Abstract
Background: There are concerns that automated drug dispensing may increase inappropriate drug use. Automated dispensing could lead to perpetual repeating of drug therapies without the necessary re-evaluation.
Objectives: The aim of this study was to examine the effect of a pharmacist-led medication review on drug-related problems (DRPs) in older patients receiving their drugs via automated dispensing.
Methods: This was a pragmatic randomized controlled study conducted in primary care. Patients were recruited from six Dutch community pharmacies. They were eligible if they lived at home, were aged ≥65 years, and used five or more different drugs, of which at least one had to be dispensed via an automated system. Patients were randomly allocated to receive a medication review at the start of the study (intervention group) or after 6 months (waiting-list group). Each patient was independently reviewed by two pharmacist reviewers. The results of these medication reviews were sent to the community pharmacist to be discussed with the patient’s general practitioner (GP). The primary outcome measure was the number of DRPs leading to a recommendation for drug change. Secondary outcomes were the total number of drug changes and the number of drug changes related to a recommendation. In order to analyse drug changes, medication records were collected 6 months after the medication review or index date in the waiting-list group. Potential DRPs were classified using the DOCUMENT classification.
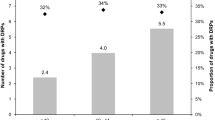
Results: There were no baseline differences between the 63 patients in the intervention group and the 55 patients in the waiting-list group with respect to age, sex, number of drugs per patient and type of drug prescribed. The mean number of DRPs per patient at baseline in the intervention group and waiting list combined was 8.5, with no difference between the groups. At baseline, the mean number of DRPs leading to a recommendation for drug change was 4.5 per patient and did not differ between the two groups. After 6 months, the number of DRPs leading to a recommendation for drug change decreased by 29% in the intervention group versus 5% in the waiting-list group (p < 0.01). Recommendations for cessation of a drug were more frequently accepted than recommendations to add a new drug (82% vs 44%, p = 0.01).
Conclusions: This study shows that patients using automated drug dispensing have a high number of DRPs. Medication review decreases the number of DRPs among these patients. We recommend that all patients with automatic drug dispensing should have a thorough medication review by pharmacists and prescribers.




Similar content being viewed by others
References
Kongkaew C, Noyce PR, Ashcroft DM. Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother 2008; 42: 1017–25
Leendertse AJ, Egberts AC, Stoker LJ, et al. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med 2008; 168: 1890–6
Beijer HM, Blaey CJD. Hospitalisations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm World Sci 2002; 25: 46–54
Howard RL, Avery AJ, Slavenburg S, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol 2007; 63: 136–47
De Smet PA. Hospital admissions related to medications and implementing guidelines. Arch Intern Med 2009; 169: 810–1
Johnell K, Fastbom J. Multi-dose drug dispensing and inappropriate drug use: a nationwide register-based study of over 700,000 elderly. Scand J Prim Health Care 2008; 26: 86–91
Gould ON, Todd L, Irvine-Meek J. Adherence devices in a community sample: how are pillboxes used? Can Pharm J 2009; 142: 28–35
Larsen AB, Haugbolle LS. The impact of an automated dose-dispensing scheme on user compliance, medication understanding, and medication stockpiles. Res Social Adm Pharm 2007; 3: 265–84
van den Bemt PM, Idzinga JC, Robertz H, et al. Medication administration errors in nursing homes using an automated medication dispensing system. J Am Med Inform Assoc 2009; 16: 486–92
Bell JS, Vaananen M, Ovaskainen H, et al. Providing patient care in community pharmacies: practice and research in Finland. Ann Pharmacother 2007; 41: 1039–46
Krska J, Avery AJ, Community Pharmacy Medicines Management Project Evaluation Team. Evaluation of medication reviews conducted by community pharmacists: a quantitative analysis of documented issues and recommendations. Br J Clin Pharmacol 2008; 65: 386–96
Cipolle RJ. Pharmaceutical care practice: the clinician’s guide. 2nd ed. New York, London: McGraw-Hill, Medical Pub. Division, 2004
Peterson G, Tenni P. Identifying, prioritizing and documenting drug-related problems. Aust Pharm 2004; 23(10): 706–9
Tenni P, Stafford A, Peterson G, et al. A comparison of drug-related problems identified in RMMRs and HMRs. Aust Pharm 2007; 26: 414–20
Rasmussen M, Stafford AC, Tenni PC, et al. Drug-related problems identified in medication reviews by Australian pharmacists. Pharm World Sci 2009; 31: 216–23
van Mil JW, Westerlund LO, Hersberger KE, et al. Drugrelated problem classification systems. Ann Pharmacother 2004; 38: 859–67
Krska J, Cromarty JA, Arris F, et al. Pharmacist-led medication review in patients over 65: a randomized, controlled trial in primary care. Age Ageing 2001; 30: 205–11
Denneboom W, Dautzenberg MG, Grol R, et al. Treatment reviews of older people on polypharmacy in primary care: cluster controlled trial comparing two approaches. Br J Gen Pract 2007; 57: 723–31
Vinks TH, Egberts TC, de Lange TM, et al. Pharmacist-based medication review reduces potential drug-related problems in the elderly: the SMOG controlled trial. Drugs Aging 2009; 26(2): 123–33
Sorensen L, Stokes JA, Purdie DM, et al. Medication reviews in the community: results of a randomized, controlled effectiveness trial. Br J Clin Pharmacol 2004; 58: 648–64
Mörlin C, Gillespie U, Alassaad A, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med 2009; 169: 894–900
Sellors J, Kaczorowski J, Sellors C, et al. A randomized controlled trial of a pharmacist consultation program for family physicians and their elderly patients. CMAJ 2003; 169: 17–22
Zermansky AG, Alldred DP, Petty DR, et al. Clinical medication review by a pharmacist of elderly people living in care homes: randomised controlled trial. Age Ageing 2006; 35: 586–91
Almeida Neto AC, Chen TF. Exploring elements of interprofessional collaboration between pharmacists and physicians in medication review. Pharm World Sci 2007; 29: 574–6
Knottnerus JA, Muijrers PEM, Grol RPTM, et al. Pharmaceutical care and its relationship to prescribing behaviour of general practitioners. Pharm World Sci 2006; 28: 302–8
Muijrers PE, Grol RP, Sijbrandij J, et al. Differences in prescribing between GPs: impact of the cooperation with pharmacists and impact of visits from pharmaceutical industry representatives. Fam Pract 2005; 22: 624–30
Niquille A, Lattman C, Bugnon O. Medication reviews led by community pharmacists in Switzerland: a qualitative survey to evaluate barriers and facilitators. Pharm Pract 2010; 8: 35–42
Klarin I, Wimo A, Fastbom J. The association of inappropriate drug use with hospitalisation and mortality: a population-based study of the very old. Drugs Aging 2005; 22: 69–82
Holland R, Lenaghan E, Harvey I, et al. Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ 2005; 330: 293
Zermansky AG, Petty DR, Raynor DK, et al. Randomised controlled trial of clinical medication review by a pharmacist of elderly patients receiving repeat prescriptions in general practice. BMJ 2001; 323: 1340–3
RESPECT Trial Team. Effectiveness of shared pharmaceutical care for older patients: RESPECT trial findings. Br J Gen Pract 2010; 60: e10–9
Niquille A, Bugnon O. Relationship between drug-related problems and health outcomes: a cross-sectional study among cardiovascular patients. Pharm World Sci 2010; 32: 512–9
Clyne W, Blenkinsopp A, Seal R. A guide to medication review, 2008. National Prescribing Centre [online]. Available from URL: http://www.npci.org.uk/medicines_management/review/medireview/library/library_good_practice_guide1.php [Accessed 2010 Apr 19]
Acknowledgements
This study was funded by Apotheek Voorzorg, a provider of automated drug dispensing systems, and the Royal Dutch Association for the Advancement of Pharmacy (KNMP). This work was performed totally independently from these funders.
The authors thank all the participating community pharmacies, the pharmacist reviewers J.M. Krijger-Dijkema and H. Buurma, and D. Titre for her contribution to the data classification. The authors also wish to thank Dr Peterson and colleagues, University of Tasmania, Australia, for their permission to include the adapted version of their DOCUMENT classification system in the Supplemental Digital Content that accompanies this article.
All authors declare that they have no conflict of interests that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kwint, HF., Faber, A., Gussekloo, J. et al. Effects of Medication Review on Drug-Related Problems in Patients Using Automated Drug-Dispensing Systems. Drugs Aging 28, 305–314 (2011). https://doi.org/10.2165/11586850-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11586850-000000000-00000