated human insulin underwent exchange during extended contact, whereas this is avoided using mixtures of IAsp and protaminated IAsp.[16] In addition, IAsp retained rapid-acting activity in mixture with protaminated IAsp.[16]
3. Pharmacokinetics and Pharmacodynamics of BIAsp 30
In healthy non-diabetic individuals, basal- and meal-related insulin secretion maintains blood glucose concentrations within the normal range of approximately 4–8 mmol/L (72–144 mg/dL). In individuals with type 2 diabetes mellitus, insulin resistance and the progressive deterioration of beta-cell dysfunction impair blood glucose control. In those individuals who require exogenous insulin, BIAsp 30 offers a pharmacokinetic profile that is closer to normal physiological insulin secretion than both biphasic human insulin (BHI 30) and basal insulin.
3.1 BIAsp 30 vs Biphasic Human Insulin (BHI)-30
The pharmacokinetic and pharmacodynamic profile of BIAsp 30 facilitates more convenient dosing than BHI 30. In a randomized, double-blind, two-way, single-dose crossover study of 24 healthy individuals, BIAsp 30 demonstrated faster absorption and higher peak concentration than BHI 30 (figure 3a).[17] A euglycaemic clamp study in 24 healthy subjects demonstrated an earlier and more pronounced glucose-lowering effect and a similar duration of action of the basal component of BIAsp 30 than BHI 30 (figure 3b).[16]
Pharmacokinetics and pharmacodynamics of biphasic insulin aspart 30 and biphasic human insulin 30. (a) Serum insulin concentration (reproduced from Jacobsen et al.,[17] with kind permission from Springer Science+Business Media). (b) Insulin action (reproduced from Weyer et al.,[16] with permission from the American Diabetes Association. © 1997 American Diabetes Association). BHI = biphasic human insulin; BIAsp = biphasic insulin aspart; * p < 0.0001.
The earlier and more pronounced onset of insulin action with BIAsp 30 means it can be dosed immediately before or following a meal, in contrast to BHI 30, which should be administered at least 30 minutes before a meal. In 93 patients aged ≥65 years, postprandial dosing with BIAsp 30 (up to 20 minutes following a meal) offered similar blood glucose control and no significant difference in hypoglycaemia compared with preprandial dosing (within 5 minutes before the meal).[18] BIAsp 30 injected immediately before a meal provided superior postprandial serum glucose control compared with BHI 30 injected 15 minutes before or immediately before the meal. BIAsp 30 injected after the meal provided comparable PPG control to BHI 30 injected 15 minutes before or immediately before the meal.[19]
In addition to allowing more convenient dosing, there is evidence that BIAsp 30 may also reduce patient exposure to nocturnal low blood glucose versus BHI 30. Patients treated with BIAsp 30 experienced significantly fewer nocturnal episodes (<3.5 mmol/L [<63 mg/dL]) per subject per week than those treated with BHI 30 (1.2 vs 1.6, respectively; p < 0.011) and spent less time at night with low blood glucose (figure S2 in the SDC).[20]
3.2 BIAsp 30 vs Biphasic Insulin Lispro
An open-labelled, randomized, single-dose, three-way crossover study examined the pharmacokinetic and pharmacodynamic characteristics of BIAsp 30, biphasic insulin lispro 25/75 and BHI 30 in 61 individuals with type 2 diabetes already being treated with insulin.[21] Patients visited the study centre on three separate days following an overnight fast. Between visits there was a 5-day washout period. Current oral and intermediate or long-acting insulin medication was discontinued 24 hours before the visit. Preinjection blood glucose target levels of 6–10 mmol/L were achieved using a night-time injection of short-acting insulin. Individuals received a single subcutaneous injection of 0.4 units/kg BIAsp 30, biphasic insulin lispro 25/75 and BHI 30; following which they consumed a standard breakfast. BIAsp 30 was associated with 17% and 10% lower serum glucose excursion between 0–5 hours post-breakfast compared to BHI 30 (p < 0.001) and biphasic insulin lispro 25/75 (p < 0.05), respectively. The time to maximum serum glucose was shorter for BIAsp 30 (75 minutes) than for BHI 30 (88 minutes) or biphasic insulin lispro 25/75 (87 minutes). Measures of insulin pharmacokinetics such as area under the concentration curve (AUC0–5h), maximum plasma drug concentration (Cmax) and time to Cmax (tmax) were significantly better for BIAsp 30 versus BHI 30 but not significantly different for BIAsp 30 and biphasic insulin lispro 25/75.
3.3 BIAsp 30 vs Insulin Glargine
As would be expected, twice-daily dosing of BIAsp 30 resulted in two distinct peaks of plasma insulin compared with insulin glargine’s flatter insulin profile (figure 4).[22] Cmax was achieved approximately 2–3 hours after BIAsp 30 injection, compared with a plateau of plasma insulin between 6 and 16 hours after insulin glargine injection. The overall area under the plasma insulin profile (AUC0–24h) was 28% (p = 0.001) higher for BIAsp 30 than insulin glargine, and the glucose-lowering response (AUC0–24 h) for BIAsp 30 was 34% greater than for insulin glargine (p = 0.037).[22]
Comparison of plasma insulin profiles of twice-daily biphasic insulin aspart 30 and once-daily insulin glargine. Reproduced from Hermansen et al.,[21] with kind permission from Springer Science+Business Media. © 2006 Springer. BIAsp = biphasic insulin aspart.
3.4 BIAsp 30 Three Times Daily vs Basal-Bolus Therapy
In a 24-hour glucose clamp study, in which blood glucose was kept at a constant 5.0 mmol/L by intravenous glucose infusion, BIAsp 30 three times daily showed a similar pharmacodynamic profile (measured by the glucose infusion rate) to basal-bolus therapy with once-daily insulin glargine and three-times daily prandial insulin glulisine in a crossover study in 24 individuals with type 2 diabetes (figure S3 in the SDC).[23] The authors observed that the greater glucose-lowering effect of BIAsp 30 in the evening compared with insulin glargine plus glulisine would require careful titration of the evening dose in order to avoid an increased risk of nocturnal hypoglycaemia.
3.5 Special Populations
The pharmacokinetics of BIAsp 30 have not been investigated in elderly patients, those with renal or hepatic impairment, or in children or adolescents.[24] Although renal or hepatic impairment did not demonstrate any clinically relevant effects on the pharmacokinetics of IAsp.[25] The pharmacokinetic and pharmacodynamic properties of soluble IAsp have been investigated in children (6–12 years) and adolescents (13–17 years) with type 1 diabetes. Insulin aspart was rapidly absorbed in both age groups, with similar tmax as in adults. However, Cmax differed between the age groups, stressing the importance of the individual titration of IAsp.[24] The US FDA classifies BIAsp 30 as pregnancy category B, reflecting the fact that while clinical studies are limited, animal studies of IAsp have demonstrated no adverse effects on spontaneous reproduction or abnormalities in fetal development at clinically relevant doses.[26]
In an exploratory post hoc subanalysis of the INITIATEplus observational trial in previously insulin-naive patients with type 2 diabetes, self-titrated BIAsp 30 was found to be well tolerated and effective in both those aged >65 years and those aged ≤65 years.[27] Patients aged >65 years had greater HbA1c and FPG reductions (p < 0.05). Major and minor hypoglycaemia rates were ≤0.5 episodes per patient-year in both age groups.
4. Safety and Efficacy of BIAsp 30
4.1 Meta-Analysis
Two meta-analyses have compared the safety and efficacy of premix insulin analogues, such as BIAsp 30, with long-acting and BHI regimens in type 2 diabetes.[28,29] In comparison with the long-acting insulin analogues insulin glargine and insulin detemir, BIAsp 30 was more effective at lowering PPG (figure 5a)[28,30–32] and HbA1c (pooled mean difference 0.48%; 95% CI −0.61, −0.34; p < 0.001), with similar reductions in FPG (pooled mean difference = 6.4 mg/dL; 95% CI −1.5, 14.2; p = 0.11).[28] The use of BIAsp 30 was associated with a higher incidence of hypoglycaemia (odds ratio [OR] for minor hypoglycaemia = 2.8; 95% CI 1.4, 5.4; p = 0.003) and more weight gain (pooled mean difference 2.5 kg; 95% CI 1.6, 3.4; p < 0.001).[28]
Biphasic insulin analogues and BHI appear to be similarly effective in lowering FPG. However, BIAsp 30 was reported to be slightly less effective than BHI in lowering FPG (pooled mean difference = 8.3 mg/dL; 95% CI 0.16, 16.5; p = 0.04) but was more effective in lowering PPG (figure 5b),[28,33–35] with similar changes in bodyweight.[28] In comparison with BHI 30, BIAsp 30 was associated with significantly lower rates of nocturnal (relative risk [RR] = 0.50; 95% CI 0.38, 0.67; p < 0.01) and major hypoglycaemia (figure 6),[22,29,34,37] but the rate of daytime hypoglycaemia was 24% higher with BIAsp 30 (RR = 1.24; 95% CI 1.08, 1.43; p < 0.01).[29]
Meta-analysis of major hypoglycaemia in patients with type 2 diabetes mellitus treated with biphasic insulin aspart 30 or biphasic human insulin 30.[21,28,33,35] Reproduced from Davidson et al.,[29] with permission from Elsevier. © 2009 Elsevier. BIAsp = biphasic human insulin; BIAsp = biphasic insulin aspart.
4.2 BIAsp 30 vs BHI or Biphasic Insulin Lispro 25
4.2.1 Type 2 Diabetes
In type 2 diabetes, BIAsp 30 was associated with similar or improved HbA1c control compared with BHI. A number of studies reported significantly improved PPG with BIAsp 30, which is a finding confirmed by the meta-analysis from Qayyum et al.[28] One study identified a significant reduction in major hypoglycaemia, a finding that was confirmed by the Davidson et al.[29] meta-analysis, which reported significant benefits for BIAsp 30 in terms of major and nocturnal hypoglycaemia. A summary of the trials comparing BIAsp 30 and BHI 30 is presented in table I.[33,38–43]
A 12-week multicentre, multinational, open-label two-period crossover trial compared BIAsp 30 and biphasic insulin lispro 25/75 in 137 individuals with type 2 diabetes.[44] Both treatments resulted in similar HbA1c reductions, self-monitored blood glucose levels were comparable; adverse events and hypoglycaemia rates (0.69 vs 0.62 episodes per month with BIAsp 30 and biphasic insulin lispro 25/75; p = 0.292) were also similar between treatments.[44] Based on these data, the authors concluded that the efficacy and safety profiles of the two biphasic insulin analogues were comparable.
4.2.2 Type 1 Diabetes
A randomized parallel-group trial looking into the differences between BIAsp 30 (three times daily plus NPH at bedtime) and BHI 30 (BHI 30 at breakfast, soluble insulin at lunch and dinner, NPH at bedtime) in 167 adolescent patients with type 1 diabetes found comparable effects on HbA1c (adjusted mean HbA1c 9.39% and 9.30% at 16 weeks in the BIAsp 30 and BHI 30 groups, respectively) and similar rates of hypoglycaemia with the two treatments.[45] A trial has examined BIAsp 30 compared with BHI 30 in a mixed population of patients with type 1 or type 2 diabetes, but the results in the subgroup of patients with type 1 diabetes were not reported separately.[36]
4.3 BIAsp 30 vs Basal Insulin
4.3.1 Type 2 Diabetes
Studies demonstrated comparable or superior HbA1c control, superior PPG control, a greater (although overall low) risk of nocturnal hypoglycaemia and greater weight gain with BIAsp 30 than with basal insulin (table II).[32,46–48]
4.3.2 BIAsp 30 vs Basal-Bolus Insulin in Type 1 Diabetes
One small, open-label, crossover study of 23 patients with type 1 diabetes demonstrated that BIAsp 30 three times daily plus NPH insulin at bedtime if required resulted in significantly lower HbA1c than basal-bolus treatment with human insulin over 12 weeks (BIAsp 30 vs human insulin: 8.6% vs 8.3%; p < 0.013).[49] Glycaemic control was comparable in those patients on BIAsp 30 three times daily without NPH compared with basal-bolus treatment.
4.4 BIAsp 30 for Insulin Initiation
Type 2 diabetes is a progressive disease, typically managed in a stepwise fashion, with oral antidiabetic drugs (OADs) introduced once diet and lifestyle changes have been made. Continuing decline of beta-cell function means that the initial choice of OAD (typically metformin) frequently proves unable to provide adequate glycaemic control, so treatment intensification is required. In most people with type 2 diabetes, treatment will eventually include insulin, either as a first step after failure of OAD monotherapy or after various OAD combination therapies have been employed. In addition to the need to re-establish glycaemic control with the introduction of insulin therapy in type 2 diabetes, considerations typically include a desire to minimize the practical burden of therapy for the patient, who may be moving to an injectable therapy for the first time, and to avoid side effects of insulin therapy such as hypoglycaemia and weight gain, which might reduce the acceptability of insulin therapy for the patient.
A number of studies have shown that BIAsp 30 is an appropriate option for insulin-naive patients with type 2 diabetes. In this patient population, BIAsp 30 offers comparable or improved glycaemic control compared with BHI 30, insulin glargine, NPH insulin or OADs along with low rates of hypoglycaemic episodes.[31,33,35,50–68] Key trials are summarized in table III.
Raskin et al.[32] compared twice-daily BIAsp 30 with insulin glargine when initiating insulin in 233 insulin-naive patients with type 2 diabetes. After 24 weeks of insulin treatment, patients receiving twice-daily BIAsp 30 had lower HbA1c levels than those receiving insulin glargine (6.91% vs 7.41%, respectively; p < 0.01) and had experienced a greater HbA1c reduction from baseline (2.79% vs 2.36%, respectively; p < 0.01). A greater proportion of BIAsp 30-treated patients reached target HbA1c levels of ≤6.5% or 7.0% than those receiving insulin glargine (p = 0.036 and p < 0.01, respectively). However, minor hypoglycemia was more frequent with BIAsp 30 than with insulin glargine (3.4 and 0.7 episodes per year, respectively; p < 0.05). Weight gain and daily insulin dose at study end were also higher with BIAsp 30 than with glargine (weight gain 5.4 vs 3.5 kg; p < 0.01; insulin dose 78.5 and 51.3 units per day, respectively).
In a double-blind study by Christiansen et al.,[54] 157 of 403 patients included were insulin-naive, and patients in this group receiving BIAsp 30 twice daily experienced a mean 0.76% reduction in HbA1c levels over 16 weeks. Although the change in HbA1c and the incidence of hypoglycaemia were similar in insulin-naive patients receiving BIAsp 30 twice daily and NPH insulin twice daily, control of PPG was significantly better with BIAsp 30. In the study population as a whole, mean PPG increment over three main meals was significantly lower with BIAsp 30 twice daily than with NPH insulin twice daily (0.69 mmol/L [12.4 mg/dL] difference between groups; p < 0.001). Reductions in FPG levels were similar for the two insulin regimens, but prandial glucose increments were lower with BIAsp 30 than with NPH insulin (5.4 mmol/L vs 7.2 mmol/L [97.2 vs 129.6]; p < 0.05).
Kann et al.[31] compared BIAsp 30 twice daily plus metformin with a regimen of insulin glargine plus glimepiride in 255 insulin-naive patients with type 2 diabetes. In this 26-week study, patients receiving the BIAsp 30 regimen achieved an HbA1c reduction of 1.6%, reaching a mean level of 7.5%; the reduction with BIAsp 30 was significantly greater than with the insulin glargine regimen (0.5% difference between groups; p < 0.001). PPG control was again significantly better with BIAsp 30 (mean prandial glucose increment 1.4 mmol/L [25.2 mg/dL]) than with insulin glargine (2.2 mmol/L [39.6 mg/dL]; p < 0.001). The superior glycaemic control with the BIAsp 30 regimen was reflected in a higher incidence of minor hypoglycaemia (20% vs 9% of patients; p = 0.012), but major hypoglycaemia was very rare in both groups.
Initiation of insulin with BIAsp 30 as an alternative to OAD intensification with a thiazolidinedione was explored in two studies by Raz and colleagues.[64,65] In a 6-week pilot study, patients poorly controlled on glibenclamide monotherapy were randomized either to BIAsp 30 plus rosiglitazone or to glibenclamide plus rosiglitazone (i.e. the addition of a thiazolidinedione to their existing OAD regimen).[64] Mean daily blood glucose level was reduced to a greater extent with the BIAsp 30 regimen than with the thiazolidinedione/glimepiride regimen (reductions of 3.8 mmol/L and 2.1 mmol/L [68.4 and 37.8 mg/dL], respectively; p = 0.01). Modest reductions of HbA1c were observed in the BIAsp 30 plus rosiglitazone group and the OAD combination group (0.7% and 0.2%, respectively), but fructosamine levels were reduced to a greater extent with the BIAsp 30 regimen (difference between groups 42.8 μmol/L; p = 0.02). A further, 18-week study in 281 patients compared BIAsp 30 monotherapy and a combination of BIAsp 30 and pioglitazone with a pioglitazone—glibenclamide regimen in patients previously treated with a sulphonylurea.[65] After 18 weeks, HbA1c levels were significantly lower with BIAsp 30 plus pioglitazone than with glimepiride plus pioglitazone (difference between groups 0.64%; p = 0.005), and were also lower than with BIAsp 30 monotherapy (difference 0.6%; p = 0.008). Mean three-meal prandial glucose increment was lower with BIAsp 30 plus pioglitazone than with glibenclamide plus pioglitazone (difference 0.78 mmol/L [14.8 mg/dL]; p = 0.012).
Initiation of insulin as an alternative to continuing to optimize OAD regimens was also studied using BIAsp 30 by Bebakar et al.[53] in 191 Western Pacific patients with type 2 diabetes. Reduction in HbA1c after 26 weeks was significantly greater with once-daily BIAsp 30 (1.24%; p < 0.01) and twice-daily BIAsp 30 (1.34%; p < 0.005) than with the optimized OAD regimen (0.67%). Similar findings were reported by Raskin et al.,[69] comparing introduction of BIAsp 30 with optimization of an OAD regimen in 200 patients treated with metformin plus pioglitazone. At the end of the study, 76% of subjects treated with BIAsp 30 reached the HbA1c goal of <7.0%, as compared with 24% treated with OADs only.
Twice-daily BIAsp 30 as a first insulin therapy in Japanese patients was examined in a 6-month study comparing this regimen with IAsp three times daily with NPH insulin as necessary.[50,57] Overall, the two regimens gave similar reductions in HbA1c, an effect that was maintained independently of body mass index (BMI), age or diabetes duration.[50]
In addition to trials using twice-daily BIAsp 30, Kilo et al.[35] studied the use of once-daily insulin initiation in a comparison of BIAsp 30, BHI 30 and NPH insulin. In patients in poor glycaemic control at baseline (mean HbA1c 9.5%), once-daily BIAsp 30 plus metformin reduced HbA1c by 1.3% over 12 weeks. Similar reductions were achieved with the other insulins. Although final HbA1c levels remained above target in many patients, these data indicate that starting insulin therapy with once-daily biphasic insulin can achieve useful improvements in control. Similar results were reported in a 26-week, open-labelled, randomized, parallel-group, treat-to-target trial of 480 insulin-naive subjects randomized to either BIAsp 30 before dinner or insulin glargine at bedtime, plus metformin and glimepiride in both arms.[47] Estimated mean reduction in HbA1c from baseline to end of treatment was −1.41% with BIAsp 30 and −1.25% with insulin glargine (p = 0.029). At the end of treatment, mean HbA1c was similar in both groups (7.1% and 7.3% for BIAsp 30 and insulin glargine, respectively). The RR of minor nocturnal hypoglycaemia was higher with BIAsp 30 than with insulin glargine (1.1 vs 0.5 episodes per year; p = 0.003) but overall hypoglycaemia was low in both groups (table II).[47] A third study that examined once-daily BIAsp 30 versus insulin glargine in an Asian population also reported similar results in terms of a small but statistically significant difference in HbA1c lowering (−0.36% difference between groups; p = 0.015), a nonsignificantly higher rate of minor and daytime hypoglycaemia with BIAsp 30, no difference in nocturnal hypoglycaemia, low rates of serious adverse events, low rates of major hypoglycaemic episodes and similar mean bodyweight increase in both groups.[59] In addition, Yang et al.[67,68] explored BIAsp 30 three times daily as a starting insulin in Chinese patients with type 2 diabetes. In this population, three daily BIAsp 30 injections provided better PPG control after lunch and dinner, and greater HbA1c reductions over 24 weeks than twice-daily BIAsp 30 (values reached 7.01% vs 6.68%; p < 0.01 for change from baseline).
4.5 Intensifying BIAsp 30 Therapy
The ability to start insulin therapy with a single daily dose of BIAsp 30 opens the possibility of a stepwise approach to initiation and intensification, in which an initial once-daily regimen is supplemented by a second and potentially a third BIAsp 30 injection as necessary to allow individuals to reach target HbA1c levels. In one such study, Garber et al.[70] examined 100 patients with type 2 diabetes. Patients, 72% of whom were insulin-naive and treated with OADs and the remainder receiving basal insulin plus OADs, were initially treated with a single daily dose of BIAsp 30 (with discontinuation of basal insulin where appropriate).[70] Patients self-titrated their BIAsp 30 dose every 3 or 4 days to achieve pre-breakfast FPG of 80–110 mg/dL (4.4–6.1 mmol/L). After 16 weeks, 21% of patients had achieved an HbA1c level of ≤6.5% and were considered to have completed the study. Of the remaining patients, 68 individuals entered the second phase of the study, in which a second daily BIAsp 30 dose was added. After a further 16 weeks, 25 subjects still did not have an HbA1c of ≤6.5%; these patients then received a third daily BIAsp 30 dose for the final 16-week period. Overall, this strategy — starting with a single daily BIAsp 30 dose and adding a second and third as necessary to achieve HbA1c target — allowed 60% of subjects to achieve HbA1c ≤6.5% and 77% to reach HbA1c ≤7.0%. Although minor hypoglycaemia was relatively frequent, there were no episodes of major hypoglycaemia and no association between the rate of minor hypoglycaemia and the number of daily BIAsp 30 injections.
A similar strategy has been applied in other populations, including Japanese patients with type 2 diabetes.[71,72] In the study by Hosoi et al.,[71] a high baseline HbA1c level (9.6%) was reflected in a lower proportion of patients reaching target HbA1c (51% to ≤7.0%) than in the study by Garber et al.[70] Similarly, Yoshioka et al.[72] reported a 49% achievement rate to HbA1c ≤7.0% in a population with baseline HbA1c of 8.9%.
4.6 BIAsp 30 vs Exenatide
Two studies comparing BIAsp 30 and twice-daily exenatide were identified.[63,73] Bergenstal et al.[73] demonstrated that treatment with once-daily BIAsp 30 and twice-daily BIAsp 30 in combination with metformin gave superior glycaemic control to that of exenatide. Both twice-daily and once-daily BIAsp 30 produced statistically and clinically significantly greater reductions of HbA1c from baseline than exenatide (2.76%, 2.34% and 1.75% for twice-daily BIAsp 30, once-daily BIAsp and exenatide groups, respectively; p < 0.001). This is in contrast to the Nauck et al.[63] study, where glycaemic control achieved with twice-daily exenatide was demonstrated to be non-inferior to that with twice-daily BIAsp 30. However, a commentary by Home[74] identified that, while an optimal dose of exenatide was utilized in the trial (10 μg daily), insulin dose adjustment was left to the investigator and at 52 weeks the premix insulin dose was only 24 U/day, well below doses normally encountered in clinical practice. It is therefore possible that the results reported by Nauck et al.[63] reflect suboptimal insulin dosing.
4.7 Guidance on Dose Titration and Insulin Intensification
Titration of BIAsp 30 is based on the lowest pre-meal glucose value over the preceding 3 days and the dose should be titrated weekly (table S1 in the SDC).[24] For those patients on twice-daily dosing, titration of the breakfast dose should be based on the lowest pre-dinner glucose and the titration of the dinner dose should be based on the lowest pre-breakfast glucose value. The dosage should not be increased if any hypoglycaemic events are reported within the 3 days. The dose adjustments are shown in table S1 in the SDC.
A consensus statement covering the intensification of basal insulin to BIAsp 30, and the intensification of once-daily or twice-daily BIAsp 30 to twice- or three-times daily BIAsp 30, is available.[75] The aim of this statement is to offer practical guidance to enable primary care or specialist physicians to intensify insulin therapy using BIAsp 30. According to the statement, physicians should consider intensifying basal insulin to twice-daily BIAsp 30 if HbA1c is >8.0%, or if HbA1c is between 7% and 8% and FPG is optimized. If a patient on once- or twice-daily BIAsp 30 has within-target FPG but an HbA1c >7%, a switch to twice- or three-times daily BIAsp 30 should be considered. If their FPG is above target, the dose should be titrated to achieve FPG 4–6 mmol/L (72–108 mg/dL); however, if hypoglycaemia occurs, an additional daily dose should be added rather than further dose titration.
4.8 Antibodies
The development of antibodies against insulin is common in individuals with diabetes who are administering exogenous insulin; however, their clinical relevance is debatable. Antibody responses to IAsp (n = 1534) and human insulin (n = 886) were investigated in four multinational, open studies of up to 1 year in duration.[76] In all four studies, cross-reactive antibodies increased in patients exposed to IAsp, with a maximum at 3 months, after which there was a decrease toward baseline levels at 9–12 months. No consistent relationship between antibody formation and glycaemic control or adverse events was observed. Similar results were reported by Chen et al.[77] in 23 patients with type 1 diabetes treated with BIAsp 30 for 12 weeks. Comparing individuals with high and medium concentrations of circulating insulin antibodies, higher levels of total but not free insulin were observed in those with high antibody concentrations; however, no difference in glycaemic control was observed.
5. Clinical Evidence Translating to Clinical Practice
A number of large, prospective, observational studies observing the effects of initiating, switching to or intensifying with BIAsp 30 have been conducted. While randomized controlled trials (RCTs) are rightly seen as the ‘gold standard’ for providing an evidence-based approach to medicine, observational studies have an important and complementary role. Prospective observational studies can recruit larger patient cohorts, which means they can be useful in predicting rare adverse events that might be missed in smaller studies.[78] In addition, patient demographics and treatment in observational studies more closely reflect ‘real-life’ clinical practice than the more tightly controlled RCT setting. This means that observational studies can be useful to corroborate results from RCTs under more typical therapeutic conditions.[78,79] However, observational studies are more open to bias and confounding than RCTs as they reflect clinical practice and lack randomization as well as placebo or comparator treatment arms.
5.1 IMPROVE™: Analysing BIAsp 30 Safety and Efficacy in ‘Real-life’ Clinical Practice
IMPROVE™ was a 26-week observational trial that included 51 430 individuals with type 2 diabetes across 11 countries (China, India, Japan, Poland, Italy, Canada, Russia, Greece, Iran, Gulf region and South Korea), of which data from eight countries have been published.[80] Individuals were enrolled into three study groups depending on their previous diabetes treatment: no previous pharmaceutical therapy, OADs only, and patients prescribed insulin with or without OADs. HbA1c, PPG and FPG levels, as well as the rate of hypoglycaemia, were measured in all three subsets of patients at baseline and after 26 weeks after initiation with/change to BIAsp 30 (table IV).[68,81–83] Major hypoglycaemia was significantly reduced in all patient subsets (no pharmaceutical therapy: 0.029 [baseline] to 0.002 events per patient-year; OADs only: 0.071 [baseline] to 0.006 events per patient-year; insulin±OADs: 0.269 [baseline] to 0.021 events per patient-year).[81]
5.2 PRESENT™: Examining BIAsp 30 Safety and Efficacy in 15 Countries Over 6 Months
PRESENT™ (Physicians’ Routine Evaluation of Safety & Efficacy of NovoMix 30 Therapy) was a 6-month observational study of 31 044 individuals with type 2 diabetes across 15 countries initiating or switching diabetes treatment to BIAsp 30 (with or without OADs). The key results are summarized in table V.[84–88] In one subanalysis of this trial, subjects were enrolled into different subgroups depending on age, BMI or ethnic background.[89] From data collected this way, it was seen that age and BMI did not affect the HbA1c-lowering qualities or the safety of BIAsp 30. Ethnic origin, on the other hand, did seem to play a role in HbA1c levels, being highest for Black individuals at baseline (11.6%) compared with Asian/Pacific Island (9.3%), Middle Eastern/Arabic (9.6%) and White (9.6%) populations. Rates of hypoglycaemia were much lower for the Black than the White subjects at the beginning of the trial (1.86 vs 7.81 events per patient-year, respectively). Overall outcomes showed that HbA1c was reduced by 1.81%, FPG was lowered by 3.74 mmol/L (67.32 mg/dL) and hypoglycaemia decreased from 5.4 to 2.2 events per patient-year with BIAsp 30 (all p < 0.001).[84]
5.3 Additional Studies: Further Analyses of BIAsp 30 Safety and Efficacy
In a multinational study across Austria, Germany and Switzerland, insulin-naive patients with type 2 diabetes were randomized to receive either insulin analogue basal-bolus treatment or BIAsp 30.[90] BIAsp 30 therapy lowered HbA1c to a similar degree as insulin analogue basal-bolus regimens (−1.23% and −1.56%, respectively) and both treatments were associated with similar, low rates of hypoglycaemia.[90]
In addition to the IMPROVE™ and PRESENT™ studies, data from the A1chieve study, the largest ever observational study of insulin use in type 2 diabetes, is now available. The A1chieve study has been performed across 30 countries and is examining the safety and efficacy of BIAsp 30, insulin detemir and IAsp treatment in over 60 000 individuals with type 2 diabetes.[91,92] Mean baseline HbA1c in A1chieve was 9.5%. At 6 months, HbA1c had improved by 2.1% in the entire cohort, 2.2% for prior non-insulin users and 1.8% for prior insulin users. Results achieved by BIAsp 30, insulin detemir and IAsp were similar and did not depend on prior insulin use. Hypoglycaemia did not increase in those initiating insulin, and was reduced in those switching insulin. There was no significant change in bodyweight, while lipid profile and systolic blood pressure were improved.[92]
5.4 Country-Specific Populations and Subgroup Analyses
A number of observational studies, or subgroup analyses of larger multinational observational studies, have examined the safety and efficacy of BIAsp 30 in country-specific populations. The Chinese, Indian, Iranian, Italian and Korean cohorts of the IMPROVE™ and PRESENT™ studies have been published.[93–100] These subgroup analyses of large multinational observational studies are a useful resource by providing a way to benchmark local outcomes against those achieved globally. Similarly, smaller single-country observational studies examining the initiation of BIAsp 30, such as those carried out in the UK and Denmark, provide physicians with clinically relevant information for the type of patients that they see in daily practice.[101,102]
5.5 Retrospective Database Studies
In one retrospective database study that included data from 7720 patients from over 350 UK general practices, BIAsp 30 demonstrated significantly greater HbA1c reductions versus BHI 30 in insulin-naive type 1 patients (0.57%; p = 0.045), insulin-naive patients with type 2 diabetes (0.17%; p = 0.003) and insulin-experienced patients with type 2 diabetes (0.23%; p = 0.007).[102] The incidence rate ratio for hypoglycaemia was significantly reduced in insulin-naive patients with type 2 diabetes (0.74; 95% CI 0.62, 0.89; p = 0.001) but not for other groups. Logistic regression analysis adjusting for baseline HbA1c, age, sex and insulin status demonstrated a significantly reduced risk of experiencing a hypoglycaemic event in patients with type 2 diabetes (OR = 0.718; 95% CI 0.593, 0.868; p = 0.001) but not in type 1 diabetes.
5.6 Devices
Insulin pens offer more convenience than vial insulin because they are easier to use, more portable and allow the rapid selection of the correct dose. By enabling more discrete injection, they minimize potential embarrassment associated with public injection,[103] giving individuals more lifestyle flexibility. In addition, insulin pens offer a more accurate way to inject insulin. This can be particularly important for those patients with vision impairment or manual dexterity issues and can allow them to independently manage their disease. By enabling more convenient, discrete and accurate dosing of insulin, an insulin pen may improve patients’ adherence to treatment and allow them to more successfully manage their diabetes.
In a randomized, open-label, crossover study, 121 insulin-experienced patients with type 1 or type 2 diabetes were transferred to BIAsp 30.[103] Following 4-week dose optimization with BIAsp 30 using their usual type of syringe, patients were randomized to a prefilled disposable pen (FlexPen® [FP]) or vial and syringe for 4 weeks, after which they switched to the other administration device for the final 4 weeks.[103] A higher percentage of patients preferred the FP (74%): they felt it was more discrete for public use (85%), found it easier to use (74%) and found the dosing scale easier to read (85%) than the vial and syringe.[103] The Next Generation FlexPen® (NGFP) was launched in 2009 and was demonstrated to be at least as accurate as the FP, required less injection force and was judged by patients to be more comfortable and easier to use than the FP.[104] In another study, a total of 64 individuals with type 1 or type 2 diabetes were asked to compare the FP with the NGFP for visual appearance, ease of needle attachment, ease of use, convenience, trust and safety.[105] The majority of patients found it easier to identify the correct insulin analogue with the NGFP; attaching the NovoTwist® needle to the NGFP was significantly easier than attaching the NovoFine® needle to the FP; the NGFP was easier to use; and a slight majority (52%) had more trust and confidence in the NGFP than in the FP.[105] Overall, 95% of patients preferred the NGFP and 77% preferred the NovoTwist® needle.[105]
6. Newer Concepts of Practice
6.1 Cost Effectiveness (Health Economics)
Cost-effectiveness assessments of treatments for diabetes ideally take into account both the direct and the indirect costs of treatment and complications and should relate these costs to the clinical benefits associated with treatment (table S2 in the SDC). Costs include the direct acquisition cost of the drug, medical costs associated with scheduled physician visits, costs due to acute adverse events such as hypoglycaemia, the costs of treating long-term diabetic complications and lost productivity.
The studies reviewed utilized the Center for Outcomes Research (CORE) diabetes model, which is a validated computer simulation that projects long-term health outcomes and economic consequences of different treatments by assessing the likelihood of patients developing complications such as cardiovascular disease, eye disease, hypoglycaemia, nephropathy and renal failure, neuropathy, foot ulcer, amputation, stroke, ketoacidosis, lactic acidosis and mortality; as well as costs of adverse events like hypoglycaemia.[106]
Given country-specific differences in medical practice and costs, it is difficult to extrapolate data from one country to predict cost effectiveness in another. In this respect, use of country-specific cohorts, costs, utility data, information on medical practices as well as clinical probability data where available, combined with data from large, well run observational trials can provide important input on which to base finely tuned, country-specific, health economic analyses.
The cost-effectiveness comparisons with insulin glargine included in this review[107–110] all utilized data from the 28-week INITIATE™ trial[31] to provide baseline characteristics and treatment outcomes for the simulated cohorts. Modelling in Palmer et al.[109] also utilized data from the OnceMix study.[47] These simulated cohorts were then used to model long-term cost effectiveness over a 35-year period. The INITIATE™ study demonstrated that BIAsp 30 plus OADs lowered HbA1c to a greater extent than the same oral combination with insulin glargine (−2.79 vs −2.36%, respectively), but with a higher daily insulin dose (+0.82 vs +0.52 units/kg, respectively), change in bodyweight (+5.4 vs +3.5 kg, respectively) and minor hypoglycaemia (3.4 vs 0.7 episodes per patient-year, respectively).[31] Costs were modelled in the US, Chinese, Swedish and UK settings using local pharmacy and hospital costs. The total cost in each treatment arm included direct medical resource costs plus the costs of treating complications. Therefore, if the CORE model predicted that treatment A would reduce the frequency, or delay the onset, of diabetic complications versus treatment B, then the total cost of treatment A may be less than treatment B (despite higher medical resource costs). On this basis, the CORE model demonstrated that BIAsp 30 was dominant (e.g. BIAsp 30 was more effective and the total lifetime treatment costs were lower) in China and Sweden (table VI).[109,110] BIAsp 30 was shown to be cost effective (e.g. the total lifetime costs of treatment were higher with BIAsp 30, but the additional costs were in the range deemed to be acceptable value for money in the respective countries for the efficacy benefits gained) in the US and the UK (table VI).[107,108]
Three published analyses have examined the cost effectiveness of BIAsp 30 compared with BHI using the Saudi Arabian and South Korean cohorts of PRESENT™ to model costs in those countries and the Canadian cohort of IMPROVE™ to model US costs.[111–113] BIAsp 30 was demonstrated to be dominant over BHI 30 in the Saudi Arabian setting and was cost effective in the South Korean and US settings (table VII).
6.2 Quality of Life and Treatment Satisfaction
Treatment satisfaction can positively impact patient compliance, cost of care and self-management behaviour.[114] Treatment satisfaction was examined in 233 individuals recruited to the INITIATE™ trial, which compared twice-daily BIAsp 30 and once-daily insulin glargine.[114] Neuropathy and the number of hypoglycaemic events during the day significantly negatively impacted treatment satisfaction while treatment efficacy significantly improved treatment satisfaction.[114] However, there was no significant relationship between the number of minor hypoglycaemic events, weight gain or treatments with one versus two daily injections with overall treatment satisfaction.[114] In a larger sample of 17 488 patients from the IMPROVE™ study, switching from prior OAD therapy to BIAsp 30 was associated with significantly improved treatment satisfaction based on the DiabMedSat testing of Overall, Treatment Burden, Symptoms and Efficacy, and Treatment Satisfaction (p < 0.001).[115] In a regression analysis, achieving target HbA1c levels was associated with greater satisfaction in the Symptoms and Treatment Burden domains, while weight gain and experiencing minor hypoglycaemic events were negatively associated with Treatment Satisfaction.[115] Similar results were reported in the study of treatment satisfaction of patients in the Indian cohort (n = 349) of IMPROVE™, with significant improvements in overall treatment satisfaction and the domains such as burden, symptoms and efficacy (p < 0.001).[116] Interestingly, analysis of the Japanese IMPROVE™ cohort demonstrated significant improvements in burden (p < 0.041), efficacy (p < 0.001) and symptoms (p < 0.049) following the switch from prior OAD to BIAsp 30 treatment, but overall treatment satisfaction was similar (p < 0.079).[117]
7. Where is BIAsp 30 Heading?
The prevalence of diabetes continues to rise globally, reflecting changing lifestyles and the increasing prevalence of obesity. The impact of diabetes on healthcare costs is high and will continue to increase. Given the increasing numbers of patients and limited healthcare resources, it is likely that there will be an increasing need for patients to be treated in a primary care rather than in a specialist setting, and there will be greater emphasis on patients self-managing their disease. In this context, premix insulins, such as BIAsp 30, provide a useful option as they offer the simplicity and convenience of being able to control both fasting and prandial glucose with a single injection. In addition, a simple dose-titration algorithm means that patients can adjust their daily dosing without the need to consult their healthcare provider. The ability of patients to self-monitor and self-adjust their BIAsp 30 regimen was demonstrated by a study of 149 patients with type 2 diabetes who initiated BIAsp 30 after failing on OADs or existing insulin regimens.[118] Patients were trained to self-monitor and adjust their BIAsp 30 over a maximum of 10 weeks. Diabetes nurses were consulted by telephone after each weekly series of blood glucose measurements until the patient was confident in self-adjusting their insulin doses. Self-adjusted BIAsp 30 resulted in significant reductions in mean HbA1c (1.9%), mean FPG (2.8 mmol/L) and mean PPG (2.9 mmol/L) [p = 0.001]. Additionally, 91% and 52% of patients achieved HbA1c <7% and ≤6.5%, respectively. No major or nocturnal hypoglycaemic episodes were reported, although 15% of patients reported minor hypoglycaemia. Similar results, supporting the ability of patients to self-titrate BIAsp 30, were reported in a large study of almost 5000 patients in a primary care setting.[119] These results showed HbA1c reductions of approximately 2.5% to around 7.5% in three groups of patients randomized to self-titration of BIAsp 30 with no dietary counselling, or one or three dietary counselling sessions conducted by telephone.[119]
Premix insulins also offer a simple route to insulin intensification as further mealtime doses can be up to three times daily, which means that patients can stick with a familiar insulin even as their diabetes progresses. Only once their diabetes is no longer controlled by three times daily premix would patients and their healthcare providers need to consider a move to a more complicated basal-bolus regimen.
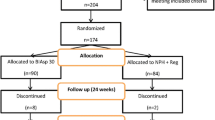
There are currently two ongoing RCTs and one planned RCT that will provide additional clinical insights into BIAsp 30. The EasyMix™ trial (BIAsp 3756) was conducted in insulin-naive Chinese and Japanese subjects with type 2 diabetes. It assessed BIAsp 30 and insulin glargine (both once daily) in combination with metformin and glimepiride. The results from the EasyMix™ trial will shortly be available at ClinicalTrials.gov. The SimpleMix™ trial (BIAsp 3878) recruited subjects between September and December 2011 with the primary aim of demonstrating that subject-driven titration is non-inferior to investigator-driven titration of BIAsp 30 in type 2 diabetes inadequately controlled on basal insulin analogues. In addition, a new BIAsp 30 RCT (BIAsp 3963) is recruiting patients as of June 2012 and will examine combination therapy with BIAsp 30 and sitagliptin.
8. Discussion
As it enters its 10th year on the international market, BIAsp 30 is a time-tested molecule that has demonstrated a positive efficacy and safety profile, having been used by millions of diabetes patients worldwide. In addition, BIAsp 30 is supported by an extensive selection of efficacy and safety data ranging from multinational RCTs to observational data from large international observational studies, including data from A1chieve, the largest observational study of insulin use in type 2 diabetes, which includes over 60 000 patients.[91,92] By combining rapid- and intermediate-acting insulins in a single formulation, BIAsp 30 offers a simple and convenient way to provide coverage of both FPG and PPG. Administered once or twice daily, BIAsp 30 is a useful option for individuals initiating insulin. BIAsp 30 can be intensified up to three times daily with meals, giving options for treatment intensification as an individual’s diabetes progresses. Given the benefits of BIAsp 30 over BHI 30 — including the convenience of being able to inject immediately before or following a meal, improved PPG control and reduced major and nocturnal hypoglycaemia — most patients on BHI 30 may benefit from a switch to BIAsp 30. It has become increasingly clear that hypoglycaemic episodes, whether major or minor, have a detrimental effect on the lives of individuals with diabetes as well as their families; result in lost productivity; and have both acute, and potentially longer-term, adverse health impacts. Therefore, treatments such as BIAsp 30 or other premixed insulin analogues such as biphasic insulin lispro 25, which offer the potential to reduce the risk of hypoglycaemic episodes, can have important benefits for patients. BIAsp 30 also provides a simple way to intensify from basal insulin if PPG coverage is required, which can be useful in those patients who have concerns about the complexity of basal-bolus options. BIAsp 30 has been shown to be a cost-effective or dominant (cost-saving and more effective than the comparator) treatment option in a number of countries, and studies have demonstrated significantly improved quality of life for patients switching from OADs to BIAsp 30. In conclusion, BIAsp 30 offers a simple, flexible option with a positive safety profile for insulin initiation and intensification that provides coverage of FPG and PPG.
References
DCCT (Diabetes Care and Complications Trial) Research group. The absence of a glycemic threshold for the development of long-term complications: the perspective of the Diabetes Control and Complications Trial. Diabetes 1996; 45: 1289–98
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837–53
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008; 359: 1577–89
Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care 2003; 26: 881–5
Leiter LA, Ceriello A, Davidson JA, et al., on behalf of the International Prandial Glucose Regulation Study Group. Postprandial glucose regulation: new data and new implications. Clin Ther 2005; 27 Suppl. B: S42–56
International Diabetes Federation (IDF). Guideline for management of postmeal glucose. 2007 [online]. Available from URL: http://www.idf.org/webdata/docs/Guideline_PMG_final.pdf [Accessed 2011 Oct 10]
Ceriello A, Davidson J, Hanefeld M, et al., on behalf of the International Prandial Glucose Regulation Study Group. Postprandial hyperglycaemia and cardiovascular complications of diabetes: an update. Nutr Metab Cardiovasc Dis 2006; 16: 453–6
Desouza CV, Bolli GB, Fonseca V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care 2010; 33: 1389–94
McEwan P, Evans M, Kan H, et al. Understanding the inter-relationship between improved glycaemic control, hypoglycaemia and weight change within a long-term economic model. Diabetes Obes Metab 2010; 12: 431–6
Brod M, Christensen T, Thomsen TL, et al. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health 2011; 14: 665–71
Brange J, Langkjoer L. Insulin structure and stability. Pharm Biotechnol 1993; 5: 315–50
Brange J, Owens DR, Kang S, et al. Monomeric insulins and their experimental and clinical implications. Diabetes Care 1990; 13: 923–54
Brange J, Ribel U, Hansen JF, et al. Monomeric insulins obtained by protein engineering and their medical implications. Nature 1988; 333: 679–82
Drejer K. The bioactivity of insulin analogues from in vitro receptor binding to in vivo glucose uptake. Diabetes Metab Rev 1992; 8: 259–86
Balschmidt P; Crystals of Asp(B28) human insulin and preparations containing such crystals. US pat. 5547930, US pat. 5834422, EPO pat. 705275 (1993)
Weyer Heise T, Heinemann L. Insulin aspart in a 30/70 premixed formulation: pharmacodynamic properties of a rapid-acting insulin analog in stable mixture. Diabetes Care 1997; 20: 1612–4
Jacobsen LV, Søgaard B, Riis A. Pharmacokinetics and pharmacodynamics of a premixed formulation of soluble and protamine-retarded insulin aspart. Eur J Clin Pharmacol 2000; 56: 399–403
Warren ML, Conway MJ, Klaff LJ, et al. Postprandial versus preprandial dosing of biphasic insulin aspart in elderly type 2 diabetes patients. Diabetes Res Clin Pract 2004; 66: 23–9
Kapitza C, Rave K, Ostrowski et al. Reduced postprandial glycaemic excursion with biphasic insulin Aspart 30 injected immediately before a meal. Diabet Med 2004; 21: 500–1
McNally PG, Dean JD, Morris AD, et al. Using continuous glucose monitoring to measure the frequency of low glucose values when using biphasic insulin aspart 30 compared with biphasic human insulin 30: a double-blind crossover study in individuals with type 2 diabetes. Diabetes Care 2007; 30: 1044–8
Hermansen K, Colombo M, Storgaard H, et al. Improved postprandial glycemic control with biphasic insulin aspart relative to biphasic insulin lispro and biphasic human insulin in patients with type 2 diabetes. Diabetes Care 2002; 25: 883–8
Luzio S, Dunseath G, Peter R, et al. Comparison of the pharmacokinetics and pharmacodynamics of biphasic insulin aspart and insulin glargine in people with type 2 diabetes. Diabetologia 2006; 49: 1163–8
Heise T, Heinemann L, Hövelmann U, et al. Biphasic insulin aspart 30/70: pharmacokinetics and pharmacodynamics compared with once-daily biphasic human insulin and basal-bolus therapy. Diabetes Care 2009; 32: 1431–3
NovoMix 30 Penfill 100 U/ml, NovoMix 30 FlexPen 100 U/ml. Summary of product characteristics. Crawley: Novo Nordisk Limited, 2011 [online]. Available from URL: http://www.medicines.org.uk/EMC/medicine/8591/SPC/NovoMix+30+Penfill+100+U+ml%2c+NovoMix+30+FlexPen+100+U+ml/ [Accessed 2011 Sep 12]
Holmes G, Galitz L, Hu P, et al. Pharmacokinetics of insulin aspart in obesity, renal impairment, or hepatic impairment. Br J Clin Pharmacol 2005; 60: 469–76
NovoLog® Mix 70/30. US prescribing information. Princeton (NJ): Novo Nordisk Inc., 2010 [online]. Available from URL: http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021172s045s049lbl.pdf [Accessed 2011 Nov 17]
Oyer DS, Shepherd MD, Coulter FC, et al., on behalf of the Initiateplus Study Group. Efficacy and tolerability of self-titrated biphasic insulin aspart 70/30 in patients aged >65 years with type 2 diabetes: an exploratory post hoc sub-analysis of the INITIATEplus trial. Clin Ther 2011; 33: 874–83
Qayyum R, Wilson LM, Bolen S, et al. Comparative effectiveness, safety, and indications of insulin analogues in premixed formulations for adults with type 2 diabetes. Rockville (MD): Agency for Healthcare Research and Quality (US), 2008 Sep (Comparative Effectiveness Reviews, No. 14.) [online]. Available from URL: http://www.ncbi.nlm.nih.gov/books/NBK43174/ [Accessed 2012 Jul 13]
Davidson JA, Liebl A, Christiansen JS, et al. Risk for nocturnal hypoglycemia with biphasic insulin aspart 30 compared with biphasic human insulin 30 in adults with type 2 diabetes mellitus: a meta-analysis. Clin Ther 2009; 31: 1641–51
Holman RR, Thorne KI, Farmer AJ, et al. Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med 2007; 357: 1716–30
Kann PH, Wascher T, Zackova V, et al. Starting insulin therapy in type 2 diabetes: twice-daily biphasic insulin Aspart 30 plus metformin versus once-daily insulin glargine plus glimepiride. Exp Clin Endocrinol Diabetes 2006; 114: 527–32
Raskin P, Allen E, Hollander P, et al. Initiating insulin therapy in type 2 diabetes: a comparison of biphasic and basal insulin analogs. Diabetes Care 2005; 28: 260–5
Abrahamian H, Ludvik B, Schernthaner G, et al. Improvement of glucose tolerance in type 2 diabetic patients: traditional vs. modern insulin regimens (results from the Austrian Biaspart Study). Horm Metab Res 2005; 37: 684–9
Boehm BO, Home PD, Behrend C, et al. Premixed insulin aspart 30 vs. premixed human insulin 30/70 twice daily: a randomized trial in type 1 and type 2 diabetic patients. Diabet Med 2002; 19(5): 393–9
Kilo C, Mezitis N, Jain R, et al. Starting patients with type 2 diabetes on insulin therapy using once-daily injections of biphasic insulin aspart 70/30, biphasic human insulin 70/30, or NPH insulin in combination with metformin. J Diabetes Complications 2003; 17: 307–13
Boehm BO, Home PD, Behrend C, et al. Premixed insulin aspart 30 vs. premixed human insulin 30/70 twice daily: a randomized trial in type 1 and type 2 diabetic patients. Diabet Med 2002; 19: 393–9
Iwamoto Y. A randomised, multicentre trial of biphasic insulin aspart versus biphasic human insulin in type 2 diabetes [abstract]. Diabetologia 2003; 46: A270
Boehm BO, Vaz JA, Brøndsted L, et al. Long-term efficacy and safety of biphasic insulin aspart in patients with type 2 diabetes. Eur J Intern Med 2004; 15: 496–502
Schmoelzer I, de Campo A, Pressl H, et al. Biphasic insulin aspart compared to biphasic human insulin reduces postprandial hyperlipidemia in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes 2005; 113: 176–81
Velojic-Golubovic M, Mikic D, Pesic M, et al. Biphasic insulin aspart 30: better glycemic control than with premixed human insulin 30 in obese patients with type 2 diabetes. J Endocrinol Invest 2009; 32: 23–7
Fakhoury WK, Richter H, Christensen TE. Real-life dosage and clinical efficacy of biphasic insulin preparations in patients with type 2 diabetes. Adv Ther 2010; 27: 859–69
Temizel M, Mert M, Bozbey C, et al. Evaluation of the weight-increasing effects of biphasic analog and regular NPH insulin mixtures in patients with type 2 diabetes mellitus. J Diabetes 2010; 2: 250–5
Ohira M, Endo Oyama T, et al. Improvement of postprandial hyperglycemia and arterial stiffness upon switching from premixed human insulin 30/70 to biphasic insulin aspart 30/70. Metabolism 2011; 60: 78–85
Niskanen L, Jensen LE, Råstam J, et al. Randomized, multinational, open-label, 2-period, crossover comparison of biphasic insulin aspart 30 and biphasic insulin lispro 25 and pen devices in adult patients with type 2 diabetes mellitus. Clin Ther 2004 Apr; 26(4): 531–40
Mortensen H, Kocova M, Teng LY, et al. Biphasic insulin aspart vs. human insulin in adolescents with type 1 diabetes on multiple daily insulin injections. Pediatr Diabetes 2006; 7: 4–10
Ligthelm RJ, Mouritzen U, Lynggaard H, et al. Biphasic insulin aspart given thrice daily is as efficacious as a basal-bolus insulin regimen with four daily injections: a randomised open-label parallel group four months comparison in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes 2006; 114: 511–9
Strojek K, Bebakar WM, Khutsoane DT, et al. Once-daily initiation with biphasic insulin aspart 30 versus insulin glargine in patients with type 2 diabetes inadequately controlled with oral drugs: an open-label, multinational RCT. Curr Med Res Opin 2009; 25: 2887–94
Ligthelm RJ, Gylvin T, DeLuzio T, et al. A comparison of twice-daily biphasic insulin aspart 70/30 and once-daily insulin glargine in persons with type 2 diabetes mellitus inadequately controlled on basal insulin and oral therapy: a randomized, open-label study. Endocr Pract 2011; 17: 41–50
Chen JW, Lauritzen T, Bojesen A, et al. Multiple mealtime administration of biphasic insulin aspart 30 versus traditional basal-bolus human insulin treatment in patients with type 1 diabetes. Diabetes Obes Metab 2006; 8: 682–9
Arai K, Hirao K, Yamauchi M, et al., on behalf of the Japan Diabetes Clinical Data Management Study Group. Influence of BMI, age and duration of diabetes mellitus on glycaemic control with twice-daily injections of biphasic insulin aspart 30 versus multiple daily injections of insulin aspart (JDDM 18): retrospective reanalysis of a 6-month, randomized, open-label, multicentre trial in Japan. Clin Drug Investig 2010; 30: 35–40
Ascić-Buturović B. Effect of biphasic insulin aspart 30 combined with metformin on glycaemic control in obese people with type 2 diabetes. Bosn J Basic Med Sci 2007; 7: 335–8
Ayad NM, Fattah WA, Bakry H. Biphasic insulin aspart 30 treatment improves glycemic control among patients with type 2 diabetes in Saudi Arabia and the Gulf region. Saudi Med J 2008; 29: 919–20
Bebakar WM, Chow CC, Kadir KA, et al., on behalf of the BIAsp-3021 study group. Adding biphasic insulin aspart 30 once or twice daily is more efficacious than optimizing oral antidiabetic treatment in patients with type 2 diabetes. Diabetes Obes Metab 2007; 9: 724–32
Christiansen JS, Vaz JA, Metelko Z, et al. Twice daily biphasic insulin aspart improves postprandial glycaemic control more effectively than twice daily NPH insulin, with low risk of hypoglycaemia, in patients with type 2 diabetes. Diabetes Obes Metab 2003; 5: 446–54
Cucinotta D, Smirnova O, Christiansen JS, et al. Three different premixed combinations of biphasic insulin aspart: comparison of the efficacy and safety in a randomized controlled clinical trial in subjects with type 2 diabetes. Diabetes Obes Metab 2009; 11: 700–8
Ebato C, Shimizu T, Arakawa M, et al. Effect of sulfonylureas on switching to insulin therapy (twice-daily biphasic insulin aspart 30): comparison of twice-daily biphasic insulin aspart 30 with or without glimepiride in type 2 diabetic patients poorly controlled with sub-maximal glimepiride. Diabetes Res Clin Pract 2009; 86: 31–6
Hirao K, Arai Yamauchi M, et al., on behalf of the Japan Diabetes Clinical Data Management Study Group. Six-month multicentric, open-label, randomized trial of twice-daily injections of biphasic insulin aspart 30 versus multiple daily injections of insulin aspart in Japanese type 2 diabetic patients (JDDM 11). Diabetes Res Clin Pract 2008; 79: 171–6
Joshi SR, Kalra S, Badgandi M, et al. Designer insulins regimens in clinical practice: pilot multicenter Indian study. J Assoc Physicians India 2005; 53: 775–9
Kalra S, Plata-Que T, Kumar D, et al. Initiation with once-daily BIAsp 30 results in superior outcome compared to insulin glargine in Asians with type 2 diabetes inadequately controlled by oral anti-diabetic drugs. Diabetes Res Clin Pract 2010; 88: 282–8
Kvapil M, Swatko A, Hilberg C, et al. Biphasic insulin aspart 30 plus metformin: an effective combination in type 2 diabetes. Diabetes Obes Metab 2006; 8: 39–48
Levit S, Toledano Y, Wainstein J. Improved glycaemic control with reduced hypoglycaemic episodes and without weight gain using long-term modern premixed insulins in type 2 diabetes. Int J Clin Pract 2011; 65: 165–71
Lund SS, Tarnow L, Frandsen M, et al. Combining insulin with metformin or an insulin secretagogue in non-obese patients with type 2 diabetes: 12 month, randomised, double blind trial. BMJ 2009; 339: b4324
Nauck MA, Duran S, Kim D, et al. A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study. Diabetologia 2007; 50: 259–67
Raz I, Mouritzen U, Vaz J, et al. Addition of biphasic insulin aspart 30 to rosiglitazone in type 2 diabetes mellitus that is poorly controlled with glibenclamide monotherapy. Clin Ther 2003; 25: 3109–23
Raz I, Stranks S, Filipczak R, et al. Efficacy and safety of biphasic insulin aspart 30 combined with pioglitazone in type 2 diabetes poorly controlled on glibenclamide (glyburide) monotherapy or combination therapy: an 18-week, randomized, open-label study. Clin Ther 2005; 27: 1432–43
Ushakova O, Sokolovskaya V, Morozova A, et al. Comparison of biphasic insulin aspart 30 given three times daily or twice daily in combination with metformin versus oral antidiabetic drugs alone in patients with poorly controlled type 2 diabetes: a 16-week, randomized, open-label, parallel-group trial conducted in Russia. Clin Ther 2007; 29: 2374–84
Yang W, Ji Q, Zhu D, et al. Biphasic insulin aspart 30 three times daily is more effective than a twice-daily regimen, without increasing hypoglycemia, in Chinese subjects with type 2 diabetes inadequately controlled on oral antidiabetes drugs. Diabetes Care 2008; 31: 852–6
Yang WY, Ji QH, Zhu DL, et al. Thrice-daily biphasic insulin aspart 30 may be another therapeutic option for Chinese patients with type 2 diabetes inadequately controlled with oral antidiabetic agents. Chin Med J (Engl) 2009; 122: 1704–8
Raskin PR, Hollander PA, Lewin A, et al., on behalf of the INITIATE Study Group. Basal insulin or premix analogue therapy in type 2 diabetes patients. Eur J Intern Med 2007; 18: 56–62
Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab 2006; 8: 58–66
Hosoi Y, Ohtani K, Shimizu H, et al. Attainment of glycaemic goals by step-up therapy with biphasic insulin aspart-70/30 in Japanese type 2 diabetic patients. Endocr J 2011; 58: 131–5
Yoshioka N, Kurihara Y, Manda N, et al. Step-up therapy with biphasic insulin aspart-70/30: Sapporo 1-2-3 study. Diabetes Res Clin Pract 2009; 85: 47–52
Bergenstal R, Lewin A, Bailey T, et al., on behalf of the NovoLog Mix-vs.-Exenatide Study Group. Efficacy and safety of biphasic insulin aspart 70/30 versus exenatide in subjects with type 2 diabetes failing to achieve glycemic control with metformin and a sulfonylurea. Curr Med Res Opin 2009; 25: 65–75
Home PD. Comment on: Nauck MA, Duran S, Kim D, et al. (2007). A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study. Diabetologia 2007; 50: 1561–2; author reply 1563-4
Unnikrishnan AG, Tibaldi J, Hadley-Brown M, et al. Practical guidance on intensification of insulin therapy with BIAsp 30: a consensus statement. Int J Clin Pract 2009; 63: 1571–7
Lindholm A, Jensen LB, Home PD, et al. Immune responses to insulin aspart and biphasic insulin aspart in people with type 1 and type 2 diabetes. Diabetes Care 2002; 25: 876–82
Chen JW, Frystyk J, Lauritzen T, et al. Impact of insulin antibodies on insulin aspart pharmacokinetics and pharmacodynamics after 12-week treatment with multiple daily injections of biphasic insulin aspart 30 in patients with type 1 diabetes. Eur J Endocrinol 2005; 153: 907–13
Ligthelm RJ, Borzì V, Gumprecht J, et al. Importance of observational studies in clinical practice. Clin Ther 2007; 29: 1284–92
Ligthelm RJ. Insulin analogues: how observational studies provide key insights into management of patients with type 2 diabetes mellitus. Curr Med Res Opin 2011; 27: 2343–55
Kawamori R, Valensi P. IMPROVE™ observational study of biphasic insulin Aspart 30/70 in patients with type 2 diabetes mellitus. Expert Rev Endocrinol Metab 2010; 5: 507–16
Valensi P, Benroubi M, Borzi V, et al., on behalf of the IMPROVE Study Group Expert Panel. Initiating insulin therapy with, or switching existing insulin therapy to, biphasic insulin aspart 30/70 (NovoMix 30) in routine care: safety and effectiveness in patients with type 2 diabetes in the IMPROVE observational study. Int J Clin Pract 2009; 63: 522–31
Gumprecht J, Benroubi M, Borzi V, et al., on behalf of the IMPROVE Study Group Expert Panel. Intensification to biphasic insulin aspart 30/70 (BIAsp 30, NovoMix 30) can improve glycaemic control in patients treated with basal insulins: a subgroup analysis of the IMPROVE observational study. Int J Clin Pract 2009; 63: 966–72
Shah S, Benroubi M, Borzi V, et al., on behalf of the IMPROVE Study Group Expert Panel. Safety and effectiveness of biphasic insulin aspart 30/70 (NovoMix 30) when switching from human premix insulin in patients with type 2 diabetes: subgroup analysis from the 6-month IMPROVE observational study. Int J Clin Pract 2009; 63: 574–82
Khutsoane D, Sharma SK, Almustafa M, et al., on behalf of the PRESENT Study Group. Biphasic insulin aspart 30 treatment improves glycaemic control in patients with type 2 diabetes in a clinical practice setting: experience from the PRESENT study. Diabetes Obes Metab 2008; 10: 212–22
Sharma SK, Al-Mustafa M, Oh SJ, et al. Biphasic insulin aspart 30 treatment in patients with type 2 diabetes poorly controlled on prior diabetes treatment: results from the PRESENT study. Curr Med Res Opin 2008; 24: 645–52
Güler S, Sharma SK, Almustafa M, et al. Improved glycaemic control with biphasic insulin Aspart 30 in type 2 diabetes patients failing oral antidiabetic drugs: PRESENT study results. Arch Drug Inf 2009; 2: 23–33
Jang HC, Guler S, Shestakova M, et al., on behalf of the PRESENT Study Group. When glycaemic targets can no longer be achieved with basal insulin in type 2 diabetes, can simple intensification with a modern premixed insulin help? Results from a subanalysis of the PRESENT study. Int J Clin Pract 2008; 62: 1013–8
Shestakova M, Sharma SK, Almustafa M, et al. Transferring type 2 diabetes patients with uncontrolled glycaemia from biphasic human insulin to biphasic insulin aspart 30: experiences from the PRESENT study. Curr Med Res Opin 2007; 23: 3209–14
Almustafa M, Yeo JP, Khutsoane D. Glycaemic control and hypoglycaemia in the PRESENT study. Diabetes Res Clin Pract 2008; 81 Suppl. 1: S10–5
Liebl A, Prager R, Binz K, et al., on behalf of the PREFER Study Group. Comparison of insulin analogue regimens in people with type 2 diabetes mellitus in the PREFER study: a randomized controlled trial. Diabetes Obes Metab 2009; 11: 45–52
Shah SN, Litwak L, Haddad J, et al. The A1chieve study: a 60000-person, global, prospective, observational study of basal, meal-time, and biphasic insulin analogs in daily clinical practice. Diabetes Res Clin Pract 2010; 88 Suppl. 1: S11–6
Home P, Naggar NE, Khamseh M, et al. An observational non-interventional study of people with diabetes beginning or changed to insulin analogue therapy in non-Western countries: the A1chieve study. Diabetes Res Clin Pract 2011; 94: 352–63
Jang HC, Lee SR, Vaz JA. Biphasic insulin aspart 30 in the treatment of elderly patients with type 2 diabetes: a subgroup analysis of the PRESENT Korea NovoMix study. Diabetes Obes Metab 2009; 11: 20–6
Sharma SK, Joshi SR, Kumar A, et al., on behalf of the PRESENT Study Group. Efficacy, safety and acceptability of biphasic insulin aspart 30 in Indian patients with type 2 diabetes: results from the PRESENT study. J Assoc Physicians India 2008; 56: 859–63
Gao Y, Guo XH, Vaz JA, on behalf of the PRESENT Study Group. Biphasic insulin aspart 30 treatment improves glycaemic control in patients with type 2 diabetes in a clinical practice setting: Chinese PRESENT study. Diabetes Obes Metab 2009; 11: 33–40
Shah S, Das AK, Kumar A, et al. Baseline characteristics of the Indian cohort from the IMPROVE study: a multinational, observational study of biphasic insulin aspart 30 treatment for type 2 diabetes. Adv Ther 2009; 26: 325–35
Gao Y, Guo XH. Switching from human insulin to biphasic insulin aspart 30 treatment gets more patients with type 2 diabetes to reach target glycosylated hemoglobin < 7%: the results from the China cohort of the PRESENT study. Chin Med J (Engl) 2010; 123: 1107–111
Giorda C, Boemi M, Borzì V, et al. The IMPROVE study: a multinational, multicentre, observational study in type 2 diabetes: results from the Italian cohort. Acta Biomed 2010; 81: 115–24
Esteghamati A, Rajabian R, Amini M, et al. The safety and efficacy of biphasic insulin aspart 30 (BIAsp 30) in Iranians with type 2 diabetes: an open-label, non-randomised, multicentre observational study. The Iran subgroup of the IMPROVE™ study. Endokrynol Pol 2010; 61: 364–70
Yang W, Gao Y, Liu G, et al. Biphasic insulin aspart 30 as insulin initiation or replacement therapy: the China cohort of the IMPROVE study. Curr Med Res Opin 2010; 26: 101–7
Breum L, Almdal T, Eiken P, et al., on behalf of the Danish BIAsp Study Group. Initiating or switching to biphasic insulin Aspart 30/70 therapy in subjects with type 2 diabetes mellitus: an observational study. Rev Diabet Stud 2008; 5: 154–62
Morgan CL, Evans M, Toft AD, et al. Clinical effectiveness of biphasic insulin aspart 30: 70 versus biphasic human insulin 30 in UK general clinical practice: a retrospective database study. Clin Ther 2011; 33: 27–35
Korytkowski M, Bell D, Jacobsen C, et al., on behalf of the FlexPen Study Team. A multicenter, randomized, open-label, comparative, two-period crossover trial of preference, efficacy, and safety profiles of a prefilled, disposable pen and conventional vial/syringe for insulin injection in patients with type 1 or 2 diabetes mellitus. Clin Ther 2003; 25: 2836–48
Pfutzner A, Reimer T, Frokjaer LPF, et al. Prefilled insulin device with reduced injection force: patient perception and accuracy. Curr Med Res Opin 2008; 24: 2545–9
Sommavilla B, Jørgensen C, Jensen K. Safety, simplicity and convenience of a modified prefilled insulin pen [published erratum appears in Expert Opin Pharmacother 2009; 10: 153]. Expert Opin Pharmacother 2008; 9: 2223–32
Palmer AJ, Roze S, Valentine WJ, et al. Validation of the CORE Diabetes Model against epidemiological and clinical studies. Curr Med Res Opin 2004; 20 Suppl. 1: S27–40
Ray JA, Valentine WJ, Roze S, et al. Insulin therapy in type 2 diabetes patients failing oral agents: cost-effectiveness of biphasic insulin aspart 70/30 vs. insulin glargine in the US. Diabetes Obes Metab 2007; 9: 103–13
Valentine WJ, Palmer AJ, Lammert M, et al. Long-term clinical and cost outcomes of treatment with biphasic insulin aspart 30/70 versus insulin glargine in insulin naïve type 2 diabetes patients: cost-effectiveness analysis in the UK setting. Curr Med Res Opin 2005; 21: 2063–71
Palmer JL, Beaudet A, White J, et al. Cost-effectiveness of biphasic insulin aspart versus insulin glargine in patients with type 2 diabetes in China. Adv Ther 2010; 27: 814–27
Goodall G, Jendle JH, Valentine WJ, et al. Biphasic insulin aspart 70/30 vs. insulin glargine in insulin naïve type 2 diabetes patients: modelling the long-term health economic implications in a Swedish setting. Int J Clin Pract 2008; 62: 869–76
Palmer JL, Knudsen MS, Aagren M, et al. Cost-effectiveness of switching to biphasic insulin aspart from human premix insulin in a US setting. J Med Econ 2010; 13: 212–20
Lee KH, Seo SJ, Smith-Palmer J, et al. Cost-effectiveness of switching to biphasic insulin aspart 30 from human insulin in patients with poorly controlled type 2 diabetes in South Korea. Value Health 2009; 12 Suppl. 3: S55–61
Ali M, White J, Lee CH, et al. Therapy conversion to biphasic insulin aspart 30 improves long-term outcomes and reduces the costs of type 2 diabetes in Saudi Arabia. J Med Econ 2008; 11: 651–70
Brod M, Cobden D, Lammert M, et al. Examining correlates of treatment satisfaction for injectable insulin in type 2 diabetes: lessons learned from a clinical trial comparing biphasic and basal analogues. Health Qual Life Outcomes 2007 Feb 7; 5: 8
Brod M, Valensi P, Shaban JA, et al. Patient treatment satisfaction after switching to NovoMix® 30 (BIAsp 30) in the IMPROVE™ study: an analysis of the influence of prior and current treatment factors. Qual Life Res 2010; 19: 1285–93
Mukherjee AK, Reddy VS, Shah S, et al. Quality of life as a key indicator of patient satisfaction and treatment compliance in people with type 2 diabetes mellitus in the IMPROVE study: a multicentre, open label, non-randomised, observational trial. J Indian Med Assoc 2009; 107: 464–70
Ishii H, Iwase M, Seino H, et al. Assessment of quality of life in patients with type 2 diabetes mellitus before and after starting biphasic insulin aspart 30 (BIAsp 30) therapy: IMPROVE study in Japan. Curr Med Res Opin 2011; 27: 643–50
Ligthelm RJ. Self-titration of biphasic insulin aspart 30/70 improves glycaemic control and allows easy intensification in a Dutch clinical practice. Prim Care Diabetes 2009; 3: 97–102
Oyer DS, Shepherd MD, Coulter FC, et al., on behalf of the INITIATEplus Study Group. A(1c) control in a primary care setting: self-titrating an insulin analog pre-mix (INITIATEplus trial). Am J Med 2009; 122: 1043–9
Acknowledgements
The authors accept direct responsibility for this paper and are grateful for the contribution made by Michael Lappin of Watermeadow Medical, Witney, UK (supported by Novo Nordisk A/S, Bagsvaerd, Denmark) in developing the draft manuscript from an agreed outline, and in collating comments.
AL has received consultancy and lecture fees from Novo Nordisk. VP is an employee of Novo Nordisk. PV served as Principal Investigator in the IMPROVE study and has given lectures for, and his department has received a grant from, Novo Nordisk. RK and JSC have no conflicts of interest to declare. AP has received consulting fees and travel expenses from Novo Nordisk. PB is an employee of Novo Nordisk A/S, with share options, and inventor of the patent covering the NovoMix® preparation. RL has been a member of Advisory Boards for Novo-Nordisk, Eli-Lilly, Sanofi and others outside the diabetes sphere. He is on the speakers’ bureaus for Novo Nordisk and GlaxoSmithKline and has been involved in both RCTs and observational studies for Novo Nordisk. He has never received grants from Novo Nordisk. VM has received research grants and honoraria from Novo Nordisk, Sanofi, MSD, Johnson & Johnson and Lilly, and lecture fees from Novo Nordisk.
All authors approved the review strategy and, where appropriate, provided input on additional references that warranted inclusion. All authors made substantive comments on the initial outline, on later drafts of the review, and approved the final version prior to submission.
The writing of this review article was supported by Novo Nordisk A/S, Bagsvaerd, Denmark, which reviewed the outline and drafts for medical accuracy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Liebl, A., Prusty, V., Valensi, P. et al. Ten Years of Experience with Biphasic Insulin Aspart 30. Drugs 72, 1495–1520 (2012). https://doi.org/10.2165/11635490-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11635490-000000000-00000